Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Pain Characteristic and Its Impact in Geriatric Patients
*Corresponding author: Mauricio B Almeida, Federal University of Minas Gerais, Belo Horizonte, Brazil.
Received: February 05, 2020; Published: February 26, 2020
DOI: 10.34297/AJBSR.2020.07.001183
Abstract
Background: Advanced age has the risk of certain health disorders that can cause pain. It becomes big problem since it often leads to serious health problems such as increased depression and decreased the quality of life. To better understand management of pain in geriatric, recognizing pain’s characteristic and it,s impact in geriatric patients are needed.
Purpose: The primary concern of this study was to identify pain characteristic and its impact in geriatric patients.
Methods: In this cross-sectional study, the data were obtained from geriatric patients (more than 60 years old) that attend internal medicine clinic and neurology clinic in Bethesda hospital Yogyakarta Indonesia. We collect the data about the type of pain, pain characteristic, pain severity and pain impact.
Results: From 134 patients, 72 (53.73%) were female and 107 (79,85%) patients aged between 60-74 years old. Of all patients, 60 (44.78%) had inflammatory pain and 88 (65,67%) had moderate pain. In terms of pain duration 94 (70,15%) reported chronic pain and 40(29,85%) with acute pain. With regard to location, most had low back pain 47,76%, shoulder pain 14,18 % and then knee pain 13,43%. Off all patients, pain also had a negative impact in activity, sleep and emotion. Pain can disturb sleep 87 (64,47%), activity (85,82%), and emotion (51,49%).
Conclusion: There has been high prevalence of chronic pain among the elderly. Moderate and low back pain were the most frequent. Pain can disturb activity, sleep, and activity of the elderly.
Keywords: Pain characteristic; pain impact; Geriatric patients
Introduction
Elderly men and women represent the fastest growing demographic in the world’s popultaion. WHO 2018 reported by 2050 the number of people aged 60 years and older is expected to total 2 billion, up from 900 million in 2015. With advancing age, pain is the most problem in elderly people [1]. Studies suggest 25% to 50% of community dwelling elderly report pain and that for elderly residents in nursing home the prevalence of pain is as high as 80% [2]. The pain is a common subjective symptom among adults older than age 65. Studies indicate that more than 50% of older adults suffer chronic pain [3], and the pain prevalence among patients at long-term geriatric care facilities is estimated at 48%- 79%2 [4].
Chronic pain is one of the most prominent causes of disability worldwide and represents a major challenge for public health. Elderly Patients with chronic pain have reported a significant impact on their functional impairment, falls, slow rehabilitation, mood changes (depression and anxiety), decreased socialization, sleep and appetite disturbance, and greater healthcare use and costs [5]. Consequences of untreated pain include unnecessary suffering and impaired quality of life, functional loss, depression and behavioral disturbances including aggression, agitation, and wandering [6, 7, 8].
However, pain characteristic and its impact in elderly patient in Indonesia is still rarely studied. The primary concern of this study was to identify pain characteristic and its impact in geriatric patients. With identify pain characteristic and it ‘s impact in geriatric patient, doctor and caregiver can do pain management based on the pain characteristic and it’s impact in geriatric patient.
Methods
This is a cross sectional study with standardized pain assessment tools from Brief Pain Inventory. The data were obtained from geriatric patients (more than 60 years old) that attend internal medicine clinic and neurology clinic in Bethesda hospital Yogyakarta Indonesia. The eligible criteria for study subjects were: male and female, age 60 years old and above, can communicate effectively, and give consent to join the study. We collect the data about the type of pain, pain characteristic, and pain severity. The pain impact was systematically measured to the sleep quality, activities, and emotional status. The information about the medication were collected systematically using the electronic medical record and prescribing information system. The data were analyzed descriptively using standard statistical software. This study obtained ethical approval form Duta Wacana Christian University School of Medicine Ethic Committee.
