Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Investigating the Relationship Between Clinical Characteristics of 2019 Novel Coronavirus Pneumonia Cases (COVID-19) Before Intubation and Treatment Outcome After 14 Days in Imam Khomeini Hospital Complex, Tehran, Iran: Descriptive-Analytic Study
*Corresponding author: Hesam Aldin, Hossein E, Bachelor of Nursing, Islamic Azad University Tehran Medical Sciences, Young Researcher and Elite Clube, Tehran, Iran.
Received: October 16, 2020; Published: October 30, 2020
DOI: 10.34297/AJBSR.2020.10.001556
Abstract
In December 2019, a new pathogen, HCoV, or New Corona Virus 2019 (2019-nCoV), was recognized in Wuhan, China, causing a pandemic. COVID-19 has a wide range of clinical severity. Approximately 3.2% of patients with some periods of the disease require intubation and invasive ventilation.
Methods: This was a descriptive-analytical study and conducted in the spring of 1399 in Imam Khomeini Hospital. Patients with COVID-19 who required endotracheal intubation were identified and their clinical symptoms and laboratory parameters were recorded. SPSS23 software was used for statistical analysis.
Results: 120 COVID-19 patients with different conditions were evaluated. The mean age was 55±14. All patients had some degree of acidosis before intubation. Lymphopenia was a common finding among patients before intubation, but thrombocytopenia and thrombocytosis were very rare. The highest mortality was observed in blood group A, but blood group O had the highest discharge from ICU. SOFA and APACHE scores were significantly associated with treatment outcome in all three groups of patients. Discussion: Although all laboratory parameters and patients symptoms can affect the treatment outcome, it was found that WBC and absolute lymphocyte count, BUN, SOFA and APACHE scores, inflammatory index ratio CRP/LDH% CRP/ESR% and ESR/LDH%, arterial blood gas indices, pulse rate, and patient temperature before intubation are among the parameters that can affect the patient’s 14-day prognosis.
Conclusion: Except for the mentioned items, CRP/LDH% ratio seems to be a good indicator for checking the prognosis of discharge or death of patients within 14 days, However, CRP/ESR% and ESR/LDH% are appropriate criteria for determining the prognosis for discharge or stay in the ICU for more than 14 days.
Keywords: COVID-19, Intubation, ICU, CRP, LDH, Invasive ventilation.
Introduction
Human coronavirus is one of the main pathogens of respiratory infections. These two highly pathogenic viruses, SARS-CoV and MERS-CoV, cause severe respiratory syndrome in humans and four other human coronaviruses (HCoV-OC43, HCoV-229E, HCoVNL63, HCoV-HKU1) cause mild upper respiratory tract disease. The major SARS-CoV outbreak, which affected 8,422 patients between 2002 and 2003, spread to 29 countries worldwide (18,19). Human coronaviruses (HCoVs) have long been considered trivial pathogens and cause “colds” in healthy people. In December 2019, a new HCoV pathogen, or 2019 novel-coronavirus (2019-nCoV), was identified in Wuhan, China, causing serious illness and death. The extent and ultimate impact of this outbreak are currently unclear as the situation is rapidly evolving [1]. The most common and severe complication in patients with COVID-19 is acute hypoxemia or acute respiratory syndrome (ARDS), which requires oxygen therapy and ventilation [3]. They had aggressive intubation and ventilation [3,4]. Approximately 3.2% of patients with COVID-19 require intubation and invasive ventilation during some periods of the disease [2] 19.
Confirmation or suspicion could be done. Some of these surgeries were performed under general anesthesia with endotracheal intubation. The intubation and ventilation of patients with COVID-19 who are highly sensitive or require urgent surgical intervention pose some unique challenges for health care providers [3-4]. COVID-19 has a wide range of clinical severity, ranging from asymptomatic to critically ill and ultimately death [5,6,7]. Which may be necessary in patients with cardiopulmonary arrest or jeopardized airway. In patients with acute COVID-19-induced acute respiratory hypoxemia, it can be challenging to decide whether to continue intubation and invasive ventilation [2,8]. For patients with improvement in respiratory distress, tachypnea (respiration rate greater than 30 beats per minute), and poor oxygenation (Pao2 versus Fio2 less than 150mm Hg) after 2 hours of high-flow oxygen therapy or non-invasive ventilation takes [9]. Most people infected with the COVID-19 virus have a mild illness and are recovering, according to the World Health Organization.
