Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Hyperventilation-Apnoea Syndrome in a 79-year Old Woman with Congestive Heart Failure
*Corresponding author: Daniela Boisteanu, Department of Pneumology, University of Medicine and Pharmacy “Grigore T Popa” Iasi, Romania
Received: August 24, 2020; Published: August 28, 2020
DOI: 10.34297/AJBSR.2020.08.001483
Abstract
We report the case of a 79-year woman admitted for daily episodes of sudden breath arrest abruptly occurred one month prior to hospital presentation. These episodes are preceded by hyperventilation due to physical activity, especially when working in bending forward position. She was diagnosed and treated for high blood pressure, coronary heart disease, major left bundle branch block, congestive heart failure, obesity, hypercholesterolaemia and hypothyroidism. Spirometry was normal, chest x-ray showed features of basal bilateral pulmonary fibrosis, overnight respiratory polygraphy revealed moderate obstructive sleep apnoea, while cerebral magnetic resonance imaging showed a right ventrolateral compression of the medulla oblongata – spinal cord junction by a dominant, sinuous right vertebral artery, and loss of foramen magnum cerebrospinal fluid due to low lying cerebellar tonsils tips, while cisterna magna is still visible. The rare breathing pattern of our patient is reported in the literature as hyperventilation-apnoea syndrome and we discuss the potential mechanisms underlying this condition.
Keywords: Hyperventilation-apnoea Syndrome, Congestive heart failure, Vertebral artery, Medulla spinal cord junction, Foramen magnum 3.
Abbreviations: CPAP: Continuous Positive Airway Pressure; CSA: Central Sleep Apnoea; Csf: Cerebrospinal Fluid; DRG: Dorsal Respiratory Group; FEV1: Forced Expiratory Volume In 1 Second; FVC: Forced Vital Capacity; HAS: Hyperventilation-Apnoea Syndrome; MRI: Magnetic Resonance Imaging; OSA: Obstructive Sleep Apnoea; PAG: Periaqueductal Gray; SACO2: Arterial Carbon Dioxide Saturation; SAO2: Arterial Oxygen Saturation; SPO2 – Oxygen Saturation Measured By Pulse Oximetry; STN: Subthalamic Nucleus; VA: Vertebral Artery; VBD: Vertebrobasilar Dolichoectasia; VRG: Ventral Respiratory Group
Introduction
Respiration is a vital function, important in maintaining physiological homeostasis, and it is primarily regulated for metabolic and homeostatic purposes in the brainstem [1]; the final respiratory output depends on a complex interaction between the brainstem and the high centres, including the limbic system and the cortical structures [2]. Studies in animals and humans have established that sites of interest for the exercise hyperpnoea are located the midbrain, particularly in the subthalamic nucleus (STN) and the periaqueductal gray (PAG). The lateral and dorsal lateral regions of PAG, having functional connectivity to higher centres (dorsal lateral prefrontal cortex) and the basal ganglia (especially with STN), receives inputs from contracting muscles and sends outputs to the brainstem nuclei involved in cardiorespiratory control [2].
The neurons that have both inspiratory and expiratory activity and generate the automatic respiratory rhythm are located in a region of the brainstem called medulla oblongata; this area of the brain is recognized as the central pattern generator. The medulla respiratory neurons are organized in two groups: the dorsal respiratory group (DRG), controlling mostly the inspiratory movements and their timing and the ventral respiratory group (VRG), containing both inspiratory and expiratory neurons, as well as the cells that innervate the muscles that control the larynx and the pharynx [3]. The central pattern generator receives afferent information from mechanoreceptors and chemoreceptors. Information arising from periphery travels to the brain and the status of gas exchanger is closely watched so that controller reacts at decreasing in PaO2 and increasing in PaCO2. Sensory inputs from the upper airways, lungs and peripheral receptors travels up the ninth and tenth cranial nerves to the DRG located in the medulla [3].
Ventilation changes little as the PaO2 decreases from the 95 to 60 mmHg, but at this point ventilation starts to increase. Contrarily to the ventilatory response to hypoxemia, ventilation increases linearly with acute increase in PaCO2 [3]. In healthy individual high values of carbon dioxide in the blood constitute the stimulant factor for respiratory centres which respond by increasing the respiratory drive. Hyperventilation decreases the level of carbon dioxide in the blood leading to a reduced stimulation of medulla oblongata centres and central apnoea. Efferent information from DRG and VRG goes to the cervical spine cord and then through the phrenic and intercostals nerves to the diaphragm, intercostals muscles, as well to the accessory muscles like sternocleidomastoid and abdominal muscles [3].
