Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Feasibility of Adopting Telemedicine Abortion (TMA) Care to Improve Access to Quality Abortion Services in Kenya: A Systematic Review
*Corresponding author: Masoud Mohammadnezhad. Faculty of Health, Education and Life Sciences, School of Nursing and Midwifery, Birmingham City University, Birmingham, UK.
Received: July 02, 2024; Published: July 09, 2024
DOI: 10.34297/AJBSR.2024.23.003052
Abstract
Background: Unsafe abortion accounts for one of the leading causes of maternal deaths in Kenya. Access to safe abortion has been bombarded by the restrictive factors such as legal, economic, and social aspects thus denying the eligible group their universal right of quality healthcare. This study explored the feasibility of implementing Telemedicine Abortion (TMA) to improve accessibility of safe abortion care services based on safety, effectiveness, acceptability, and accessibility.
Methodology: This study applied a systematic review approach. The following electronic databases were searched; Cochrane Library, CINHAL plus, Embase, Scopus Medline studies for the articles published between 2012 up until 2024. Abstracts and articles were subjected to double screening and data extracted using Data Extraction Form (DEF) following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Thematic analysis was carried out using Atlas.ti software. Mixed Methods Appraisal Tool was adopted to determine the quality of selected articles.
Results: Out of 2147 articles searched, 44 papers met the inclusion criteria. Most papers originated from the developed countries such as United States, United Kingdom, and Australia. The following themes emerged, safety of Telemedicine Abortion, effectiveness of Telemedicine Abortion, acceptability of Telemedicine Abortion and Access through Telemedicine Abortion. Most studies reported high patient satisfaction and increased access. Also, TMA was found to be highly effective with no deaths and an insignificant proportion of complications reported.
Conclusion: Telemedicine Abortion is safe, acceptable and improves access to abortion care services. This study recommends further research on tackling health inequalities linked to telemedicine abortion.
Keywords: Telemedicine abortion, Patient acceptability, Safety, effectiveness, Feasibility, Systematic review study, Kenya
Introduction
Global statistics indicate that by estimate, 35 out of 1000 women between the ages 15-44 have access to safe abortion care services [1]. World Health Organisation (WHO) recommendations allow for outpatient provision of abortion care services during the first trimester by mid-level care providers. In addition, eligible women can access abortion services at home through self-administration of abortion medication and be able to assess the completeness of abortion, following the standard guidelines of medication abortion [1]. Besides being a popular obstetric event and a crucial component of Sexual and Reproductive Health (SRH), several women still face myriads of challenges in accessing safe abortion care services in Low- and Middle-Income Countries (LMICs) such as social, economic, cultural, technological, and legal factors. These access barriers pose a risk to women’s health worldwide. While safe abortion is associated with negligible deaths and rare adverse events, unsafe abortion is reported to cause an estimate of 23 000 deaths annually on a global scale [2]. Africa leads with 76% of unsafe abortions due to access barriers, and in Kenya, the cost of treating cases of unsafe abortions is estimated at $6.3 million every year, hence projecting the high incidence of unsafe abortion cases in the country [3]. The abortion rate is estimated to be 48 per 1000 women [4]. Sing et al [5] alludes that mortalities and morbidities due to unsafe abortion are common in Kenya. The cohort with high incidence of unsafe abortion is women aged between 15-24 years, who face access barriers such as social stigma, legal constraints, shortage of healthcare facilities and providers and inadequate information on sexual and reproductive health [6].
