Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Greater Flow Diversion with the LVIS Stent vs the Enterprise Stent Regarding Basilar Tip Aneurysm Hemodynamics
*Corresponding author: Chao Sun, Binzhou Medical University Hospital, No. 661 Second Huanghe Road, Binzhou, Shandong, China. Jian Liu, Beijing Neurosurgical Institute and Beijing Tiantan Hospital, Capital Medical University, TiantanXili 6, Dongcheng District, Beijing, China.
Received: August 19, 2020; Published: September 11, 2020
DOI: 10.34297/AJBSR.2020.10.001499
Abstract
Objective: Computational fluid dynamics (CFD) has been widely used to investigate the intra-aneurysmal hemodynamic alteration after stent implantation. The aim of this study was to quantify the flow diverting difference of the new LVIS stent compared with the conventional Enterprise stent and various stent configurations in basilar tip aneurysms using CFD.
Methods: In this research, we simulated six basilar tip aneurysms constructed from 3D digital subtraction angiography (DSA). The LVIS and Enterprise stent combined with three stent configurations (Left half-Y, right half-Y and Y) were virtually conformed to fit into the vessel lumen and placed across the aneurysm orifice. Computational fluid dynamics analysis was performed to compare the hemodynamic differences among these stents.
Results: All the hemodynamic changes were compared to the untreated aneurysm (Control). The LVIS stent produced more wall shear stress (21.59% vs 11.6%) and velocity (12.2% vs 7.31%) reduction than the Enterprise stent compared. The left half-Y stent configuration, which was usually deployed first clinically, demonstrated a better flow diversion effect than the right half-Y. However, most of the reduction in wall shear stress (40.08%) velocity (20.12%) and pressure increase was observed in the Y stent configuration.
Conclusion: This study confirmed the better flow diverting effect of LVIS stent than Enterprise stent. The left half-Y stent configuration resulted in a more wall shear stress (WSS), velocity decrease and Pressure increase than the right half-Y stent configuration while the Y stent configuration demonstrated the most.
Keywords: Computational Fluid Dynamics, Stent Configuration, Wall Shear Stress, Intracranial Aneurysm, Hemodynamics
Abbreviations: CFD: Computational Fluid Dynamics; WSS: Wall Shear Stress; LVIS: Low-profile Visualized Intraluminal Support
Introduction
The interventional technique for treating intracranial aneurysm including coiling, stent-assisted coiling and Flow diverter (FD)-Pipeline device. Traditional coiling was mainly used in the treatment of narrow-neck aneurysm, limited its use to wide-neck aneurysm, an alternative stent-assisted coiling was invented and proved to have a lower recurrence rate vs conventional coiling [1]. The Pipeline device was known to have the advantages in treating large or giant wide-neck aneurysm, while its indication was limited in the internal carotid artery from the petrous to the superior hypophyseal segments and not all the institutions had the authority to use it [2,3]. A novel braided stent with broader indication (especially for the treatment of posterior circulation aneurysms): the Low-profile Visualized Intraluminal Support stent (LVIS; MicroVention, Tustin, California, USA) with small cell structure (0.9 mm) and high metal coverage (23%) between conventional Enterprise stent (10%) and FD-Pipeline (30%-35%) was invented and has been widely used in the treatment of wide-neck aneurysm [2-4]. Like the implantation of FD, we can use the push-pull technique to improve the metal coverage at the aneurysm orifice, thus maximizing the flow diverting effect [4]. Meanwhile, the LVIS stent still performed a safe and effective treatment outcome in the clinical and angiographic follow-up research [5-7].
The main function of stent is not only preventing coil herniation, but also impact the intracranial aneurysm hemodynamics. For the posterior circulation aneurysms, especially the basilar tip aneurysm, various stent configurations including half-Y Y crossbar and T could be implanted. Previous hemodynamic studies demonstrated obvious differences between Enterprise stent configurations in wide-necked basilar tip aneurysms [8]. However, compared to the Enterprise stent, the LVIS stent has lower recanalization rate and a higher occlusion rate [2,3]. Some experts might be interested in the hemodynamic difference after LVIS implantation. Therefore, in our study, we used a virtual stenting technology and computational fluid dynamics (CFD) simulation, to elucidate the influence of three LVIS and Enterprise stent configurations (left half-Y, right half-Y, and Y) on cerebral aneurysm fluid dynamics in six virtual wide-necked basilar tip aneurysms.
