Opinion 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A New Era of Disposable Endoscopy in Urology during Tumultuous Times
*Corresponding author: Michael J Kennelly, Department of Urology, Carolinas Medical Center, Atrium Health 1023 Edgehill Rd. S. Charlotte, NC 28207, USA.
Received: October 01, 2020; Published: October 29, 2020
DOI: 10.34297/AJBSR.2020.10.001554
Introduction
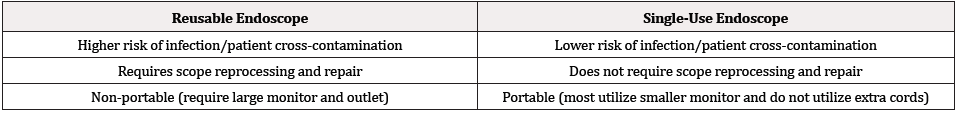
Flexible endoscopy is a key method used by physicians to prevent, diagnose, and treat a wide range of diseases. Similar to gastrointestinal endoscopy and bronchoscopy, cystoscopy is one of the most commonly performed urological procedures which aids providers in visualizing and identifying lower urinary tract pathology. In an effort to minimize patient cross-contamination and risk of infection, many medical devices including endoscopes have shifted to disposable, single-use items, with cystoscopes most recently joining this flourish of technological advancement. There are notable differences between single-use and reusable endoscopes, as displayed in Table 1.
Reusable Endoscopy: Reprocessing and Infection Risks
The multi-channel, reusable flexible endoscopes are associated with one of the highest cross-contamination infection rates among medical devices and thus require rigorous reprocessing and highlevel disinfection (HLD) techniques in between each use to prevent remaining bacterial and protein collection [1]. Reprocessing flexible endoscopes is an arduous, time consuming process which consists of precleaning, leak testing, cleaning, disinfection using an HLD approved by the FDA, rinsing, drying, and correct storage. Standard guidelines indicate more than 100 individual steps, all of which are critical to preventing patient cross-contamination following each use.2,3 Disposable endoscope sheaths were an initial advancement developed to minimize both infection risk by creating a singleuse barrier between the patient and the reusable device, as well as reduce reprocessing time by eliminating the need for HLD in between each use [2,3].
Unfortunately, both human error and deviation from the extensive guidelines are common in endoscope disinfection which leads to increased contamination due to reprocessing failure. Even with strict adherence to reprocessing steps, residual bacteria, formation of biofilm, and subsequent infections are seen with usage of reusable endoscopes [4]. Additionally, studies have shown that continuous reprocessing of reusable endoscopes over time can lead to scope deterioration, including debris, scratches, and reduced image quality resulting in the need for repairs and replacement [5]. The nature of single-use endoscopes aims to reduce these common reusable endoscope pitfalls.
The Nature of Single-Use Endoscopes
Following the development of disposable sheaths, the most recent advancement in endoscopic technology and infection prevention is the creation of fully disposable, single-use endoscopes. A common provider concern regarding single-use endoscopes is the possibility for worsened image quality compared to reusable endoscopes. Over the years, however, great strides have been made to improve digital image processing and quality while simultaneously decreasing the associated costs. A recent study showed single-use bronchoscopes were preferred over reusable as a result of improved visualization and maneuverability [6]. With a different endoscope used for each patient, patient cross-contamination is all but eradicated and infection risk due to inadequate reprocessing techniques is prevented. A systematic review investigating the difference in single-use and reusable bronchoscopes indicated a reduction in both patient contamination risk and subsequent infection in single-use scopes compared to reusable [7].
The nature of the single-use endoscope eliminates the need not only for reprocessing, but also for costly repairs and scope replacement. For this reason, and in combination with minimized infection risk and accompanying costs of patient crosscontamination, single-use flexible endoscopes may have reduced cost per use. Potential cost savings associated with single-use endoscopes, however, are dependent on numerous factors including geography, currency, hospital reimbursement, and certain costs built into the endoscope itself.
The currently available single-use endoscopes are light weight and user friendly compared to the detailed set up, break down, and reprocessing of reusable endoscopes. Certain singleuse endoscopes also utilize small, compact monitors which are “plug and play,” giving the scope a portable nature not applicable to reusable endoscopes. Overall, the eliminated time, cost, and patient infection risk associated with the single-use endoscope, as well as its adaptability and straightforwardness, affords providers the opportunity for increased efficiency and psychological patient comfort. Single-use cystoscopes are still in their developmental infancy, with few manufacturers in the market. Similar to reusable, single-use cystoscopes vary in design specifications, such as distal end diameter, deflection angle, and working accessory ports.
The potentially negative environmental impact is a rightful concern regarding the single-use endoscopes. A recent, comparative Danish study aiming to determine the environmental comparison between reusable and single-use bronchoscopes suggested that reusable bronchoscopes produce comparable or higher levels of waste compared to single-use bronchoscopes due to the PPE and cleaning material consumed per reprocessing [8]. Obviously, more research is required to determine the true difference in environmental impact, as this is only one study and these measurements are highly dependent on each facility and reprocessing PPE requirements.
Conclusion
With ever changing medical and technological advancement, single use endoscopy is the natural next step in the evolution of infection and patient cross-contamination prevention, with singleuse cystoscopy being the most recent development. Furthermore, the current tumultuous times we are in due to the COVID-19 pandemic will forever change many aspects of the healthcare system, including the way we think about containing the spread of infection and disease. Although in its early stages of clinical application, single-use cystoscopy may have its place in medicine and afford opportunities for increased patient efficiency and safety.
References
- Kenters N, Huijskens EGW, Meier C, Voss A (2015) Infectious diseases linked to cross-contamination of flexible endoscopes. Endosc Int Open 3(4): E259-E265.
- Clemens J Quentin, Dowling Robert, Foley Frances, Howard B Goldman, Chris M Gonzalez, et al. (2010) Joint AUA/SUNA White Paper on Reprocessing of Flexible Cystoscopes. Journal of Urology 184(6): 2241-2245.
- Ofstead CL, Hopkins KM, Quick MR, Brooks KB, Eiland JE, et al. (2019) A Systematic Review of Disposable Sheath Use During Flexible Endoscopy. AORN Journal 109(6): 757-771.
- Bisset L, Cossart YE, Selby W, Richard West, Denise Catterson, et al. (2006) A prospective study of the efficacy of routine decontamination for gastrointestinal endoscopes and the risk factors for failure. American Journal of Infection Control 34(5): 274-280.
- Ofstead CL, Wetzler HP, Heymann OL, Johnson EA, Eiland JE, et al. (2017) Longitudinal assessment of reprocessing effectiveness for colonoscopes and gastroscopes: Results of visual inspections, biochemical markers, and microbial cultures. Am J Infect Control 45(2): e26-e33.
- Kriege M, Dalberg J, McGrath BA, AlexanderShimabukuro-Vornhagen, BjörnBillgren, et al. (2020) Evaluation of intubation and intensive care use of the new Ambu® aScopeTM 4 broncho and Ambu® aViewTM compared to a customary flexible endoscope a multicentre prospective, non-interventional study. Trends in Anaesthesia and Critical Care 31: 35-41.
- Mouritsen JM, Ehlers L, Kovaleva J, Ahmad I, El‐Boghdadly K (2020) A systematic review and cost effectiveness analysis of reusable vs. single-use flexible bronchoscopes. Anaesthesia 75(4): 529-540.
- Sørensen BL, Grüttner H (2018) Comparative Study on Environmental Impacts of Reusable and Single-Use Bronchoscopes. American Journal of Environmental Protection 7(4): 55-62.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.