Approximately 80 laboratory-confirmed patients with mild adjustment, including non-pneumonia and those with pneumonia, will have 13.8 severe illnesses (shortness of breath, respiratory rate /30 per minute, blood oxygen saturation 93, PaO2 to FiO2 ratio less than 300, and/or lung infiltration>50 from the lung background in 24-48 hours) and 6.1 are highly critical (respiratory failure, septic shock, and/or dysfunction / organ failure) [27]. In a descriptive study in Wuhan, China, which examined the symptoms of 99 patients with COVID-19, many patients with functional organ damage, including (17%) with ARDS (8%) with acute respiratory injury, 3% had acute kidney damage, 4% had septic shock and 1% had ventilator-induced pneumonia [10]. In terms of laboratory tests, the absolute number of lymphocytes is reduced in most patients. This result suggests that 2019-nCoV may act primarily on lymphocytes, especially T lymphocytes, such as SARS-CoV. Virus particles spread through the respiratory mucosa and infect other cells, cytokine storm Induce in the body, trigger a series of immune responses, and alter peripheral white blood cells and immune cells such as lymphocytes.
Some patients with ARDS and septic shock progress rapidly, eventually leading to failure. Multiple limbs were associated. Therefore, early detection and timely treatment of important cases is of particular importance. Absolute low lymphocyte counts can be used as a reference in the diagnosis of new coronavirus infections in the clinic [10]. Some studies suggest that A significant reduction in the total number of lymphocytes indicates that the coronavirus consumes (depletes) many immune cells and inhibits the function of the body’s cellular immune system. T lymphocyte damage may be an important factor in exacerbating patients [11-15]. ARDS was present in 20 of 138 patients and in 61 of 36 patients admitted to the Intensive Care Unit (ICU) at Zhongnan Hospital in Wuhan [4]. Dysfunction, injury, or organ failure, except for the lungs, is common. Heart damage occurred in 23, liver damage in 29 and acute kidney damage in 29 critically ill patients [3]. Neurological disorders occur in more than one-third of patients with advanced COVID-19.7 [8]. Decreased susceptibility of women to viral infections can be attributed to protection against the X chromosome and sex hormones, which play an important role in innate immunity and adaptation [16-19].
Like MERS-CoV viruses, almost half of the patients infected with 2019-nCoV had chronic underlying disease: mainly cardiovascular disease and diabetes [14]. Mortality SARS- CoV more than 10 and MERS-CoV with more than 35 have been reported [20,21]. Regarding the mortality rate of patients with 2019-nCoV, 11% has been reported in two studies [6,7]. Additional deaths may occur in people who are still hospitalized. Another study found that ICU patient mortality was improved by 20.5%, as well as 21.1% of ICU non-hospitalized patients [31]. The laboratory results of a meta-analysis showed that lymphocytopenia (64.5), increased CRP (44.3), increased LDH (28.3) and leukocytopenia (29.4) were more common, and in general, all of them were compatible with respiratory virus infection [22]. Studies have also shown that the level of inflammatory cytokines may be associated with disease severity, which is expected to be an indicator of disease severity [6,23,24]. The SOFA score is a good diagnostic marker for sepsis and septic shock and indicates the status and degree of dysfunction [25,26].
A retrospective cohort study of several risk factors for adult death in Wuhan with COVID-19 In particular, older age, d-dimer levels above 1μg/ml, and higher SOFA score at baseline were associated with a higher chance of death in hospital [24]. Thrombocytopenia in patients with COVID-19 has been observed and may be multifactorial [27]. In SARS, it has been suggested that a combination of viral infection and mechanical ventilation may lead to platelet activation, accumulation damage, and thrombosis in the lungs, leading to high platelet intake. As the lung may be a site of platelet diffusion from fully mature megakaryocytes, intermittent morphological depletion in the pulmonary capillary substrate may lead to platelet failure [28]. Coronaviruses may also directly infect bone marrow elements because of abnormal hematopoiesis [29], triggering an autoimmune response against blood cells. It has also been suggested that moderate-to-reduced DIC may produce lower platelet counts in SARS [28]. A study to evaluate lactate dehydrogenase as a risk factor for patients with coronavirus found that LDH was positively correlated with both APACHE II and SOFA scores, as well as PSI and CT. In addition, as a protective agent the lymphocyte count was less than 1.045x109/liter.