In central sleep apnoea (CSA) there is a cessation of air flow without any respiratory effort due to a temporary reduction in, or cessation of, central respiratory drive [4,5]; in obstructive sleep apnoea (OSA) there are ongoing respiratory efforts during air flow stops due to the collapse of pharynx [4,5], but it is described a considerable overlap in the pathogenesis and clinical appearance of CSA and OSA [4]. Identification of the underlying pathophysiological mechanisms is of extreme importance in making a treatment decision [4]. Lately has become clear that CSA and OSA often coexist in the same patient, the existence of one can predispose to the other, and it seems that two forms of apnoea are not so distinct as previously thought [6]. Both CSA and OSA exert several acute pernicious effects as intermittent hypoxia, arousals from sleep and swings in the negative intrathoracic pressure, which will lead to chronic physiologic consequences as nonrestorative sleep and chronic daytime sleepiness, followed by autonomic dysregulation, endothelial dysfunction and cardiac remodelling. CSA and OSA may further predispose to cardiovascular diseases as hypertension, coronary heart disease, stroke and congestive heart failure [6].
Case Report
A 79-year woman with multiple cardiac and metabolic comorbidities was admitted in our Section of Pulmonary Rehabilitation due to respiratory disturbances. One month prior to hospital presentation she started to experience daily episodes of sudden breath arrest after short episodes of hyperventilation. Hyperventilation was triggered by physical activity, especially in the bending forward position, for example when sweeping. She was diagnosed in the past with high blood pressure, coronary heart disease, major left bundle branch block, congestive heart failure NYHA class II, hypercholesterolaemia and hypothyroidism. She was effectively treated for hypertension, coronary heart disease, hypercholesterolaemia and hypothyroidism (levothyroxine 25 μg/ day), being clear-minded and very active in her rural household. Such a crisis of breath arrest occurred in the hospital at physical examination, when she was invited to perform more profound and frequent breathings. She suddenly started to gasp, became cyanotic and had no air flow despite her excessive breathing effort. It took about 2 minutes to resume ventilation and some other 20 min up to full recovery. She was cyanotic and had a very low SpO2 up to 80%. The neurological examination was normal, and the neurologist recommended overnight respiratory polygraphy and cerebral magnetic resonance imaging (MRI). In order to prevent the respiratory arrest crisis during hospitalisation she was advised to avoid intense physical activity and bending forward position, so she had no similar events during her hospital stay.
Physical Examination
Physical examination performed as a second attempt revealed an obese grade I 79-year woman, with a body mass index of 31.20 (1.60 m, 80 kg), a waist to hip ratio of 0.86 and a cervical circumference of 37 cm. She had normal blood pressure (130/80 mmHg) and heart rate (66/min) and no abnormalities at respiratory and cardiac auscultation. No oedema, no cyanosis and a normal SpO2 (98%).
Investigations
Blood tests revealed only a small increase of cholesterol (260 mg/dL) and urea level (50 mg/dL), and a small decrease of total calcium level (8.73 mg/dL). Resting ECG showed left axis deviation at -22°, sinus rhythm and left bundle branch block. Chest X-ray showed features of basal bilateral pulmonary fibrosis, with increased lung markings in the lower lobes. Spirometry was unexpectedly good, with forced vital capacity (FVC) of 3.09 L (143.9%), forced expiratory volume in 1 sec (FEV1) of 2.43 L (139.3%) and FEV1/ FVC ratio of 78.7%. Overnight respiratory polygraphy determined an apnoea-hypopnoea index of 23.3/hour, with desaturation index of 19.3/hour and the medium overnight SpO2 of 93%. Therefore, the patient was diagnosed with moderate obstructive sleep apnoea.
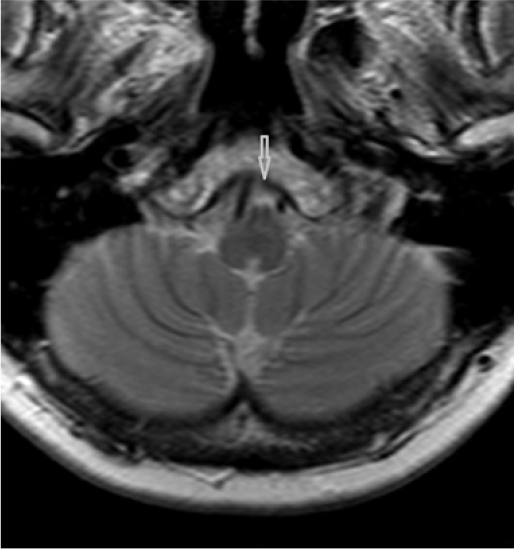
Native cerebral magnetic resonance imaging examination has revealed four features: normal MR signal of the brainstem; dominant and sinuous right vertebral artery (VA) compressing junction between medulla oblongata and spinal cord; medulla oblongata clamping in between the two vertebral arteries; and loss of foramen magnum cerebrospinal fluid (CSF) spaces due to low lying cerebellar tonsils tips, while cisterna magna is still visible. Figure 1 depicts the VA compressing right ventrolateral junction of medulla oblongata with spinal cord. Figure 2 reveals the medulla clamping in between the two vertebral arteries.