Kenya being part of the Low-and Middle-Income Countries (LMICs) faces severe constraints of healthcare access inequities. These conundrums include inadequate healthcare workers, constrained health budgets, poor healthcare leadership and low uptake of digital healthcare. Research shows that most teenage pregnancies are intended in the LMICs due to early marriages and socioeconomic prospects. It further indicates that teenagers ranging from 15-19 have higher risk of death due to pregnancy than those from 20–24 years old [1]. Also, limited access to SRH services such as contraception and sexuality education have led to unintended pregnancies as well us untimely access to safe abortion care services, thus compelling the young adolescents to give birth, against their choice [7]. According to the Constitution of Kenya, abortion is only legal under certain circumstances such as need for emergency care, or if the health or life of the mother is at stake or otherwise in danger. This is confusing to most women as shown in research, since most women do not comprehend the legal framework of undertaking abortion [8]. In addition, the duress from anti-abortion groups have further propagated the confusion on the perceived immorality of abortion and resulted in the withdrawal of safe abortion guidelines from the Kenyan Ministry of health, which were in place [3]. As a result, high incidence of unsafe abortion cases has been witnessed due to stigma and fear instigated amongst eligible women, thus leading to severe complications of unsafe abortion, contributing to preventable maternal deaths. This calls for rapid and responsive approaches to boost access to safe abortion care services [7]. Telemedicine, which refers to assessment and treatment of patients remotely through utilization of telecommunication technologies, aids in provision of medical services through electronic exchange of medical data and health education services[9]. Garvin, et al., [10] notes that optimal utilization of telemedicine has the potential to utterly increase health care access to large number of people across the globe, and in the context of abortion care, telemedicine has the potential to increase access to safe abortion care services. Medication abortion integrates easily with telemedicine since patients do not require direct observations when taking their medications. The process of medication abortion entails determining eligibility criteria for medication abortion, obtaining informed consent, taking medication abortion drugs simultaneously starting with mifepristone, followed by misoprostol, and establishing follow-up to assess completion of abortion. Integrating telemedicine into medication abortion has simplified and de-medicalized the process of abortion It also shows that women facing access barriers such as legal and cost constraints value Telemedicine Abortion [11].
Although some studies report the unpopular use of telemedicine in provision of healthcare services in Kenya, the existence of a robust digital architecture provides a platform for adopting telemedicine in the delivery of healthcare services. Kenya is at the frontier in embracing technology, having laid a robust Information and Communication Technologies (ICT) infrastructure to allow for digitization of healthcare services [9]. For instance, Digital Health Act, 2023 was recently enacted with the aim of strengthening health service provision in Kenya and is backed by Data Protection Regulations, 2021 which ensures privacy and confidentiality of personal data [12]. Therefore, the existing ICT infrastructure lays a foundation for adoption of Telemedicine Abortion (TMA) which leads to improved access to abortion care services. Adoption of telemedicine abortion will create a platform to widen the access of abortion care services through utilisation of numerous digital health technologies and break the access barriers. This systematic literature review sought to explore the feasibility of adopting TMA to boost accessibility of safe abortion care services in Kenya amongst the eligible women. The study’s outcomes were aligned to the safety, acceptability by eligible women, and effectiveness of telemedicine on safe abortion. Effectiveness was measured by completeness of abortion, safety by measure of complications related to abortion that poses a risk to a woman’s physical health, and acceptability by woman’s perception of using telemedicine for abortion care services [13].
Methodology
Study Design
A systematic review was adopted to synthesis primary and secondary research papers on the utilization of telemedicine in healthcare setups using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14]. Due to rapid and dynamic use of technology in healthcare, with the shifting state of healthcare systems, it was plausible to explore possible outcomes of embracing technology in delivery of specific healthcare services in primary care settings. A systematic review study was chosen as the apt method to widen the search for variety of research thus enhancing quality evidence to build on the existing knowledge. This method summarizes research from a series of levels, combining divergent interventions, populations, and settings in a manner that enhances coherence [14]. Access to safe abortion is defined as using telemedicine as set of services provided throughout the course of abortion care which include assessment and counselling, guidelines on medication, abortion medication, follow up, exchange of information either verbal or written between the healthcare provider and the eligible woman. The author discusses provision of safe abortion services using telemedicine against the medical abortion provided in-person, either in clinic or any other setup without utilization of telemedicine.
Search Strategy
The following databases are searched to review the existing literature; Cochrane Library, CINHAL plus, Embase, Scopus Medline studies. The databases were chosen due to their popular use in many systematic review studies as well as their accessibility. Medical Subject Heading (MeSH) was used as search construct for the index terms. Boolean Search operators (AND, OR) were adopted to sift through the keywords relevant to study title. The key terms used for the search included “telemedicine”, “telemedicine abortion”, “medication abortion ”, “safety”, “effectiveness”, “medication abortion”, “acceptability”, “access”, “feasibility”, “Kenya”, “Low- and Middle-Income Countries”.
Inclusion and Exclusion Criteria
The inclusion and exclusion of studies followed the Population, Intervention, Comparator, Outcome and Setting (PICOS) format that is shown in Table 1.