Results
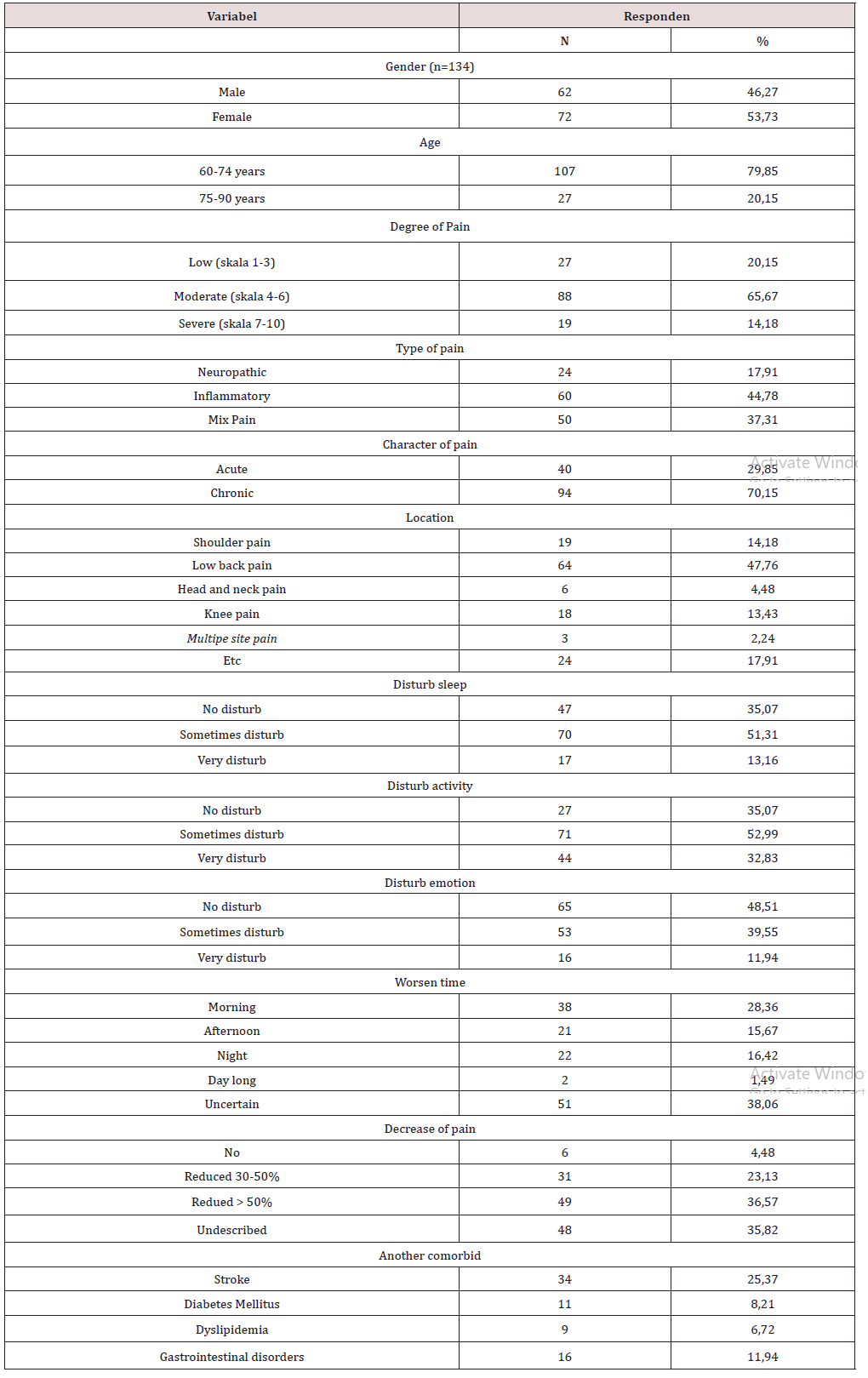
From 134 patients, 72 (53.73%) were female and 107 (79,85%) patients aged between 60-74 years old. Of all patients, 60 (44.78%) had inflammatory pain and 88 (65,67%) had moderate pain. In terms of pain duration 94 (70,15%) reported chronic pain and 40(29,85%) with acute pain. With regard to location, most had low back pain 47,76%, shoulder pain 14,18 % and then knee pain 13,43%. Off all patients, sometimes pain distrub sleep 51,33%, activity 52,99% and emotion 39,55%. After treatment, most patients had decrease of pain >50% (36,57%), 30-50% (23,13%) (Table 1).