Good accuracy in identifying severe patients, maximum specificity (91/30) and sensitivity (24/95) showed. In addition, LDH was positively correlated with CRP, AST, BNP and cTnI, while it was negatively correlated with lymphocyte cells and its subsets including CD3+, CD4+ and CD8+ T cells (P<0.01). The study also found that LDH is a powerful predictor of early detection of lung damage and severe cases of COVID-19. Importantly, the number of lymphocytes, especially CD3+, CD4+ and CD8+ T cells in the peripheral blood of COVID-19 patients, which was related to serum LDH, was dynamically correlated with disease severity [30]. With higher APACHE II and SOFA scores, high PCT levels, excessive fluid volume, and delayed corticosteroid use may increase the risk of death [31]. The results of a study in China showed that blood type A was more dangerous. Achieving COVID-19 was associated with a lower risk of infection compared with non-A blood groups compared with non-A blood groups. This is the first observation of the association between ABO blood type and COVID-19, although more research is needed to confirm this [32]. Preliminary studies on the effect of BCG vaccination suggest that BCG vaccination is the number of reported COVID cases. Reduces-19 in a country.
The combination of reduced morbidity and mortality makes BCG vaccination a potential new tool in the fight against COVID-19 [33,34]. Given that there is currently no definitive cure for coronavirus-19 pneumonia, and supportive therapies such as oxygen therapy, mechanical ventilation, and nutritional support are the basis of these patients’ treatment process, and given that Many of the treatments offered are clinical trials and research. Knowing what the patient is at and what the patient’s prognosis may be of great help to physicians and researchers in choosing different treatments and clinical strategies. Therefore, according to the research records in the field of clinical signs and laboratory parameters of patients with COVID-19, as well as mechanical ventilation and endotracheal intubation, it is necessary to study the relationship between clinical signs and laboratory parameters of patients before intubation and Outcome/outcome of their treatment.
Methods and Materials
