Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Case Report of a Glomangioma in an Unusual Location and Review of the Literature
*Corresponding author: Hiroko Kodama, Special Appointment Professor, Teikyo Heisei University, Toshima-ku, Tokyo, 170—8445, Japan.
Received: June 14, 2020; Published: September 17, 2020
DOI: 10.34297/AJBSR.2020.10.001511
Abstract
Glomangioma or glomus tumors are rare neoplasms of the glomus body, which are located in the stratum reticularis of the dermis throughout the body. Its location on the elbow is unusual and presents a diagnostic challenge. It manifests clinically by a triad of pain, tenderness and cold hypersensitivity. We present a case of 75-year-old male who presented with a very painful nodule over the left elbow for the past 3 years. Dermoscopy showed an angiomatous nodule. After local excision, histopathology revealed sheets of epitheloid-like ovoid cells, disposing around dilated and congestive vascular structures without nuclear pleomorphism or mitotic activity. On immunohistochemistry, glomus cells were positive to smooth muscle actin, characteristic of a glomus tumor.
Keywords: Glomus Body; Elbow; Glomus Cells; Glomangioma
Introductions
Glomus tumors are rare benign mesenchymal neoplasms of the skin accounting for 1% to 2% of all soft tissue tumors. They arise from the neuroarterial receptors called glomus bodies [1]. These receptors are located in the walls of the Sucquet-Hoyer canal that is a specialised arteriovenous anastomosis central to thermoregulation [2]. Glomus tumors typically arise in the extremities, especially subungual, but they can occur all over the body. Most tumours are less than 1 cm in diameter and their surgical removal is usually effective and curative. The diagnosis is histological and the prognosis is good.
Case Presentation
A 75-year-old male presented to the dermatology department with complaints of a very painful nodule, measuring 1 × 0,7 cm, over the left elbow for the past 3 years. The pain was non-radiating and there was no history of other swellings in the body, or history of a previous trauma. Local examination revealed an angiomatous well limited nodule of 1x0,7 cm (Figure 1). The swelling was in the subcutaneous plane and the distal limb was normal. En Dermoscopy examination, the nodule was angiomatous with the presence of some irregular lobules and some septas (Figure 2). No regional lymphadenopathy was palpated.
The patient underwent a local excision of his lesion.
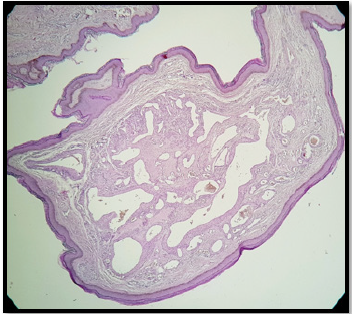
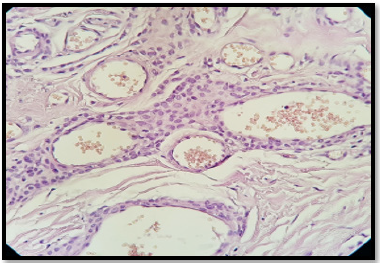
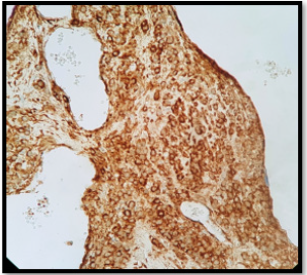
Histopathology demonstrated a dermis benign, well limited with a lobulated architecture tumor proliferation (Figure 3). It’s made up of numerous epitheloid-like ovoid cells, disposing around dilated and congestive vascular structures (Figure 4). There was no evidence of nuclear pleomorphism or mitotic activity. On immunohistochemistry, glomus cells were positive to smooth muscle actin (SMA) (Figure 5). The diagnosis of glomangioma was made and no further treatment was indicated.

Figure 2: Dermoscopy examination showing an angiomatous nodule with some irregular lobules and some septas.
Discussion
Glomangiomas are benign well limited tumors of the skin characterized by abnormal, smooth muscle–like glomus cells [3]. They were first described in 1924 by Masson [4] like a neuromyoarterial glomus of the tactile regions, which he later renamed the neurovascular glomus and its tumors. The term glomangioma was coined by Bailey in 1935 [5], corresponding to a rare neoplasm of the glomus body. Glomus bodies are present in the stratum reticularis of the dermis and the glomus tumors arise from modified smooth muscle cells that we found normally is specialized arteriovenous shunts named also Sucquet-Hoyer canals. These channels are lined with endothelial cells, contain several layers of glomus cells in their walls, and connect afferent arterioles to efferent venules [6].
There are 2 forms of glomus tumors. The solitary form is more common than the multiple type, representing 90% of all cases. The multiple variants is seen most often in children and is thought to be inherited in an autosomal dominant pattern [2]. Glomus tumors are found in women more than men (sex ratio=2/1) [7,8], and they are typically located at the distal extremities. In approximately 65% of cases, the tumor presents in the subungual location and most commonly is diagnosed between 20 and 40 years of age [9], unlike our case patient who is older. This tumor manifests clinically by a triad of pain, tenderness and cold hypersensitivity. On clinical examination, the solitary form of the tumor is small (less than 1 cm), well-localized, painful and purple nodules [10]. In contrast, multiple glomus tumors may be slightly larger and less well circumscribed and more painful than solitary glomus tumors [6]. Due to the relative paucity of these lesions, the diagnosis may be late, and patients on average suffer from symptoms for 4–7 years from initial presentation [11].