Selection Process
The selected studies were exported to End-Note platform and duplications titles removed. Then, the remained studies’ titles were scanned, and irrelevant titles were omitted. Abstracts with results illustrating the acceptability for eligible women and healthcare providers, safety, and effectiveness of using telemedicine to improve access to safe abortion, with adherence to stipulated standard regimens for abortion treatment were reviewed. Finally, the full text of the remaining studies was printed and read for more information. The bibliography of studies also checked to find other articles that were not available in the searched databases.
Data Extraction
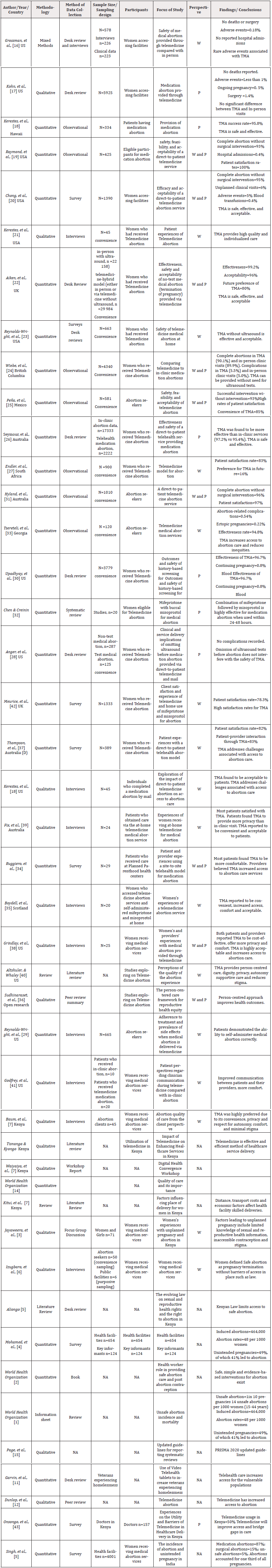
Online data collection was conducted with the use of Data Extraction Form (DEF) and exported into excel spreadsheet. DEF enhanced consistent retrieval and organization of relevant study contents for variety of articles selected before analysis (Table 2).
Critical Appraisal
The Mixed Methods Appraisal (MMAT) Tool was used to appraise study designs of various articles such as quantitative, qualitative, or mixed methods approach. The rationale behind the selection of MMAT tool was due to selection of research with different study designs, besides being a popular tool used by many researchers. The researcher put greater emphasis on studies ranging between 50% and 100% and less on those that scored below 50%. Individual articles were reviewed, and quality determined by the author. The score of each article was based on the degree of conformity to criteria. The categories were ranked as high quality for articles that met all or most of criteria, good quality for those that conformed to many fields of criteria and poor quality for papers that met few criteria. Table 3 and Table 4 illustrate the scoring criteria for quantitative and qualitative studies respectively.
Synthesis the Results
ATLAS.ti software was used to perform thematic analysis which entailed coding of definitions, descriptions, and statements linked to telemedicine medical abortion and further categorized into themes accordingly. The codes reflected the most recurrent statements or quotations from each category. Codes that depicted common explanation were put together to develop sub-themes, followed by final merger of list of codes to form themes.
Results
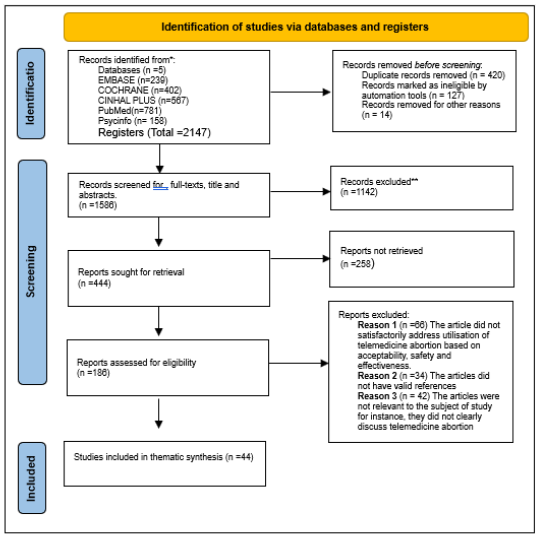
A total of 5 databases were searched which yielded a total of 2147 articles as the initial search. 420 duplicate records and 141 articles deemed ineligible by automation tools were removed before screening. 1586 articles were eligible for screening for full-texts, titles, and abstracts, which led to exclusion of 1142 articles. Upon retrieval, 186 articles were assessed for eligibility, excluding 142 studies. Finally, 44 studies were considered for this study (Figure 1).