This is a descriptive-analytical study that was conducted in the spring of 1399 (April to June 2020) in Imam Khomeini Hospital. This article has an ethics code number IR.TUMS.VCR.REC.1399.389. Patients with Covid-19 who required endotracheal intubation were identified and their clinical signs and laboratory parameters were recorded. These include: vital signs (SPO2,HR,BP,T), inflammatory factors (CRP,LDH,PCT,ESR), Complete Cell Count (CBC), Arterial Blood Gas Factors (ABG or VBG), Liver Function Test (ALT, AST), Electrolytes (Na,K,Ca) and Blood Urea Nitrogen and Creatinine (BUN, Cr) were recorded. The patient’s clinical condition including underlying disease (such as diabetes, hypertension, etc.) and Either co-morbidity (such as acute renal failure, or ventilator-induced pneumonia) was extracted from the patient’s record. APACHE 2 and SOFA scores were also calculated. After intubation, patients were followed for 14 days to determine the outcome of their treatment. Patients were divided into three groups based on the outcome of treatment: group 1 patients who recovered/discharged within 14 days, group 2 patients who remained in the ICU for more than 14 days, and group 3 patients who died within 14 days. After collecting data, data were analyzed by SPSS-23 statistical software. Descriptive statistics including mean and standard deviation were used. Also, inferential statistics including one-way variance (ANOVA) were used. To analyze the qualitative variables, Phi and Cramer correlation coefficient analysis was used.
Results
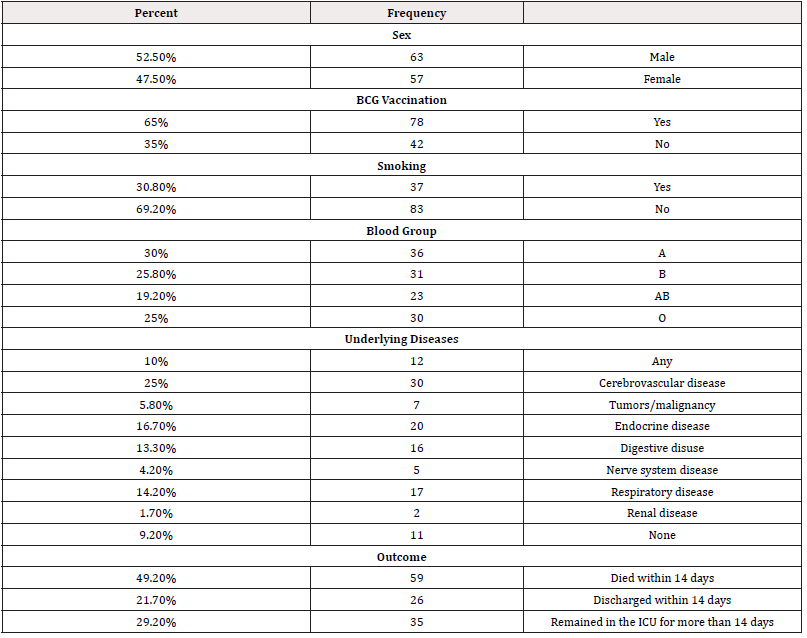
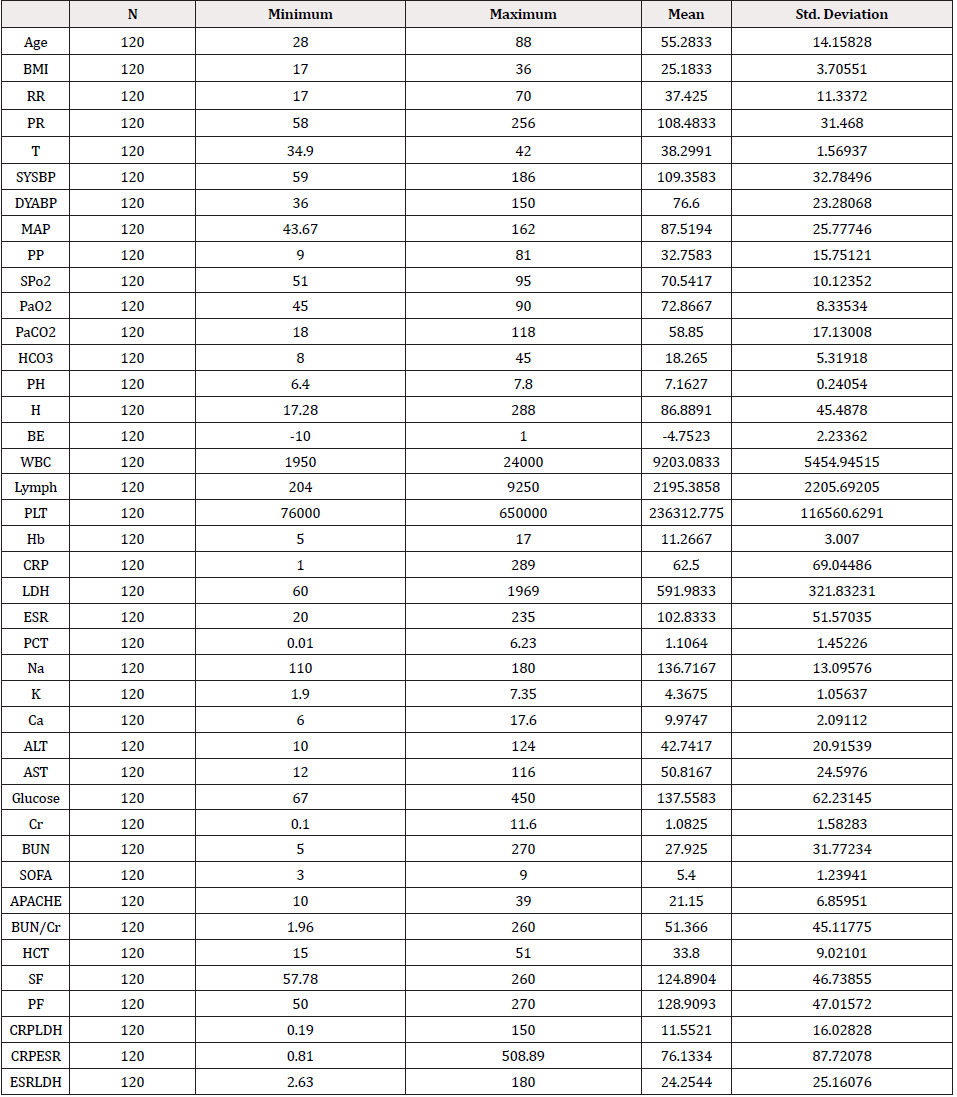
In this study, 120 patients were evaluated. The demographic information of the patients is given in Table 1. Underlying diseases were extracted from the records of 25% of patients with cardiovascular and cerebral diseases (such as hypertension), 16.7% with diseases of the endocrine system (such as diabetes) and 14.2% with respiratory diseases (such as asthma or COPD). In general, patients were divided into 14-day survival: survival and non-survival. Therefore, according to the survival (50.8%) of 61 patients and death (49.2%) of 59 patients, the mortality rate was 49.2%. 22.5% of patients showed several associated comorbidity conditions within 14 days (such as acute renal failure with pneumonia). Acute respiratory failure and respiratory distress syndrome were also observed in 19.2% of patients. 10% of patients experienced acute lung or kidney injury.