Methods
Aneurysm
We simulated six basilar tip aneurysms constructed from 3D digital subtraction angiography (DSA). Two morphological parameters measured by DSA were summarized: Neck Width represented the largest axial diameter at the orifice of the aneurysm; Aneurysm Size was defined as the length from the neck center to the dome of the aneurysm. Case 1 involved an aneurysm with a neck width of 6.41 mm and an aneurysm size of 6.72 mm; Case 2 involved an aneurysm with a neck width of 6.15 mm and an aneurysm size of 3.36 mm; Case 3 involved an aneurysm with a neck width of 9.18 mm and an aneurysm size of 11.35 mm; Case 4 involved an aneurysm with a neck width of 12.52 mm and an aneurysm size of 7.87 mm; Case 5 involved an aneurysm with a neck width of 2.72 mm and an aneurysm size of 1.88 mm; Case 6 involved an aneurysm with a neck width of 4.54 mm and an aneurysm size of 3.21 mm; The medical data were recorded for diagnostic purposes, and the study was approved by the Ethics Committee of our institution.
Stent Modeling and Deployment
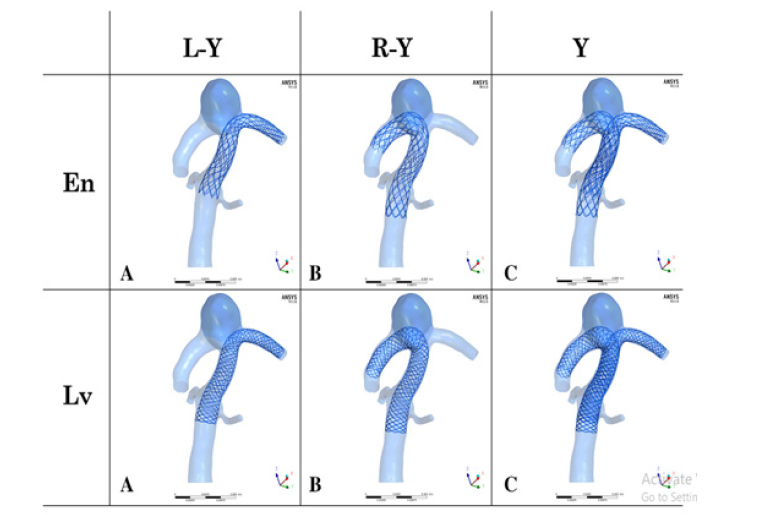
Figure 1: A left-half Y (L-Y), B right-half Y (R-Y) and c Y stent configurations; Note: En Enterprise stent and LvLvis stent.
In our simulations, a novel virtual stenting workflow [8,9] was used to deploy the Enterprise and LVIS stents (Figure 1). The simulation consists of the following three steps: (1) Pre-processing, which separates the parent artery from the aneurysm, and produces a simplex mesh structure along the vessel centerline position; (2) Simplex mesh expansion, where the simplex mesh structure experience radial expansion, and the expansion stops when the simplex mesh has good adherence to the parent artery wall; and (3) Post-processing, which maps the stent structure on the simplex mesh, and transforms the stent wires into three-dimensional structures.
CFD Modeling
CFD modeling with an unsteady blood flow was performed by the finite volume method using ANSYS CFX 14.0 (ANSYS, Inc., Canonsburg, PA). Mesh dependency tests, which contained approximately 2 to 40 million tetrahedral elements was used to ensure the stability of the calculation. Blood was considered as an incompressible Newtonian flow with a viscosity of 0.004 kg/m/s and a density of 1060 kg/m3. Vessel wall was assumed to be a rigid and no-slip boundary pattern. The pressure distribution along the vessel wall was then computed using the decreases in pressure calculated based on the P=10,000Pa value set at the outlet [10]. A mean inlet WSS of 1.5Pa was scaled to the flow waveforms. The flow conditions were advanced in time using 0.001 seconds for two cycles [11]. The results of the second cycle were assumed for hemodynamic characterization (e.g., the WSS). We then post-processed and visualized the results of these simulations with the ANSYS CFD-Post.