Forty-four studies were included for the study which constituted 16 qualitative studies and 27 quantitative studies. Qualitative data collection methods involved interviews and focused group discussions whereas quantitative articles were mainly surveys and experimental studies. The papers included originated from USA (19), UK (4), South Africa (1), Hawaii (1), Australia (4), Scotland (1), Kenya (6), Mexico (1), British Columbia (1). Four themes emerged from the thematic synthesis which included safety of TMA, Effectiveness of TMA, Acceptability of TMA, and Access through TMA. Figure 1 illustrates the steps for selection of articles for inclusion.
Theme 1: Safety of Telemedicine Abortion
After assessing the selected research articles, three components emerged on the safety of TMA namely: complications, infections, and blood transfusion rates. Many studies reported less significant complications linked to TMA, constituting no deaths [15-26]. In examining the likelihood of ectopic pregnancy, Aiken et al [21] and Anger, et al., [27] reported comparisons of two groups: test and non-test groups. one study indicated no occurrence of ectopic pregnancy at all between the two groups [17] whereas another one [28] reported an insignificant proportion of patients experiencing ectopic pregnancy and required postabortion care management at a healthcare facility setup in non-test group. However, it further ascertained the emergence of minor complications that were resolved through use of various telecommunication channels between the provider and the clients, thus reducing the need for in-person visits to healthcare facility. Several studies reported low rates of blood transfusion being less than 1% [15-17,19,26,28-29]. Two studies found the infection rates to be significantly low [24,25].
Theme 2: Effectiveness of Telemedicine Abortion
To determine its effectiveness, three components of TMA namely complete abortion, continuing pregnancy and surgical intervention were scrutinized. All studies described TMA to be effective, reporting complete abortion rates to be high and less of surgical interventions [18-20,24-26,30,31]. Gestational age was a factor in determining the effectiveness of TMA, with pregnancies less than 70 days of gestational age linked with high chances of complete abortion of up to 98%, with minimal chances of continuing pregnancy [21,20,24,25,27,30,32] and surgical intervention [18-20,24,25,29,32]. In comparing these findings to the medical abortion provided at healthcare setup, there was no significant difference in terms of effectiveness and safety. In determining the need for pre-abortion tests such as ultrasound, most studies found these tests to be compulsory which would require the clients to visit healthcare facilities [20,24,25,29,32]. However, some studies argued that only certain cases such as uncertain gestations or confirmation of ectopic pregnancies needed to undergo pre-abortion tests including ultrasound [25,26,31]. In trying to compare the efficacy of providing TMA without tests, Hyland, et al., [30] reported no compromise to effectiveness with clients who underwent pre-abortion tests and those who did not. On the contrary, another study compared two groups; test and non-test and reported incomplete abortion rates to be high among the non-test group. For the two groups, there were low rates of continuing pregnancy and need for surgical intervention [20]. Another retrospective cohort study found no difference in effectiveness in dispensing abortion medication either through in-person or with telemedicine via mail [25]. The evidence drawn from the above studies has a convergent argument that TMA is as effective as care provided through in-person.
Theme 3: Patient Acceptability of Telemedicine Abortion
The author determined three wide components to evaluate acceptability of TMA which included patient satisfaction, comfortability of patients and convenience. High rates of patient satisfaction as high as 90% due to TMA was reported by most studies [19,20,22,24,25,29,31,32] with two studies scoring 100% patient satisfaction rates [24,25]. One study reported the willingness of patients to refer TMA to their colleagues and friends [24] and would choose TMA in future for similar purposes. Several studies reported patient satisfaction and comfortability of using TMA, further citing the positive experiences with respective abortion care providers [20,29,33,34,35]. According to Ruggiero, et al., [33], patients expressed their comfort in interacting with their abortion care providers during TMA sessions due to absence of perceived stigma that would have otherwise occurred in in-person visit and interaction. The findings above pose TMA as a platform widely acceptable to patients and enhances comfortability among most patients. In choosing between TMA and In-person visit, most patients preferred TMA with reasons such as improved access, reduced stigma and pliability being highly associated with TMA. Most patients reported comfort as their reasons for TMA preference whereas others valued a non-judgmental environment that was possible with TMA. Also, TMA was found to be more convenient than in-person [34,36].