Discussion
Pain characteristic in adult/geriatric is different with the pain characteristic in young/pediatric patient. The study by King et all (2011) estimate the prevalence of chronic pain in the young patient (pediatric). In young or pediatric patient, headache is most prevalent and is reported in 8% to 83% of children, followed by abdominal pain (4%–53%), musculoskeletal pain (4%–40%), and back pain (14%–24%). In adult or geriatric patient, concert with age-associated changes in somatosensory function, chronic comorbidities often contribute to pain, including musculoskeletal disorders, diabetes, and cancer, particularly with advanced stages of chronic disease. In addition, pain may result from treatments, such as surgery and chemotherapy. From this study, musculoskeletal related pain (low back pain) is the most common site of pain in geriatric patient [9].
Pathophysiological pain research studies have taught us that the pain signal initiates from the stimulation of peripheral nociceptor nerve terminals from specific receptors/ ion channels. Pain circuitry activates nociceptors in response to painful stimuli. Pain is signaled to the brain via a wave of depolarization. Such depolarization encompasses a discharge of sodium and potassium, via sodium channels. The surge of sodium is transmitted to firstorder neurons ending in the brain stem within the trigeminal nucleus or dorsal horn of the spinal cord. Sensory information is then spread via small-diameter C-fibers terminating within individual regions of the dorsal horn of the spinal cord (laminae I-IV), from where the signal is transmitted to the brainstem, thalamus, and higher cortical centers [10]. Within this structure, the electrochemical signal opens voltage-gated calcium channels in the presyn- aptic terminal for calcium to enter and allow glutamate to release into the synaptic space. Glutamate connects with N-methyl-D-aspartate (NMDA) receptors on the second-order neurons producing depolarization. These neurons cross over the spinal cord and ascend to the thalamus, where they synapse with third-order neurons, after which they connect to the limbic system and cerebral cortex.
Neurophysiologic changes associated with aging seem to influence pain processing, with evidence to support a general increase in pain threshold and reduced pain tolerance from deterioration of the pathways involved in endogenous inhibition. An age-related increase in pain threshold to thermal stimuli may be related to loss in the structure and function of the peripheral (A delta fibers) and central nervous system (CNS) pathways implicated in the processing of noxious information [11]. Experimental pain studies provide some evidence of reduced sensitivity to mild pain with advancing age, particularly for thermal pain. Other types of pain stimuli (i.e., mechanical, electrical) are more equivocal, with reports of no change or decreased thresholds in older adults. In contrast, results from 10 independent studies showed reduced pain tolerance as a function of age, irrespective of stimulus method [12, 13]. In addition, temporal summation of noxious heat is enhanced in the CNS of older adults compared with younger individuals [14]. Age-related impairment in opioid and nonopioid mechanisms of the endogenous pain inhibitory systems have been described, showing less than a third of the strength of induced effects on sensitivity when compared with younger adults [15]. Collectively, these studies suggest that aging increases vulnerability to persistent severe pain owing to reduced pain tolerance and impaired endogenous pain-modulating capacities.
Pain in older adults is a significant problem worldwide, and is associated with reduced activity, falls, mood disorders, sleep disturbances, isolation, and substantial disability; factors that compromise quality of life and well-being. Persistent pain may lead to frailty, compromising general health and functional status [16, 17]. From this study, chronic pain in geriatric patient is higher than acute pain (70,15% and 29,85%) and it can disturb activity, sleep, and emotion. Although pain management can be successfully implemented for most older adults, pain remains undertreated in the oldest old, African Americans, and ethnic minorities, as well as in individuals with cognitive impairment [18]. Overall, older adults are less likely to receive analgesics compared with young adult patients despite the significant ramifications to general health and well-being [19]. Specific physiologic changes in older adults need to be considered when selecting appropriate analgesic therapy [11]. Older adults have reduced intravascular volume and muscle mass, which may alter drug distribution resulting in increased plasma levels relative to younger individuals, and leading to increased volume of distribution of fat-soluble opioids (i.e., fentanyl) because of greater fat/lean body mass ratio, whereas decreased total body water can result in increased plasma levels of hydrophilic opioids (i.e., morphine). Renal clearance (glomerular filtration, tubular reabsorption, and secretion) decreases at a rate of 6% to 10% per decade beginning at age 30 years.
Thus, reduced renal function without underlying kidney disease is common in older adults. In addition, hepatic clearance is reduced because of decreased hepatic blood flow. Nonsteroidal anti-inflammatory drugs are not recommended by the American Geriatrics Society, especially long-term use because of the high risk of adverse effects on the gastrointestinal, cardiovascular, and renal systems. Dosage reductions (25%–50%) of other medications used to treat pain in older adults are typically necessary, particularly at initiation of treatment [20]. In this study, by administering pain medication can reduce pain <50% in geriatric patient.