Histopathologically, typical glomus tumors show variable proportions of glomus cells, blood vessels, and smooth muscle cells [12]. The blood vessels are dilated and surrounded by glomus cells. The glomus cells are uniform round, cuboidal or polygonal with centrally, rounded nuclei and prominent eosinophilic cytoplasm, without atypia, nor mitosis. These cells are positif for SMA, and vascular endothelial cells are positive for factor VIII and CD34 [13]. Always remember to eleminate a malignant lesion. In 1990, Gould et al. classified atypical glomus tumors as locally infiltrative glomus tumors, glomangiosarcoma emerging from a benign glomus tumor, and glomangiosarcoma arising de novo [14]. In our case, we did not note any infiltrative zones and there was no evidence of nuclear pleomorphism or mitotic activity.
Depending on the prevalence of glomus cells, vascular smooth muscle cells, and spindle cells resembling smooth muscle, glomus tumors can be subdivided into solid glomus tumor, glomangioma, and glomangiomyoma [12]. Most common is the solid type, found in 75% of cases, in which the glomus cells predominate and appearing in solid cell sheets. The glomangioma variant can be found in 20% of resected lesions and it is associated with more abundant vascularity, with large, often dilated vascular channels surrounding nests of glomus cells. Finally, the glomangiomyoma subset occurs in only about 5% of glomus tumors, in which both vascular and smooth muscle cells are prominent. Complete surgical excision is the treatment of choice. Recurrence is rare and is usually due to incomplete excision.
These are benign tumors, but malignancy can be seen in about 1% of cases and there are case reports of metastasis [15]. Malignancy is to be suspected in case of deep location, size greater than 2 cm, mitotic rate greater than 5 per 10 high-power fields and the presence of abnormal mitotic figures, and moderate to high nuclear grade. If all of these criteria are present, the risk of metastasis has been found to be 25% [16]. In our case, the malignancy was eliminated due to the small size of the lesion, its superficial location and the absence of nuclear pleomorphism or mitotic activity in the histological examination.
Conclusion
We report a case of glomangioma in an unusual location, the elbow, presenting with sharp pain with no history of trauma to the area. Because of their rarity and nonspecific presentation, the diagnosis was not suggested by clinical presentation and the final diagnosis was confirmed by histological evaluation.
Conflict of Interest
None declared
Funding
No funding sources
Acknowledgements
Not applicable.
Ethical Approval
Not required
References
- D Singh, RS Garg, Vikas, Y Garg, V Arora (2016) “Glomus tumor: a rarity; M.R.I- a big help in early diagnosis.” Journal of Orthopaedi, Case Reports 6(3): 38-39.
- Fletcher C (2000) Tumours of blood vessels and lymphatics. In: Diagnostic histopathology of tumors. Edinburgh: Churchill Livingstone p. 75-76.
- Parsi K, Kossard S (2002) Multiple hereditary glomangiomas: successful treatment with sclerotherapy. Aust J Dermatol 43(1): 43-47.
- Masson P (1924) Le glomus neuromyo-artériel des régions tactiles et ses tumeurs. Lyon Chir 21: 257-280.
- Bailey OT (1935) The cutaneous glomus and its tumors—glomangiomas. Am J Pathol 11: 915-936.
- Myers RS, Lo AK, Pawel BR (2006) The glomangioma in the differential diagnosis of vascular malformations. Ann Plast Surg 57(4): 443-446.
- Lee DW, Yang JH, Chang S, Won CH, Lee MW, et al. (2011) Clinical and pathological characteristics of extradigital and digital glomus tumors: a retrospective comparative study. J Eur Acad Dermatol Venereol 25: 1392-1397.
- Maxwell GP, Curtis RM, Wilgis EF (1979) Multiple digital glomus tumors. J Hand Surg 4(4): 363-367.
- E A Walker, J S Salesky, M E Fenton, M D Murphey (2011) Magnetic resonance imaging of malignant soft tissue neoplasms in the adult, Radiol Clin North Am 49(6): 1219-1234.
- M Miettinen, E Paal, J Lasota, L H Sobin (2002) “Gastrointestinal glomus tumors: a clinicopathologic, immunohistochemical, and molecular genetic study of 32 cases”. The American Journal of Surgical Pathology 26(3): 301-311.
- Drape JL, Idy-Peretti I, Goettmann S, HenryGuérin-Surville, JacquesBittoun (1996) Standard and high resolution magnetic resonance imaging of glomus tumors of toes and fingertips. J Am Acad Dermatol 35(4): 550-555.
- E Calonje, C Fletcher (2000) “Tumors of blood vessels and lymphatics,” Diagnostic Histopathology of Tumors. pp. 66-72.
- Abou Jaoude JF, Roula Farah A, Sargi Z, Khairalla, C Fakih (2000) Glomus tumors: report on eleven cases and a review of the literature. Chir Main 19(4): 243-252.
- EW Gould, J Carlos Manivel, J Albores-Saavedra, H Monforte (1990) “Locally infiltrative glomus tumors and glomangiosarcomas. A clinical, ultrastructural, and immunohistochemical study”. Cancer 65(2): 310-318.
- CD Brathwaite, RJ Poppiti (1996) Malignant glomus tumor. A case report of widespread metastases in a patient with multiple glomus body hamartomas, Am J Surg Pathol 20(2): 233-238.
- AL Folpe, JC Fanburg-Smith, M Miettinen, SW Weiss (2001) Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol 25(1): 1-12.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.