Theme 4: Accessibility of Abortion Care Services through TMA
The author identified subthemes such as affordability, distance, ease of access and equity as metrics for determining TMA accessibility. A study cited a scenario where 13 % of patients would have otherwise opted for continued pregnancy given the barriers of accessibility, privacy, and affordability, in the absence of TMA [20]. Some studies associated TMA with reduced costs of travel and affordability. Others cited that most patients were faced with cost barriers such as travel costs, childcare costs, and hotel costs to accessing abortion services, which would otherwise be avoided through TMA [18,19,22]. Some patients identified distance of traveling as a barrier to accessing abortion services [37]. Patients who utilized TMA travelled less compared to the in-person visits [35]. Also, TMA was likely to be utilized in remote areas that were far from abortion-care facilities [38]. In terms of obtaining pre-abortion tests, two studies cited that patients found it easier to access to tests through TMA, with significant proportion of patients expressing difficulty, posing access barrier [39,40]. Although TMA greatly improves access, there still exists an underpinning challenge of equity. The reliability of internet services and mobile phones is not consistent across the population. For instance, rural residents and those with low income have limited access to internet and mobile phones, thus preventing them from engaging through TMA platforms [37].
Discussion
According to WHO framework, components such as safety, effectiveness and acceptability are key to determining quality of care [14]. WHO also equates quality of care to women’s rights to health and upholding dignity. Women in Kenya experience conundrums such as legal uncertainties, stigma, and cost of services in accessing high quality abortion care [4]. This study has explored utilisation telemedicine abortion to improve access to high quality abortion care. Themes such as safety, effectiveness, acceptability, and access have been identified from various research papers, highlighting the viability of telemedicine abortion and the impact it has on improving quality of abortion care services. From the findings, TMA has proven to be safe with minimal complications and no mortalities reported [19]. The few complications emerging have been resolved remotely through use of electronic health channels such as telephone, emails, and internet information [24]. The evidence established indicates low rates of blood transfusion, infection rates and complications from TMA [25]. These findings resonate with a study that sort to compare the safety of TMA and in-person abortion care and found no significant difference [21]. Another study also reported low hospital admission rates and no mortalities from TMA [20].
Many studies found TMA to be effective with high success rates, low surgical interventions and minimal chances of continuing pregnancy reported. From the findings established, there was no significant difference in effectiveness between TMA and in-person abortion care. However, one study argued that some tests such as ultrasound and laboratory tests were only possible through hospital visits, thus requiring clients to make in-person visits to clinics [31]. In contrast, some studies did not perceive these tests to be necessary unless on exceptional circumstances such as uncertain gestations or a need to establish ectopic pregnancy [29,31]. The findings from this study suggested TMA to be acceptable amongst patients across several settings. Many patients were satisfied with TMA and would recommend the service to other eligible clients. Similar findings are relatable to a study examining the utility of telemedicine in Kenya, which established high rate of patient satisfaction with using e-consultations to provide care [41]. It also established that clients expressed positive experiences with their abortion care providers through TMA as it provided them with comfort and confidence to share their health issues. This increased their preference to TMA over In-person clinic visit. These findings resonate with a study that explored on quality of abortion services in Kenya and India and found out that women preferred a safe and comfortable environment with social support when receiving abortion care [42]. In comparison between TMA and In-person visit, patients preferred TMA and portrayed it as having more person-centered care approach in terms of privacy, confidentiality, trust, dignity, and social support than in-person visits. The findings also suggest that TMA has enabled patients to overcome several abortion barriers such as stigma, flexibility, and access. to acquiring abortion services and thus becoming a preferred choice for eligible clients.
