Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Assessment of an Academic Dental Outreach Program on the Geriatric Population in London, Ontario, Canada: Improvement or Inadequacy?
*Corresponding author: Les Kalman, Restorative Dentistry; Chair, Dental Outreach Schulich School of Medicine & Dentistry, Western University, N6A-3K7, London, Ontario, Canada
Received: July 24, 2020; Published: September 11, 2020
DOI: 10.34297/AJBSR.2020.10.001500
Abstract
Aim: Canada’s aging population has seen a historic increase in the last twenty years. Geriatric patients are more likely to have comorbid conditions, cognitive incapacities, verbal limitations and frailty, all of which affect and accentuate pre-existing dental conditions and pose barriers to the maintenance of health. An academic dental outreach program in London, Ontario provides free comprehensive dental care to all economically-challenged individuals that have no other options for treatment. An assessment was conducted to assess the program’s impact on the geriatric population.
Materials & Methods: Data on 2156 outreach patients between 2012-2019 was analyzed to determine [1] the percentage of geriatric patients treated [2] the dental treatments that were provided [3] a comparison to the national average and [4] a comparison to other programs.
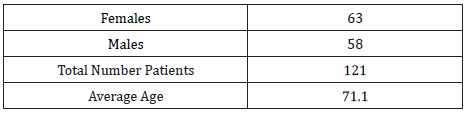
Results: Geriatric patients treated in the outreach program were 5.6% of the total patient population. There were 63 female patients, or 52%, and 58 male patients, or 48%.The average geriatric patient age was 71 years. Much of the treatment provided was limited to diagnostic and restorative procedures, consistent with the Canadian Health Measures Survey. Other options for geriatric patients are available but are limited and follow strict qualification guidelines.
Conclusion: The academic outreach program was only treating a small proportion of the geriatric population. Expanding the program to more geriatric patients was warranted. This would necessitate an increased educational footprint, additional funding, greater faculty support, heightened promotion, patient education and targeted recruitment.
Keywords:Dental Care, Ageing, Geriatric Dentistry, Oral Health
Keyword Messages
- The geriatric population in Canada is rapidly increasing
- The geriatric population experiences challenges for oral health maintenance
- An academic outreach program treats a small percentage of geriatric patients
- The program should increase its geriatric patient population
Introduction
Canada’s aging population has seen a historic increase in the last twenty years [1]. The 2016 Canadian census revealed that between 2011 and 2016, the 65 or older demographic grew by 19.9% [2]. In 2017, the Canadian population numbered 36.54 million, of which individuals 65 or older comprised 6.13 million and represented 16.8% of the population[3].It is estimated that within 10 years, Canadians aged 65 or older will rise to over 9.5 million and comprise 23% of the Canadian population [4]. The growing demographic of individuals aged 65 or older, referred to as geriatrics, and presents a unique challenge to primary and oral health care providers. Geriatric patients are more likely to have comorbid conditions, cognitive incapacities, verbal limitations and frailty, all of which [1] affect and accentuate pre-existing dental conditions and [2] pose barriers to the maintenance of health[5]. There is a significant disparity in oral health care as it is not publicly funded.The geriatric population faces reduced access to dental care due to a lack of insurance, limited income, institutionalization and reluctant clinicians[6,7].
Geriatric patients are also the largest reported demographic that have not visited a dental professional in the last year [6]. The oral cavity can be a reflection of systemic health and oral health is an integral component to overall health.Oral health also impacts individuals both physically and psychologically, and the geriatric population tends to have significant oral health concerns, based on the incidence of xerostomia, periodontitis, and caries [5,8]. Despite a greater percentage of the geriatric population retaining their natural dentition, tooth loss is still prevalent and has been associated with malnutrition, impairment of speech and a reduced quality of life[8,9]. Recent evidence has linked oral diseases to chronic systemic conditions, such as diabetes and cardiovascular disease [5]. Conversely, systemic diseases, such as cancers and gastrointestinal problems, also manifest orally, which exemplifies the necessity for dental examinations and early diagnoses[9]. The geriatric population is highly susceptible to oral diseases (Figure 1).
Individuals between 60-79 years of age experience the highest rate of edentulism (22%) although the CMHS [8] has reported a decrease in the prevalence of edentulism among Canadians, resulting in a shift from prosthetic to restorative treatment [8]. Within the CMHS-surveyed oldest cohort (60-79 years), 11% had untreated root caries, 31% had at least one periodontal pocket ≥4.0 mm, 90% had ≥1 decayed, missing or filled tooth (DMFT), and 20% had 1 or more soft tissue lesions 8,10. An academic Dental Outreach Community Service (DOCS) program, at Schulich Dentistry, is a mandatory component for dental students in their final year. The outreach program provides free dental care to low income individuals that have no other options for dental care. The program is unique, as it essentially operates as a stand-alone program and is largely supported by volunteer dental professionals. The program is a collaborative community-based effort, as many of the clinics operate at various community centres (Figure 2). An assessment was performed to assess the academic dental outreach program’s impact on the geriatric population in London, Ontario, Canada.
Materials & Methods
All outreach patient data and treatment information, since the program was implemented, was compiled into an electronic patient management software. The outreach administrator was contacted, and specific geriatric patient information was requested. Information was provided without any patient identifiers; therefore, ethics approval was not required. Analysis of the data was completed and compared to national statistics and local geriatric dental programs were examined to assess [1] the percentage of geriatric patients within the DOCS program, [2] the treatments that were delivered, [3] a comparison to the national average and [4] a comparison to other programs that may treat geriatric patients in London, Ontario.
