Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Case Report of a Rare Cause of Postoperative Transient Tetraparesis after Epidural Catheter Placement
*Corresponding author: Christian Vetter, Inselspital, Bern University Hospital, Department of Anesthesiology and Pain Medicine, Freiburgstrasse.
Received: August 19, 2021; Published: October 18, 2021
DOI: 10.34297/AJBSR.2021.14.002002
Introduction
Epidural anesthesia in combination with general anesthesia is a standard procedure for major visceral surgery [1-3]. Severe complications of epidural anesthesia are rare, but there is a risk of epidural hematomas, which can cause spinal cord compression [4]. Incidence rates differ in specific perioperative patient populations [5]. In general, this complication is excluded by computed tomography (CT) or magnetic resonance imaging (MRI) [6]. In the literature, the rate of complications related to epidural anesthesia ranges from < 10% for transient paresthesia to 0.0006% for epidural hematomas with signs of compression [6].
Case study
We report on a 73-year-old patient who underwent Whipple surgery for proven pancreatic cancer (histology: moderately differentiated ductal adenocarcinoma of the pancreatic head). In addition to standard monitoring, which included invasive blood pressure monitoring and placement of a central venous line in the internal jugular vein, an epidural catheter was inserted at the level of Th 6/7 under local anesthesia for postoperative pain management. The operation itself was uneventful, and the patient was extubated a few minutes after surgery ended. Immediately after extubation, the patient showed signs of postoperative delirium, which was treated with dexmedetomidine. A neurological examination revealed significant symmetrical force reduction (M3) of the upper extremities and paraplegia of the lower extremities, both of which did not exist prior to the induction of anesthesia.
Although the epidural catheter had been placed without any complications, we promptly performed an MRI examination of the thoracic and cervical spine to rule out traumatic and non-traumatic tetra paresis [4]. The whole spine was examined with the addition of MRI diffusion, and we were able to exclude an epidural hematoma. The tip of the epidural catheter was located at the neuroforamina T6. But we were surprised to find complete spinal canal stenosis at the level of C4-C6, with signs of chronic vascular damage in the area to the right sulcocommissural artery at the level of C4-C5.
By the end of the MRI examination, the patient was able to move his arms without any restrictions (force M5), and the paresis of the lower extremities was clearly decreasing (force M2). About two hours after extubation, the force in the lower and upper extremities was fully restored (M5). The further postoperative course was aggravated by delirium persisting over several days. Apart from the persistent delirium, no further neurological problems were registered, and the patient recovered completely during his hospitalization. Later, the patient received adjuvant chemotherapy. Since the patient did not show any neurological symptoms in everyday life, surgical therapy of the spinal canal stenosis was not performed.
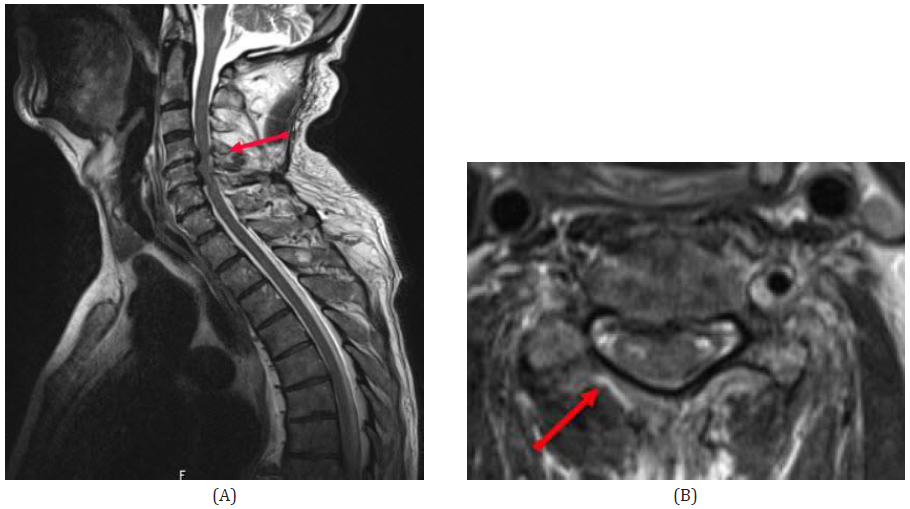
Figure 1A+B: The sagittal T2-weighted (Fig.1a) and the axial T2-weighted (Fig.1b) MR scans of the cervical spine revealed absolute combined osseous and absolute discogenic spinal canal stenosis at the level of the cervical vertebra 4 to the cervical vertebra 6, with signs of chronic cervical myelopathy in the vascular territory of the right sulcocommissural artery at level C4/5.