Discussion
According to our knowledge, this is the first reported case of HAS due to a dilated or sinuous VA. A sinuous VA compressing the medulla oblongata – spinal cord junction may compress the VRG which contains both inspiratory and expiratory neurons, as well as neurons which control larynx and pharynx muscles.
The case raises some questions on the pathophysiology of this rare hyperventilation-apnoea dysfunctional breathing pattern, taking into consideration the complex interactions between different pathologies. Advanced age, cardiac and metabolic disorders are responsible for atherosclerotic and tortuous systemic and cerebral vessels. Adequate vasodilator and vasoconstrictive reactivity of cerebral arterioles is a condition for proper capillary perfusion. While aging, the vasoregulatory capacity decreases, together with the basic mean flow velocity [7].
Medulla oblongata is supplied by several arteries, branches of vertebral arteries. Medullar compression by vertebral arteries is a rare condition. Discussing a similar case, Savitz reported nine patients with medullar compression by tortuous, angulated, and/or dominant vertebral arteries, but not necessarily elongated or dilated [8]. They counted only 19 reported patients with transient symptoms or permanent neurologic deficit, motor or vestibular or cerebellar features [8]. There is a poor correlation between radiographic features and symptoms, and surgery may provide only temporary symptom relief and cause other complications [8]. Theoretical, compression over brainstem and cranial nerve roots may result in medulla oblongata compression, facial spasm, trigeminal neuralgia, neurogenic hypertension, cerebellar dysfunction, hydrocephalus, central or obstructive apnoea [9].
Along with other comorbidities, our patient was diagnosed and treated for hypothyroidism. It seems to be an etiologic relationship between hypothyroidism and OSA in some patients. Hypothyroidism might cause OSA through different mechanisms: mucoprotein deposition in the upper airway, decreased neural output to the upper airway musculature, obesity, and abnormalities in ventilatory control. Case series have reported that 50 to 100 % of patients with this association show a reduction or even a complete resolution of sleep-disordered breathing with levothyroxine therapy [10].
In addition to a nonrestorative sleep and excessive daytime sleepiness, impaired cognitive function and reduced quality of life [6,11], OSA is related to serious cardiovascular consequences like hypertension, coronary artery disease, stroke and congestive heart failure [6]. Comparing to general population, the prevalence of OSA in patients with these conditions is much higher than in general population, reaching 30-50% [6]. Sleep apnoea is a common and important comorbidity in heart failure and affects survival by several mechanisms, such as: nocturnal hypoxia and oxidative stress; increasing daytime sympathetic activity and blood pressure and blunting vagal tone; and by increasing left transmural pressure and myocardial oxygen demand [12].
The prevalence of sleep apnoea is much higher in fluid-retention states like heart failure and end-stage renal disease comparing to general population. This finding led to the hypothesis that fluid retention is involved in the pathogenesis of both CSA and OSA. Due to gravity, fluid accumulates during daytime in the intravascular and interstitial spaces of the legs, and it is redistributed rostrally when lying down during night-time. Some of this fluid may accumulate in the neck, increasing tissue pressure, narrowing upper airways and predisposing to OSA, or in the lungs, generating hyperventilation and predisposing to CSA [5]. Severity of OSA is not associated with increasing BMI in heart failure patients, suggesting that other factors than obesity are involved. Patients with heart failure and sleep apnoea have a higher sodium intake, with consecutive fluid retention, and the apnoea-hypopnoea index is correlated with sodium intake [5]. Moreover, it seems possible that increasing in pulmonary capillary and interstitial pressure due to chronic heart failure can change afferent information on the lung status transmitted through the C unmyelinated fibres. It is uncertain how C fibres may modulate the respiratory control, but it is possible that they play a role in the tachypnoea seen in patients with CHF and other conditions associated with acute changes in pulmonary capillary pressure [3].