Statistical Analysis
If normally distributed, all recorded data were summarized as mean ± SD, and analyzed with paired-samples or independent-samples t-tests. If not normally distributed, all recorded data were summarized as median (interquartile range) and analyzed with paired Wilcoxon tests. P <0.05 was regarded as statistically significant. Statistical analysis was performed with SPSS 17.0.
Results
The tilted orifice of the aneurysm mainly determined the location of the first clinical implanted stent, thus we defined it as the left half-Y configuration. The secondary stent configuration was defined as the right half-Y configuration. Without any stent, the blood flow entered the aneurysm dome from the left to proximal neck with a counterclockwise direction, and the main flow direction of pre-operation was toward to the left PCA from the inlet. After stenting, the flow condition was suppressed with gradually lower strength and decreased WSS or velocity (Figure 2).

Figure 2: A Control, B left-half Y (L-Y), C right-half Y (R-Y) and D Y stent configurations; R-Y caused only a small change in the overall intra-aneurysm flow pattern compared with Control. L-Y produced a more obvious flow reduction than R-Y. While Y showed the most evident WSS and flow velocity reduction compared with other stent configurations. The Streamline pattern seen in Control persists with the gradually lower intensity after stenting similar to the WSS and velocity changes. Meanwhile, Lv showed a better flow diversion effect than En within the same stent configuration.
Note: En Enterprise stent, Lv Lvis stent and WSS wall shear stress.
Compare Aneurysms by Stents (En vs Lv)
Both WSS and flow velocity decreased after stent implantation. With the same stent configuration like Left half-Y, although the Enterprise stent showed relatively obvious decreases, from 3.640Pa±2.246Pa to 3.217Pa±2.452Pa, a 11.6% reduction (P=0.138) and from 0.164m/s±0.123m/s to 0.152m/s±0.131m/s, a 7.31% reduction (P=0.152) in WSS and flow velocity. The LVIS stent, produced a more obvious flow reduction than the Enterprise stent, 2.854Pa±2.413Pa and 0.144m/s±0.124m/s, a 21.59% (P=0.03) and a 12.2% (P=0.038) reduction respectively, the changes were statistically significant (P<0.05). The overall pressure increased less than 1% after stent implantation. However, the LVIS stent indicated a pressure increase than the Enterprise stent (10247.633Pa±223.064Pa vs 10245.217Pa±214.198Pa) (Table 1 & 2).
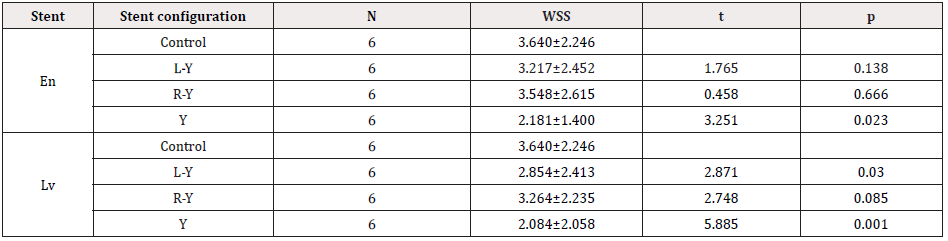
Table 1: Hemodynamic changes after stent placement (WSS).
Control was analyzed with paired-samples t-tests among left-Y, right-Y and Y stent configurations, respectively. L-Y left half-Y stent configuration, R-Y right half-Y stent configuration, Y Y stent configuration, En Enterprise stent. LvLvis stent, WSS wall shear stress.
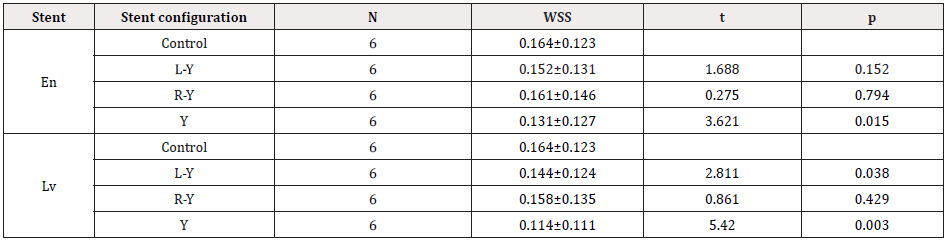
Table 2: Hemodynamic changes after stent placement (Velocity).
Control was analyzed with paired-samples t-tests among left-Y, right-Y and Y stent configurations, respectively. L-Y left half-Y stent configuration, R-Y right half-Y stent configuration, Y Y stent configuration, En Enterprise stent, LvLvis stent, WSS wall shear stress.