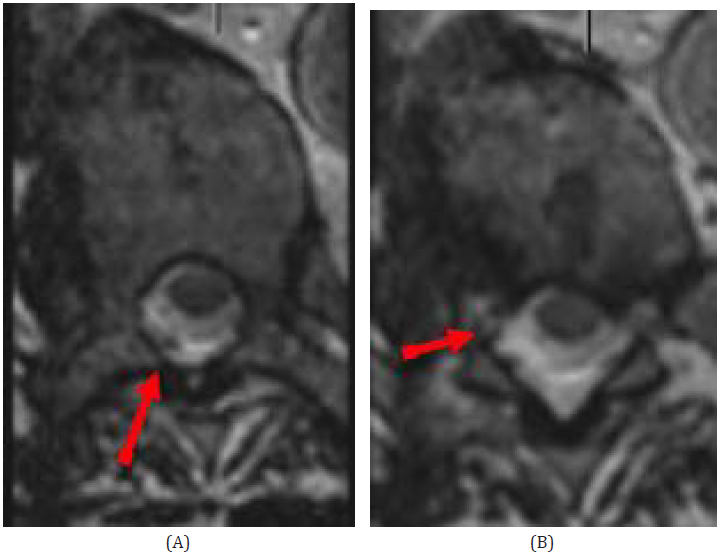
Figure 2A+B: The axial T2-weighted SPACE showed the epidural catheter with epidural entry at thoracic vertebra level 7 (Fig. 2a) and ascending course on the right side to the level of the right neuroforamen of T6, with localization of the catheter tip just at the entry of the right neuroforamen of the right T6.
Discussion
For extensive surgical procedures, combined general and epidural anesthesia is now widely used, and has become the preferred technique [1-3]. Severe complications of epidural anesthesia are rare, but if a patient displays new neurological symptoms, complications after epidural catheter placement must be promptly evaluated to prevent serious neurological sequelae. In a 2021 publication, Oliveira et al. listed differential diagnosessuch as stroke, myasthenia gravis, severe hypokalemia, and spinal cord compression-that can be ruled out with an emergency imaging procedure (CT or MRI scan) or blood gas analysis [4,7-11].
In our case, hypotension could have exacerbated the cause of chronic myelopathy, leading to a reduction in supply of the spinal cord [13]. However, the patient received invasive monitoring prior to the start of surgery, and hypotension (>20% of baseline blood pressure [7]) was promptly treated with administration of vasopressors. The duration of the operation, performed over six hours with the patient in the same supine position, could have been a trigger for this transient event [12]. Preoperatively, the patient reported no neurological complaints. Despite placement of an epidural catheter, we decided to perform an emergency MRI immediately after the operation, in order to rule out a cervical cord lesion. The MRI scan showed complete spinal stenosis in the vascular territory of the right sulcocommissural artery at level C4/5. Other potential causes, as described above, were not followed up since the patient’s symptoms steadily improved. Also, transient hypotension does not immediately lead to signs of chronic damage of the myelon, so we consider this possibility rather unlikely in this context.
We believe spinal stenosis in the vascular territory of the right sulcocommissural artery at level C4/5, caused by the patient’s position during the operation, was the most probable cause of the transient tetra paresis after Whipple’s surgery
Conclusion
Neurological complications occurring after epidural catheter placement must be immediately subjected to diagnostic and/or therapeutic procedures. The case we describe shows that even rare findings can lead to tetra paresis. After exclusion of acute mechanical spinal cord compression by MRI scan, we believe that chronic vascular damage was the cause of our patient’s transient tetra paresis.
The patient and his family consented to our publication of the case.
References
- Lesley De Pietri, Roberto Montalti, Bruno Begliomini (2014) Anaesthetic perioperative management of patients with pancreatic cancer. World J Gastroenterol 20(9): 2304-2320.
- Clemente A, Carli F (2008) The physiological effects of thoracic epidural anesthesia and analgesia on the cardiovascular, respiratory, and gastrointestinal systems. Minerva Anestesiol 74(10): 549-563.
- Nan Li, Hao Kong, Shuang Ling Li, Sai Nan Zhu, Dong Xin Wang (2018) Combined epidural-general anesthesia was associated with lower risk of postoperative complications in patients undergoing open abdominal surgery for pheochromocytoma: A retrospective cohort study. PLoS ONE 13(2): e0192924.
- Oliveira R, Rocha FR, Teodoro T, Santos MO (2021) Acute non-traumatic tetraparesis: differential diagnosis. J Clin Neurosci 87:116-124.
- Bos E, Hollmann M, Lirk P (2017) Safety and efficacy of epidural analgesia. Curr Opin Anaesthesiol 30(6): 736-742.
- Mariano R, Flanagan EP, Weinshenker BG, Palace J (2018) A practical approach to the diagnosis of spinal cord lesions. Pract Neurol 18(3):187–200.
- Moraca RJ, Sheldon DG, Thirlby R (2003) The role of epidural anesthesia and analgesia in surgical practice. Ann Surg 238(5): 663-673.
- Vafi Salmasi, Kamal Maheshwari, Dongsheng Yang, Edward J Mascha, Asha Singh, et al. (2017) Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology 126(1): 47-65.
- Sadanand V, Kelly M, Varughese G, Fourney DR (2005) Sudden quadriplegia after acute cervical disc herniation. Can J Neurol Sci 32:356-358.
- Wyndaele M, Wyndaele JJ (2006) Incidence, prevalence, and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 44: 523-529.
- Caplan LR (2009) Caplan’s stroke: a clinical approach. 4th edition. Elsevier/Saunders.
- David JW Knight, MRCP FRCA, Ravi P Mahajan, DM FRCA (2004) Patient positioning in anaesthesia. Contin Educ Anaesth Crit Care Pain, 4(5): 160-163.
- Drummond JC, Lee RR, Owens EL (2012) Spinal cord ischemia occurring in association with induced hypotension for colonic surgery. Anesth Analg 114(6):1297-1300.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.