Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Case Report: Spontaneous Leg Swelling Due to Acquired Factor VIII Deficiency in an Older Patient
*Corresponding author: Barbara Helen Rosario, Changi General Hospital, 2 Simei Street 3, 529889, Singapore.
Received: October 12, 2020;Published: November 10, 2020
DOI: 10.34297/AJBSR.2020.10.001569
Abstract
This case report describes a rare cause of leg swelling and highlights the importance of investigation of what may appear to be a minor blood abnormality.
Keywords: Acquired Factor 8 Deficiency, Acquired Haemophilia, Falls, Haematoma.
History
An 82-year-old male presented with a 2-day history of worsening right leg pain. There was no history of trauma or fall. There was no evidence of sepsis, no fever or increase in temperature at the site of the swelling. His mobility was limited by pain and swelling. There was no recent change in his medications and no intake of traditional Chinese medicines. There was no history of weight loss or loss of appetite. Pre-morbidly he required assistance with his daily activities; however, he was home ambulant with a walking stick. He had been investigated for anaemia and recently diagnosed with a myeloproliferative disorder associated with thrombocytosis, eosinophilia and the presence of a positive JAK2 mutation, which indicated a non-chronic myeloid leukemia myelop roliferative disorder. Past medical history included Alzheimer’s dementia with behavioural and psychological symptoms of dementia, benign prostatic hyperplasia, falls and cervical myelopathy.
On examination there was generalised swelling of the right thigh with tenderness on palpation but no surrounding erythema or evidence of cellulitis. Femoral, popliteal, posterior tibial and dorsalis pedis were palpable bilaterally. Extensive bruising was present over the right popliteal fossa and a bedside ultrasound demonstrated that the femoral and popliteal veins were patent and compressible. Well’s score was 3. There was no evidence of a deep vein thrombosis, but the ultrasound noted a solid cystic lesion in the adductor muscle of the medial thigh, likely a haematoma.
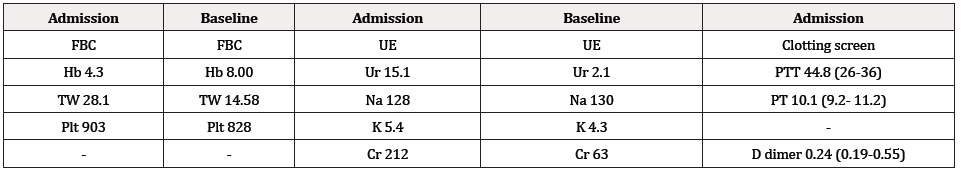
Initial Investigations
Initial investigations are shown in Table 1. Due to hypotension, he received a fluid challenge and 3-unit blood transfusion. A further 2 units of blood were required over the following 3 days. An acute kidney injury was noted and improved with intravenous fluids. After 3 days he developed fever and was commenced on antibiotics for a likely infected haematoma. In view of increasing drowsiness, a CT head was performed as shown in Fig 1, with no evidence of cerebral haemorrhage.
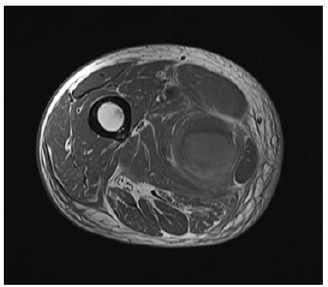
MRI Scan
A magnetic resonance scan (MRI), shown in Fig 2, was performed and confirmed an elongated lobulated soft tissue mass in the right adductor compartment (25cm x 4cm x 4cm), most likely a post traumatic hematoma from muscle tears. He was reviewed by the orthopaedic team who were concerned that the hematoma was infected and scheduled him for emergency surgery. There was no evidence of compartment syndrome. He subsequently developed a swollen left wrist, followed by a large area of bruising over the right posterior chest wall area with further bruising extending into the scrotum. In view of the deranged clotting (activated partial thromboplastin time, aPTT at 44.8 (range 26-36)) and the increasing haematomas, further evaluation was undertaken (Figure 1-2).
Progress
Haematology advice was sought and advised that the prolonged aPTT was likely due to acquired Factor 8 deficiency (acquired Haemophilia). Lupus anticoagulant was negative, and aPTT 50% correction (partially correctable). The initial Factor 8 assay was <1 and the factor 8 inhibitor assay were 12 Bethesda units. Anti-nuclear antibodies and anti-double stranded DNA were negative. Treatment was initiated with prednisolone and cyclophosphamide. Despite the earlier correction of his Haemoglobin (Hb), he developed a further precipitous drop to Hb 4.4, requiring a four-unit blood transfusion. Due to the drop in Hb, Novoseven, a recombinant Factor 7 that combines with tissue factor to activate Factor 10, therefore bypassing the need for Factor 8 was administered. Novoseven was given as a lifesaving treatment as this was available immediately within the hospital. Another option for treatment was Feiba, that contains activated coagulation factors from human plasma which he received following transfer to the specialist Haematology care. Following immunosuppressive treatment, the repeat Factor 8 assay was 72 (normal 55-200) and the Factor 8 inhibitor was no longer detected resulting in normalisation of the aPTT. The patient did not require surgery and was discharged home with a plan to tail down the steroid treatment.