This study found TMA to increase access to abortion services and suppresses the associated barriers. At one instance, a study cited a scenario where a sect of patients would have opted for continued pregnancy in the absence of TMA due to access barriers associated with in-person clinic visits 34. Among the barriers identified were travel costs, ease of access, childcare costs, and cost of abortion procedures. The clients believed that these barriers were mitigable with the use of TMA. These findings are like qualitative research conducted in South Africa on acceptability of TMA which found it as a preferable means for women to save on travel cost and time [26]. Also, distance was identified as one of the barriers to accessing abortion care services, citing that patients utilising TMA were found to travel lesser distance than those doing in-person visits [43]. The study also identified TMA as reliable means for clients in remote areas living far from abortion clinics. A few studies found TMA to be reliable when accessing pre-abortion tests whereas other studies cited it as a barrier due to its difficulty to obtain these tests. However, equity was cited as challenge associated with TMA, due to limited access of internet services, favoring those with income and living in urban areas. Similar findings were found in qualitative research in South Africa, which termed TMA as inaccessible to women from poor background who could hardly afford mobile phones, thus creating a barrier to access [26]. Therefore, considering the equity challenges and limiting laws abortion, for instance in Kenya, TMA cannot be guaranteed to fully solve the access barriers of abortion services.
Limitations of the Study
This study has deliberately narrowed on the benefits of adopting telemedicine abortion as a form of improving access to abortion services and discussed less of the challenges associated with telemedicine abortion such as legal constraints, social and cultural barriers, and religious beliefs, which could affect its adoption. The study has focused on the experiences and benefits to the eligible women and ignored the perspectives from the provider’s side on telemedicine abortion. In addition, the scope of the study is based on assumptions that abortion is legal, and the guidelines present in the proposed context of implementation. Due to limited research conducted on telemedicine abortion in developing countries, the author selected broad spectrum of research articles from developed countries that have successfully implemented telemedicine abortion, thus providing heterogeneous results which may not be fully applicable to proposed context, considering the different social, political, and economic factors. The outcome of this study might have been divergent if articles other than those published in English were included. Despite the difference in the context of implementation, with more papers from developed countries, the perspectives of eligible women have been fairly represented to reflect ideal experiences for women in both contexts. This study has established limited research on telemedicine abortion in developing countries.
Conclusion
From the studies reviewed, telemedicine abortion appears to be safe, acceptable, effective and increases access to abortion care services. Most women believe that TMA provides more autonomy, convenience, privacy, confidentiality and is cost effective than in-person visit. TMA is suitable for breaking the barriers such as inadequate health facilities for providing abortion care services, cost of procedure, client comfort with healthcare providers, perceived stigma, and privacy and confidentiality. Furthermore, it establishes a platform for individualized care with enhanced information sharing amongst the eligible clients. From the studies conducted, adoption of telemedicine abortion reduces waiting consultation times, early abortion treatment and care during pregnancy, privacy during consultation and enhances convenience and reduced costs of frequent traveling to relevant healthcare facilities. However, the unclear legal abortion guidelines from the Ministry of Health still cause confusion amongst both the healthcare providers and patients, which stagnates the upscale of safe abortion care services through telemedicine in Kenya. Therefore, the Ministry of Health, civil society organizations, religious institutions and other key stakeholders have a mandate to put in place health policies and guidelines to allow for available and accessible safe abortion services without the limiting legal barriers. Furthermore, telemedicine curricula ought to be integrated with health training programs to bolster awareness and adoption of telemedicine in healthcare practice [44].
Acknowledgements
None.
Conflict of Interest
None.
References
- (2012) World Health Organization Unsafe abortion incidence and mortality: global and regional levels in 2008 and trends during 1990-2008 (No. WHO/RHR/12.01). World Health Organization.
- (2015) World Health Organization Health worker role in providing safe abortion care and post abortion contraception. World Health Organization.
- Jayaweera RT, Ngui FM, Hall KS, Gerdts C (2018) Women’s experiences with unplanned pregnancy and abortion in Kenya: a qualitative study. PloS One 13(1): e0191412.
- Mohamed SF, Izugbara C, Moore AM, Mutua M, Kimani Murage EW, et al. (2015) The estimated incidence of induced abortion in Kenya: a cross-sectional study. BMC Pregnancy Childbirth 15: 185.
- Singh S, Shekhar C, Acharya R, Moore AM, Stillman M, et al. (2018) The incidence of abortion and unintended pregnancy in India, 2015. Lancet Glob Health 6(1): e111-e120.