Compare Aneurysms by Stent Configurations (L-Y vs R-Y vs Y)
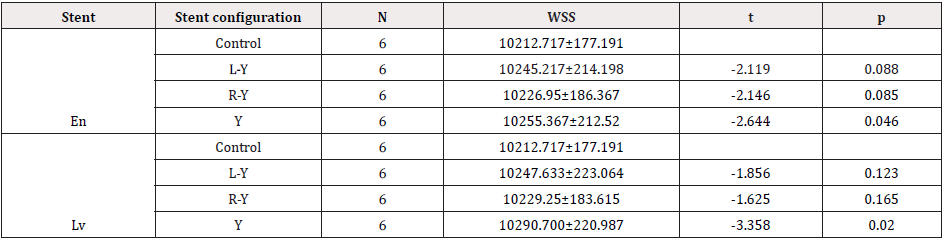
Table 3: Hemodynamic changes after stent placement (Pressure).
Control was analyzed with paired-samples t-tests among left-Y, right-Y and Y stent configurations, respectively. L-Y left half-Y stent configuration, R-Y right half-Y stent configuration, Y Y stent configuration, En Enterprise stent,LvLvis stent, WSS wall shear stress.
With the same stent as Enterprise. The right half-Y stent configuration caused only a small change compared with the Control, the values of WSS and velocity changed from 3.640Pa±2.246Pa to 3.548Pa±2.615Pa, a 2.52% reduction (P=0.666) and from 0.164m/s±0.123m/s to 0.161m/s±0.146m/s, a 1.83% reduction (P=0.794). The left half-Y, which is usually deployed as the first stent clinically, the WSS and velocity demonstrated a more obvious reduction of 11.6% and 7.31%. However, the Y stent configuration showed the highest WSS and flow velocity reductions 40.08% (P=0.023) and 20.12% (P=0.015) respectively. An opposite pressure increases were also observed in Table 3. Meanwhile, the hemodynamic changes after Y stent configuration were all statistically significant, which meant the most obvious reduction in WSS Velocity and increase in Pressure.
Discussion
Although the advances in endovascular devices and techniques, treatment for aneurysm with wide-neck or irregular morphologies was still challenging. The LVIS stent, which is self-expanding and braided stent with compliant cells, has broadened the scope of endovascular therapy in IAs of the Pipeline device: aneurysms arising from a parent vessel with a diameter >2.5mm and <4.5mm, which means a promise in treating more types or locations of the aneurysms [2-5]. Our study of six basilar tip aneurysm treated with LVIS and Enterprise stent combined with three stent configurations (Left half-Y, Right half-Y and Y), demonstrated that the LVIS stent provided better flow diversion vs the Enterprise stent, which might resulted from the smaller cell size (0.9mm) and higher metal coverage (23%) of LVIS stent. Compared with our previous study on hemodynamic alterations for various Enterprise stent configurations in one idealized basilar tip aneurysm [8], the current result seemed more valuable because of a bigger sample size. In the clinical application, intracranial aneurysms treated with LVIS stent has gained favorable neurological outcomes. Poncyljusz et al. [12] and Cheung et al. [7] demonstrated a safe and effective therapy option of the LVIS stent in a short term (6 months) and long term (18 months) clinical and radiological follow-up, respectively. The main function for endovascular treatment is to lower the recurrence rate and prevent postoperative complications. Thus, in order to better assess the effect and prognosis after the endovascular treatment, many evaluation indicators such as the occlusion rate recanalization rate and thromboembolic rate were analysed in the follow-up research. Ge et al. [2] reported a series of 190 cases that treated with LVIS or Enterprise stents, the LVIS stent achieved a greater complete or near-complete occlusion rate than Enterprise stent (96.9% vs 88.4%). Feng et al. [3] showed that LVIS stents might achieve a lower recanalization rate (8% vs 13.5%) and thromboembolic rate (10.2% vs 16.8%) than Enterprise during the angiographic follow-up. Zhang et al. [5] demonstrated that the overall rate of thromboembolic complication was 4.9%, and the symptomatic thromboembolic complication was only 2.4%. However, FD has been proved that the perforator vessel (especially the ophthalmic artery and posterior communicating artery) could be kept patent when treating intracranial large or giant aneurysm [13-16]. These similar braided stents, high metal coverage at the orifice of the aneurysm could be achieved when deployed with the push-pull technique in the artery, thus preserving the perforator vessels with low metal coverage or patent, this may be the reason why FD or LVIS showed a non or low thromboembolic rate after stenting. In the hemodynamic research, WSS is a measurement of the friction force between the blood flow and vessel wall, and this friction force plays an important role in the