Discussion
Acquired Factor 8 deficiency (Acquired Haemophilia) has been reported in an older population [1] with a roughly equal incidence in men and women [2]. It has a high rate of mortality and morbidity [3] (7.9-22%) and as many as 73% present initially with a severe life-threatening bleed [10]. The presentation can be diverse with cases of compartment syndrome [3], profound haematuria [4] excessive bleeding post-surgery and gastro-intestinal bleeding [5] Acquired Factor 8 deficiency has also presented with tongue swelling, initially thought to be angioedema [6].
Acquired Factor 8 deficiency (Acquired Haemophilia) arises from the presence of auto-antibodies or inhibitors directed against clotting factors, most often Factor 8 [4]. Development of immune- mediated auto-antibodies against Factor 8 is associated with a wide range of clinical disorders including malignancy, pregnancy and autoimmune disorders [7]. The hallmark of this disorder is an isolated prolonged aPTT in the absence of any other abnormality of clotting [4]. Treatment options include steroids and cyclophosphamide, for low risk patients and for higher risk or bleeding patient’s treatment with Feiba, a plasma derived activated pro-thrombin complex concentrate and NovoSeven are used. NovoSeven is a recombinant bypassing agent available for the treatment of bleeding episodes in patients with acquired haemophilia [8]. A further treatment to consider would be the Bonn protocol which involves large volume immunoadsorption, intravenous immunoglobulin substitution as well as immunosuppression with cyclophosphamide and prednisolone and administration of Factor 8 [10]. Following immunosuppressant therapy, effective inhibitor eradication leads to an increase of the 5 years survival rate from 37% to 71% [9].
In this older patient with dementia and a history of falls, bleeding into soft tissues, as described above, is common presentation and could have led to a surgical procedure if appropriate investigation of his derangement of clotting had not been pursued. The blood loss was significant and a potentially life-threatening complication of acquired Factor 8 deficiency, which should be considered as differential diagnosis in the presence of an isolated prolonged aPTT.
References
- Calle A, AC Gama, LM Perez, MA Marquez, M Pi-Figueras, et al. (2013) Acquired hemophilia in a nonagenarian: a case report. Journal the American Geriatrics Society 61(11): 2056-2057.
- Knoebl P, P Marco, F Baudo, P Collins, A Huth-Kuhne, et al. (2012) Demographic and clinical data in acquired hemophilia A: results from the European Acquired Haemophilia Registry (EACH2). J Thromb Haemost 10(4): 622-631.
- Pham TV, CA Sorenson, JV Nable (2014) Acquired factor VIII deficiency presenting with compartment syndrome. Am J Emerg Med 32(2): 195.e1-2.
- Shander A, C Walsh H Bailey, C Cromwell (2013) Acquired hemophilia presenting as profound hematuria: evaluation, diagnosis, and management of elusive cause of bleeding in the emergency department setting. J Emerg Med 45(1): e1-6.
- Franchini M, G Gandini, T Di Paolantonio, G Mariani (2005) Acquired hemophilia A: a concise review. Am J Hematol 80(1): 55-63.
- Demissie A, L Shahani, A Khan, M Desai (2013) Acquired haemophilia A initially diagnosed as angioedema. BMJ Case Rep.
- Sborov DW, GM Rodgers (2013) How I manage patients with acquired haemophilia A. Br J Haematol 161(2): 157-165.
- Huth-Kuhne A, F Baudo, P Collins, Ingerslev J, CM Kessler, et al. (2009) International recommendations on the diagnosis and treatment of patients with acquired hemophilia A. Haematologica 94(4): 566-575.
- Baudo F, P Collins A Huth-Kuhne, H Levesque, P Marco, L Nemes, et al. (2012) Management of bleeding in acquired hemophilia A: results from the European Acquired Haemophilia (EACH2) Registry. Blood 120(1): 39-46.
- Zeitler H, G Goldmann, N Marquardt, G Ulrich-Merzenich (2013) Long term outcome of patients with acquired haemophilia--a monocentre interim analysis of 82 patients. Atheroscler Suppl 14(1): 223-228.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.