- Izugbara CO, Egesa C, Okelo R (2015) ‘High profile health facilities can add to your trouble’: women, stigma and un/safe abortion in Kenya. Soc Sci Med 141: 9-18.
- Aliongo SAM (2021) The evolving law on sexual and reproductive health rights and the right to abortion in Kenya.
- Kitui J, Lewis S, Davey G (2013) Factors influencing place of delivery for women in Kenya: an analysis of the Kenya demographic and health survey, 2008/2009. BMC Pregnancy Childbirth 13: 40.
- Tisnanga JS, Kyongo J (2023) Impact of Telemedicine on Enhancing Healthcare Services in Kenya: A Comprehensive Review.
- Garvin LA, Hu J, Slightam C, McInnes DK Zulman DM (2021) Use of video telehealth tablets to increase access for veterans experiencing homelessness. J Gen Intern Med 36(8): 2274-2282.
- Dunlop H, Sinay AM, Kerestes C (2023) Telemedicine abortion. Clin Obstet Gynecol 66(4): 725-738.
- Waiyaiya E, Nyaga N, Nyangena J, Nyotu R, Wamicwe J, et al. (2024) Digital Health Convergence Workshop: The Kenyan Experience. Oxford Open Digital Health 2.
- (2017) World Health Organization What is quality of care and why is it important. World Health Organization.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372: n71.
- Grossman D, Grindlay K, Buchacker T, Lane K Blanchard K (2011) Effectiveness and acceptability of medical abortion provided through telemedicine. Obstet Gynecol 118(2 Pt 1): 296-303.
- Kohn JE, Snow JL, Simons HR, Seymour JW, Thompson TA, et al. (2019) Medication abortion provided through telemedicine in four US states. Obstet Gynecol 134(2): 343-350.
- Kerestes C, Murayama S, Tyson J, Natavio M, Seamon E, et al. (2021) Provision of medication abortion in Hawai ‘i during COVID-19: Practical experience with multiple care delivery models. Contraception 104(1): 49-53.
- Raymond E, Chong E, Winikoff B, Platais I, Mary M, et al. (2019) TelAbortion: evaluation of a direct to patient telemedicine abortion service in the United States. Contraception 100(3): 173-177.
- Chong E, Shochet T, Raymond E, Platais I, Anger HA, et al. (2021) Expansion of a direct-to-patient telemedicine abortion service in the United States and experience during the COVID-19 pandemic. Contraception 104(1): 43-48.
- Kerestes C, Delafield R, Elia J, Shochet T, Kaneshiro B, et al. (2022) Person‐centered, high‐quality care from a distance: a qualitative study of patient experiences of TelAbortion, a model for direct‐to‐patient medication abortion by mail in the United States. Perspect Sex Reprod Health 54(4): 177-187.
- Aiken AR, Lohr PA, Lord J, Ghosh N, Starling J (2021) Effectiveness, safety and acceptability of no‐test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG 128(9): 1464-1474.
- Reynolds Wright JJ, Johnstone A, McCabe K, Evans E, Cameron S (2021) Telemedicine medical abortion at home under 12 weeks’ gestation: a prospective observational cohort study during the COVID-19 pandemic. BMJ Sex Reprod Health 47(4): 246-251.
- Wiebe ER, Campbell M, Ramasamy H, Kelly M (2020) Comparing telemedicine to in-clinic medication, abortions induced with mifepristone and misoprostol. Contracept X 2: 100023.
- Peña M, Flores KF, Ponce MM, Serafín DF, Zavala AMC, et al. (2022) Telemedicine for medical abortion service provision in Mexico: a safety, feasibility, and acceptability study. Contraception 114: 67-73.
- Seymour JW, Melville C, Thompson TA, Grossman D (2022) Effectiveness and safety of a direct-to-patient telehealth service providing medication abortion targeted at rural and remote populations: Cross-sectional findings from Marie Stopes Australia. Contraception 115: 67-68.
- Endler M, Petro G, Danielsson KG, Grossman D, Gomperts R, et al. (2022) A telemedicine model for abortion in South Africa: a randomised, controlled, non-inferiority trial. Lancet 400(10353): 670-679.