Therefore, treatment of cases associating OSA and heart failure will consist of various forms of positive airway pressure, such as continuous positive airway pressure (CPAP) ventilators [13] and therapies to prevent fluid retention: loop diuretics and aldosterone antagonists, sodium restriction, compression stockings, elevating the head of the bed, physical exercises and ultrafiltration [5]. Moderate and severe OSA are associated with an increased mortality; weight loss is a useful measure to improve outcomes in OSA patients [14]. The prognosis of hyperventilation-apnoea syndrome is generally good [15], but the patient should continue her long-term treatment to avoid blood pressure rises and consecutive haemodynamic compromise, adding antiplatelets and anticoagulants [8].
Microvascular decompressive surgery has become the most appropriate technique to reduce symptoms in simple neurovascular compression syndromes [8]. For example, a tortuous vertebrobasilar artery might be pulled away and fixed with unabsorbable nylon or silk on the nearby dura-mater through a microsurgical repositioning technique [9,16]. But this technique has no application in this case due to right vertebral arterial status which is simply sinuous and not dolichoectatic. Functional neuroimaging, including 99mTc single photon emission computerized tomography scanning, may be helpful in detecting brainstem hypoperfusion, otherwise a delay in correct diagnosis and treatment might allow irreversible brainstem ischaemia to occur [16] and to compromise the neurological and overall prognosis of the patient.
According to our knowledge, this is he first reported case with hyperventilation-apnoea syndrome associated with a sinuous vertebral artery compressing the ventrolateral part of medulla spinal cord junction. It is difficult to demonstrate the correlation between MRI findings and respiratory symptoms. It is also difficult to know if or when to recommend corrective vascular neurosurgery in such a complex and multifaced case. Conservative treatment might be the best way to manage this case. The patient was well and alive at her 80th anniversary, without non-invasive ventilation or microvascular decompressive surgery that she has refused.
Disclosure
The authors declare that they have no conflict of interest.
References
- Homma I, Masaoka Y (2008) Breathing rhythms and emotions. Ex Physiol 93(9): 1011-1021.
- Paterson DJ (2014) Defining the neurocircuitry of exercise hyperpnoea. J Physiol 592(3): 433-444.
- Schwartzstein RM, Parker MJ (2006) Respiratory physiology: a clinical approach. Lippincott Williams & Wilkins, Philadelphia, Baltimore, New York, London, Buenos Aires, Hong Kong, Sydney, Tokyo, pp. 9-29 & 126-144.
- Malhotra A, Owens RL (2010) What is central sleep apnea? Respir Care 55(9): 1168-1178.
- White LH, Bradley DT (2013) Role of nocturnal rostral fluid shift in the pathogenesis of obstructive and central sleep apnoea. J Physiol 591(5): 1179-1193.
- Leung RS, Comondore VR, Ryan CM, Daniel Stevens (2012) Mechanisms of sleep-disordered breathing: causes and consequences. Pflugers Arch 463(1): 213-230.
- Peisker T, Bartos A, Skoda O, Ibrahim Ibrahim, Pavel Kalvach (2010) Impact of aging on cerebral vasoregulation and parenchymal integrity. J Neurol Sci 299(1-2): 112-115.
- Savitz SI, Ronthal M, Caplan LR (2006) Vertebral artery compression of the medulla. Arch Neurol 63: 234-241.
- Pereira-Filho A, Faria M, Bleil C, Luiz Kraemer (2008) Brainstem compression syndrome caused by vertebrobasilar dolichoectasia: microvascular repositioning technique. Arq Neuropsiquiatr 66(2B): 408-411.
- Kapur VK, Koepsell TD, deMaine J, Richard Hert, Sandblom RA, et al. (1998) Association of hypothyroidism and obstructive sleep apnoea. Am J Respir Crit Care Med 158: 1379-1383.
- Jilek C, Gebauer J, Muders F (2012) Polysomnography underestimates altered cardiac autonomic control in patients with obstructive sleep apnea. Herzschr Elektrophys 23: 45-51.
- Floras JS (2009) Should sleep apnoea be a specific target of therapy in chronic heart failure? Heart 95(13): 1041-1046.
- Ciobanu LD (2018) Non-invasive ventilation in chronic heart failure, an important comorbidity of COPD. ECPRM 7.6: 416-423.
- Zammit C, Liddicoat H, Moonsie I, Makker H (2010) Obesity and respiratory diseases. Int J Gen Med 3: 335-343.
- Munemoto T, Masuda A, Nagai N, et al. (2013) Prolonged post-hyperventilation apnea in two young adults with hyperventilation syndrome. Biopsychosoc Med 7(1): 9.
- Hung PE, Shen CC (2011) Neurovascular decompression for lateral medullary syndrome caused by vertebral artery dolichoectasia. J Med Sci 31(6): 283-288.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.