recurrence of aneurysms. Low velocity and WSS area promote the thrombosis procedure [20,21]. Previous hemodynamic studies on the Y stent configuration mainly focused on the conventional Enterprise or Neuroform stent. Canton, et al. [17] measured a reduction of 11 % following a Y configuration Neuroform stent deployment in a realistic cerebral aneurysm model. Appanaboyina, et al. [18] simulated half-Y and Y Neuroform stent deployments on basilar artery tip aneurysm models and found a reduction in aneurysmal velocity and WSS either. We previously studied the hemodynamic effect after four Enterprise stent configurations implantation and concluded that all of the stent configurations showed a velocity and WSS reduction and pressure increase, cross-bar configuration reduced velocity and WSS within the aneurysm most while a Y configuration increased pressure most [8], this result was a little different from our current research. Regarding to the hemodynamic between Enterprise and LVIS stenting, similar to our current results, we previously found that a single LVIS stent resulted in more flow diverting effect than the double-Enterprise stent, but less than a Pipeline device. Nevertheless, the double-LVIS stent caused a better flow reduction than a Pipeline device [19]. The low recanalization rate and thromboembolic rate after LVIS stenting may be explained by CFD. Liu et al. [20] and Jing et al. [21] found that obviously decreased flow velocity and WSS at the aneurysmal neck may be an important factor in preventing recanalization. li et al. [22] observed a velocity reduction of flow in an aneurysm (40.6%) with only a slight impact on branch velocity (10%), and these results may be the explanation for aneurysms being occluded while branches remain patent. Meanwhile, the mesh compaction at the aneurysmal orifice with the lower metal coverage at the perforator regions for this braided structure also promoted the happening of low thromboembolic rate. The most important limitations of this study include, (a) we did not evaluate coiling, which is a crucial factor in aneurysm treatment; (b) small sample size, which requires confirmation of the results with larger series of different aneurysmal locations; and (c) lack of patient-specific flows, which can affect the exact values of the boundary setting. In addition, the assumption that the hemodynamic factors avoid complications and leads to a successful outcome may be not persuasive and other factors should be further investigated. Despite these limitations, interesting associations among different stent configurations of LVIS stent are primarily identified. This could provide some theoretical reference instruction for choosing the therapy option of Y-LVIS stenting.
Conclusion
This study confirmed the better flow diverting effect of LVIS stent than Enterprise stent. The left half-Y stent configuration resulted in a more WSSvelocity decrease and Pressure increase than the right half-Y stent configuration while the Y stent configuration demonstrated the most.
Acknowledgments
Not applicable.
Conflict of Interest
The authors declare that they have no conflict of interests.
Funding
This work was supported by National Natural Science Foundation of China (No. 81571128), Shandong Province Natural Science Foundation of China (No. ZR2017LH033), Binzhou Medical University Scientific Research Foundation (No. BY2016KYQD15).
References
- Hong Y, Wang YJ, Deng Z, Wu Q, Zhang JM (2014) Stent-Assisted Coiling versus Coiling in Treatment of Intracranial Aneurysm: A Systematic Review and Meta-Analysis. PlosOne 9(1): e82311.
- Ge H, Lv X, Yang X, He H, Jin H, et al. (2016) LVIS Stent Versus Enterprise Stent for the Treatment of Unruptured Intracranial Aneurysms. World Neurosurgery 91: 365-370.
- Feng X, Qian Z, Liu P, Zhang B, Wang L, et al. (2018) Comparison of Recanalization and In-Stent Stenosis Between the Low-Profile Visualized Intraluminal Support Stent and Enterprise Stent-Assisted Coiling for 254 Intracranial Aneurysms. World Neurosurgery 109: e99-e104.
- Ma D, Xiang J, Choi H, Dumont TM, Natarajan SK, et (2014) Enhanced Aneurysnal Flow Diversion Using a Dynamic Push-Pull Technique: An Experimental and Modeling Study. Am J Neuroradiol 35: 1779-1785.