- Anger HA, Raymond EG, Grant M, Haskell S, Boraas C, et al. (2021) Clinical and service delivery implications of omitting ultrasound before medication abortion provided via direct-to-patient telemedicine and mail in the US. Contraception 104(6): 659-665.
- Reynolds Wright JJ, Johnstone A, McCabe K, Evans E, Cameron S (2022) Adherence to treatment and prevalence of side effects when medical abortion is delivered via telemedicine: a prospective observational cohort study during COVID-19. BMJ Sex Reprod Health 48(3): 185-192.
- Upadhyay UD, Raymond EG, Koenig LR, Coplon L, Gold M, (2022) Outcomes and safety of history-based screening for medication abortion: a retrospective multicenter cohort study. JAMA Inter Med 182(5): 482-491.
- Hyland P, Raymond EG, Chong E (2018) A direct‐to‐patient telemedicine abortion service in Australia: retrospective analysis of the first 18 months. Austr New Zealand J Obstet Gynaecol 58(3): 335-340.
- Chen MJ, Creinin MD (2015) Mifepristone with buccal misoprostol for medical abortion: a systematic review. Obst Gynecol 126(1): 12-21.
- Tsereteli N, Mamatsashvili L, Tsertsvadze G, Tsereteli T, Platais I (2023) Telemedicine medical abortion service in Georgia: an evaluation of a strategy with reduced number of in-Clinic visits. Eur J Contracept Reprod Health Care 28(2): 141-146.
- Ruggiero SP, Seymour JW, Thompson TA, Kohn JE, Snow JL, et al. (2022) Patient and provider experiences using a site-to-site telehealth model for medication abortion. Mhealth 8: 32.
- Boydell N, Reynolds Wright JJ, Cameron ST, Harden J (2021) Women’s experiences of a telemedicine abortion service (up to 12 weeks) implemented during the coronavirus (COVID‐19) pandemic: a qualitative evaluation. BJOG 128(11): 1752-1761.
- Grindlay K, Lane K, Grossman D (2013) Women's and providers' experiences with medical abortion provided through telemedicine: a qualitative study. Women's Health Issues 23(2): e117-e122.
- Sudhinaraset M, Afulani P, Diamond Smith N, Bhattacharyya S, Donnay F, et al. (2017) Advancing a conceptual model to improve maternal health quality: the person-centered care framework for reproductive health equity. Gates Open Res 1: 1.
- Thompson TA, Seymour JW, Melville C, Khan Z, Mazza D, et al. (2022) An observational study of patient experiences with a direct-to-patient telehealth abortion model in Australia. BMJ Sex Reprod Health 48(2): 103-109.
- Fix L, Seymour JW, Sandhu MV, Melville C, Mazza D, et al. (2020) At-home telemedicine for medical abortion in Australia: a qualitative study of patient experiences and recommendations. BMJ Sex Reprod Health 46(3): 172-176.
- Altshuler AL, Whaley NS (2018) The patient perspective: perceptions of the quality of the abortion experience. Curr Opin Obstet Gynecol 30(6): 407-413.
- Godfrey EM, Fiastro AE, Ruben MR, Young EV, Bennett IM, et al. (2023) Patient perspectives regarding clinician communication during telemedicine compared with in-clinic abortion. Obstet Gynecol 141(6): 1139-1153.
- Onsongo S, Kamotho C, Rinke de Wit TF, Lowrie K (2023) Experiences on the Utility and Barriers of Telemedicine in Healthcare Delivery in Kenya. Intern J Telemedicine Applications 2023(1): 1-10.
- Baum SE, Wilkins R, Wachira M, Gupta D, Dupte S, et al. (2021) Abortion quality of care from the client perspective: a qualitative study in India and Kenya. Health Policy Plan 36(9): 1362-1370.
- Endler M, Petro G, Danielsson KG, Grossman D, Gomperts R, et al. (2022) A telemedicine model for abortion in South Africa: a randomised, controlled, non-inferiority trial. Lancet 400(10353): 670-679.
- Meurice ME, Whitehouse KC, Blaylock R, Chang JJ, Lohr PA (2021) Client satisfaction and experience of telemedicine and home use of mifepristone and misoprostol for abortion up to 10 weeks’ gestation at British Pregnancy Advisory Service: A cross-sectional evaluation. Contraception 104(1): 61-66.






 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.