Results
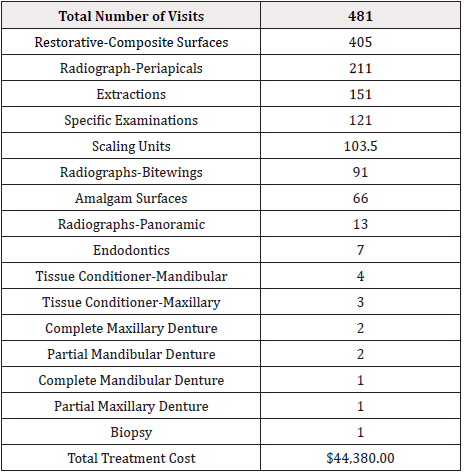
The DOCS program treated a total of 2156 patients between 2012-2019. Geriatric patients represented 5.6% (121 patients) of the total patients treated. The number of female patients were 63 and the number of male patients were 58. The average age was 71.1 (Table 1). The total number of geriatric patient visits was 481. Treatments that were provided included composite restorations (405 surfaces), periapical radiographs (211), extractions (151), specific examinations (121) and periodontal scaling (103.5). The remainder of the treatments delivered are listed in (Table 2) in descending order. The total cost of treatment delivered was $44380 CDN.
Discussion
The Schulich Dentistry DOCS program treated a small proportion of the geriatric population of 5.6%, which is well below the national percentage of 16%. Females represented 52% and males represented 48%. This represents an almost equal representation of both males and females. The average age was 71 years. There was a total of 481 visits for the 121 patients, representing almost four visits per patient. Table 2 lists dental treatments that were delivered, arranged from the most common to least common. Composite restoration was the highest, but this value considered the surfaces restored. Periodical radiographs were second, followed by extractions. Treatments were mainly composed of examinations (and radiographs), restorations and periodontal treatments, which were consistent with the CMHS [8]. It was notable that extractions were third common with a value of 151.Total treatment cost that was delivered to geriatric patients was $44380 CDN, which was a reduced fee of approximately 40%, based on the Schulich Dentistry fee guide [10].
There are currently three other programs offering dentistry to geriatric patients, with strict qualification guidelines.
- Parkwood Institute provides services for current inpatients or registered outpatients, including those in the Veterans Care Program, Mental Health Care Program and Southwest Centre for Forensic Mental Health Care. Treatments include examinations, periodontics, prosthodontics, endodontics and oral surgery. Service payment is through social assistance dental coverage, Ontario Health Insurance Plan (OHIP), a reduced fee or free (for inpatients).
- Ontario Seniors Dental Care Program is publicly funded and provides care for individuals65 years or older who have no dental benefits, a single income of less than $19,300 or a combined couple’s income of less than $32,300 [12]. Services are accessed via public health units, community health centres, and Aboriginal Health Access Centres [12]. Many municipalities lack these units and centres, limiting access.
- OHIP covers some dental services, if procedures are performed in an acute care hospital when hospitalization is medically [13]. Services include oral and maxillofacial surgery, for high risk patients13.
London’s geriatric population continues to grow and is expected to more than double by 2036 [11]. The geriatric population in London continues to increase, so will the need for dental services. Increased awareness of the DOCS program, through education, promotion, and targeted recruitment, could address the shortcomings presently observed. Any expansion of the program would require an increased educational footprint, additional funding and greater faculty support. The geriatric population in Canada, specifically in London, is increasing at an unpreceded rate and so will the demands for dental care. With limited programs available and strict qualifications, the geriatric patient population will continue to experience barriers to oral health care. This is a vulnerable population with unique barriers to oral health care. The DOCS program has the potential to expand and provide additional services, but increased educational and promotional campaigns, with appropriately expanded resources, are essential for the intervention.
The assessment of the outreach program indicated that it has been inadequate at serving the geriatric population and should increase its commitment to this vulnerable community.
References
- E Grenier (2017) Canadian seniors now outnumber children for 1st time, 2016 census shows.
- (2017)Ministry of Finance. 2016 census highlights: factsheet 3.
- (2020)Statistics Canada. Seniors and aging statistics.
- (2014) Government of Canada. Action for seniors report.
- Coll PP, Lindsay A, Meng J (2019) the prevention of infections in older adults: oral health. J Am Geriatr Soc 68(2): 411-416.
- (2019)Statistics Canada. Health fact sheets: dental care, 2018.
- Marvin MF (2001) Access to care for seniors—dental concerns. J Can Dent Assoc 67(9): 504-506.
- Government of Canada (2010) Report on the findings of the oral health component of the Canadian health measures survey 2007-2009.
- Yao CS, MacEntee MI (2014) Inequity in oral health care for elderly Canadians: part 2.Causes and ethical considerations. J Can Dent Assoc 80: e10.
- Yao CS, MacEntee MI (2013) Inequity in oral health care for elderly Canadians: part 1. Oral health status. Can Dent Assoc 79: d114.
- (2013)Middlesex London Health Unit. Healthy aging.
- (2019)Dental Care for Low-Income Seniors. Government of Ontario: Ministry of Health.
- (2020)Ministry of Health and Long-Term Care. Schedule of benefits. Dental services under the Health Insurance Act (April 1, 2012).




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.