- Zhang X, Zhong J, Gao H, Xu F, Bambakidis NC (2016) Endovascular treatment of intracranial aneurysms with the LVIS device: a systematic review. J NeuroIntervent Surg 9(6): 553-557.
- Wang CC, Li W, Feng ZZ, Hong B, Xu Y, et al. (2017) Preliminary Experience with Stent-Assisted Coiling of Aneurysms Arising from Small (<2.5mm) Cerebral Vessels Using the Low-Profile Visualized Intraluminal Support Device. Am J Neuroradiol 38: 1163-1168.
- Cheung NK, Chiu AH, Cheung A, Wenderoth JD (2017) Long term follow-up of bifurcation aneurysms treated with braided stent assisted coiling and complex T- and Y- stent J NeuroIntervent Surg 10(6): 560-565.
- Wang C, Tian Z, Liu J, Jing L, Paliwal N, et al. (2016) Hemodynamic Alterations for Various Stent Configurations in Idealized Wide-neck Basilar Tip Aneurysm. J Med Biol Eng 36: 379-385.
- Paliwal N, Yu H, Xu J, Xiang J, Siddiqui A, et (2016) Virtual stenting workflow with vessel specific initialization and adaptive expansion for neurovascular stents and flow diverters. Comput Methods Biomech Biomed Engin 19(13): 1423-1431.
- Kim M, Taulbee DB, Tremmel M, Meng H (2008) Comparison of two stents in modifying cerebral aneurysm hemodynamics. Ann Biomed Eng 36: 726-741.
- Mut F, Aubry R, Lohner R, Cebral JR (2010) Fast Numerical Solutions of Patient-Specific Blood Flows in 3D Arterial Systems. Int J Numer Method Biomed Eng 26(1): 73-85.
- Poncyljusz W, Biliński P, Safranow K, Baron J, Zbroszczyk M, et al. (2014) The LVIS/LVIS stents in the treatment of wide- neck intracranial aneurysms: multicentre registry. J NeuroIntervent Surg 7(7): 524-549.
- Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, et (2011) The pipeline embolization device for the intracranial treatment of aneurysms trial. Am J Neuroradiol 32: 34-40.
- Szikora I, Berentei Z, Kulcsar Z, Marosfoi M, Vajda ZS, et (2010) Treatment of intracranial aneurysms by functional reconstruction of the parent artery. the Budapest experience with the pipeline embolization device. Am J Neuroradiol 31: 1139-1147.
- Fischer S, Vajda Z, Aguilar Perez M, Schmid E, Hopf N, et (2012) Pipeline embolization device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology 54: 369-382.
- Puffer RC, Kallmes DF, Cloft HJ, Lanzino G (2012) Patency of the ophthalmic artery after flow diversion treatment of paraclinoid aneurysms. J Neurosurg 116: 892-896.
- Canton G, Levy DI, Lasheras JC (2005) Hemodynamic changes due to stent placement in bifurcating intracranial aneurysms. J Neurosurg 103: 146-155.
- Appanaboyina S, Mut F, Lohner R, Putman C, Cebral J (2009) Simulation of intracranial aneurysm stenting: Techniques and Computer Methods in Applied Mechanics and Engineering 198: 3567-3582.
- Wang C, Tian Z, Liu J, Jing L, Paliwal N, et (2016) Flow diverter effect of LVIS stent on cerebral aneurysm hemodynamics: a comparison with Enterprise stents and the Pipeline device. Journal of Translational Medicine 14(1): 199.
- Liu J, Jing L, Wang C, Paliwal N, Wang S, et (2016) Effect of Hemodynamics on Outcome of Subtotally Occluded Paraclinoid Aneurysms after Stent-Assisted Coil Embolization. J Neurointerv Surg 8(11): 1140-1147.
- Jing L, Liu J, Zhang Y, Paliwal N, Meng H, et al. (2016) Analysis of Multiple Intracranial Aneurysms with Different Outcomes in the Same Patient After Endovascular World Neurosurg 91: 399-408.
- Li W, Liu J, Zhang Y, Wang K, Tian Z, et (2017) Flow diversion and Outcomes of Vertebral Fusiform Aneurysms after Stent-Only Treatment: A Hemodynamic Study. World Neurosurg 107: 202-210.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.