Conclusion
There has been high prevalence of chronic pain among the elderly. Moderate and low back pain were the most frequent. Pain can disturb activity, sleep, and activity of the elderly. Because of that, the good management of pain in geriatric is important to reduce pain in geriatric and make geriatric patients live well.
Authors’ contribution
RP - Concept and design of the study, manuscript preparation, statistically analyzed and interpreted, critical revision of the manuscript.
FB - Concept and design of the Study, collected data, preparing first draft of manuscript, critical revision of manuscript and review of the study.
YF - Concept and design of the Study, collected data, preparing first draft of manuscript, critical revision of manuscript and review of the study.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Bicket MC, Mao J (2015) Chronic Pain in Older Adults. Anesthesiology Clin 33: 577-590.
- Kaye AD, Baluch A, Kaye RJ, Niaz RS, Kaye, AJ, et al. (2014) Geriatric pain management, pharmacological and nonpharmacological considerations. Journal of psychology & neuroscience 7(1): 15-26.
- Nahin RL (2015) Estimates of pain prevalence and severity in adults: United States, 2012. The Journal of Pain 16(8): 769-780.
- Bj€ork S, Juthberg C, Lindkvist M, Wimo A, Sandman PO, et al. (2016) Residents’ engagement in everyday activities and its association with thriving in nursing homes. Journal of Advanced Nursing 73(8): 1884-1895.
- Dueñas, M, Ojeda B, Salazar A, Mico JA, Failde I (2016) A review of chronic pain impact on patients, their social environment and the health care system. Journal of Pain Research 9: 457-467.
- Klapwijk MS, Caljouw MAA, Pieper MJC, van der Steen JT, Achterberg WP (2016) Characteristics associated with quality of life in long-term care residents with dementia: A cross-sectional study. Dement Geriatr Cogn Disord 42(3-4): 186-197.
- Zakoscielna KM, Parmelee PA (2013) Pain variability and its predictors in older adults: Depression, cognition, functional status, health, and pain. J Aging Health 25(8): 1329-1339.
- Hadjistavropoulos T, Voyer P, Sharpe D, Verreault R, Aubin M (2008) Assessing pain in dementia patients with comorbid delirium and/or depression. Pain Manag Nurs 9(2): 48-54.
- King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, et al. (2011) The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 152(12): 2729-2738.
- Bradesi S (2010) Role of spinal cord glia in central processing of peripheral pain perception. Neurogastroenterol Motil 22(5): 499-511.
- Hadjistavropoulos T, Herr K, Prkachin KM, Craig KD, Gibson SJ, et al. (2014) Pain assessment in elderly adults with dementia. Lancet Neurol 13(12): 1216-1227.
- Gibson SJ, Farrell M (2004) A review of age differences in the neurophysiology of nociception and the perceptual experience of pain. Clin J Pain 20(4): 227-239.
- Lautenbacher S (2012) Experimental approaches in the study of pain in the elderly. Pain Med 13(Suppl-2): S44-S50.
- Edwards RR, Fillingim RB (2001) Effects of age on temporal summation and habituation of thermal pain: clinical relevance in healthy older and younger adults. J Pain 2(6): 307-317.
- Riley JL, King CD, Wong F, Fillingim RB, Mauderli AP (2010) Lack of endogenous modulation and reduced decay of prolonged heat pain in older adults. Pain 150(1): 153-160.
- Shega JW, Andrew M, Kotwal A, Lau DT, Herr K, et al. (2013) Relationship between persistent pain and 5-year mortality: a population-based prospective cohort study. J Am Geriatr Soc 61(12): 2135-2141.
- Shega JW, Dale W, Andrew M, Paice J, Rockwood K, et al. (2012) Persistent pain and frailty: a case for homeostenosis. J Am Geriatr Soc 60(1): 113-117.
- Malec M, Shega JW (2015) Pain management in the elderly. Med Clin North Am 99(2): 337-350.
- Hwang U, Belland LK, Handel DA, Yadav K, Heard K, et al. (2014) Is all pain is treated equally? A multicenter evaluation of acute pain care by age. Pain 155(12): 2568-2574.
- Gupta DK, Avram MJ (2012) Rational opioid dosing in the elderly: dose and dosing interval when initiating opioid therapy. Clin Pharmacol Ther 91(2): 339-343.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.