Table 2 To examine the correlation of qualitative variables, Phi and Cramer correlation analysis were used. Based on Phi and Kramer correlation analysis, a significant correlation was found between comorbid disease and patient outcome (P-Value=0.00), blood group and outcome treatment (P-Value=0.01). However, no statistically significant correlation was found between the underlying disease and therapeutic outcome (P-Value=0.19) [Table 3-5]. 31 patients (25.8%) had no accompanying condition, 27 patients (22.5%) had more than 1 accompanying condition, 23 patients (19.16%) had respiratory distress syndrome and 12 patients (10%) had acute renal failure or suffered from acute respiratory failure. The frequency of patients’ blood groups was A (30%), B (25.8%), O (25%) and AB (19.16%), respectively. The highest mortality was observed in blood group A, blood group O had the highest discharge from ICU and most patients who were in ICU for more than 14 days had blood groups AB and O. Cardiovascular diseases, endocrine diseases and respiratory diseases were the most common underlying diseases, respectively.
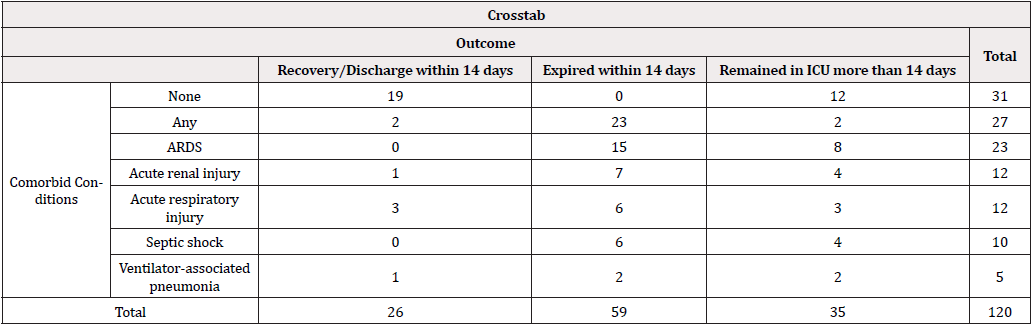
Table 3: Comorbid Conditions and Outcome The correlation coefficient is Phi=72% and the Cramer correlation coefficient is 52%.
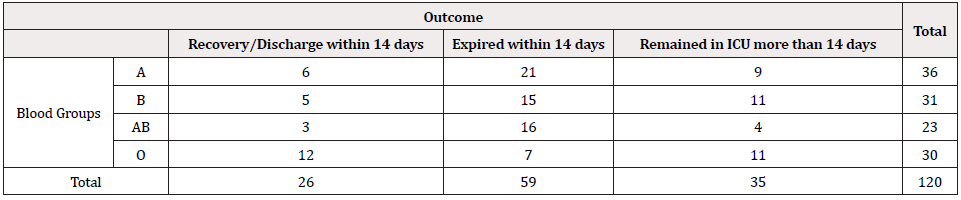
Table 4: Blood groups and Outcome
The correlation coefficient is Phi=35% and the Cramer correlation coefficient is 25%.
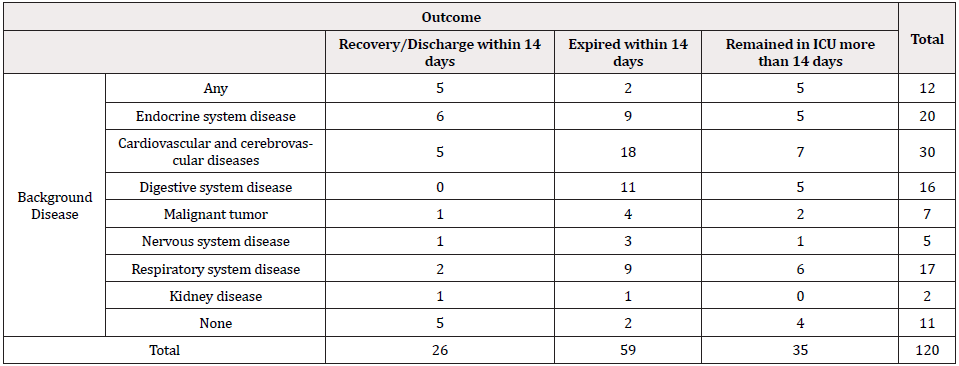
Table 5: Background disease and Outcome
The correlation coefficient is Phi=41% and the Cramer correlation coefficient is 29%.
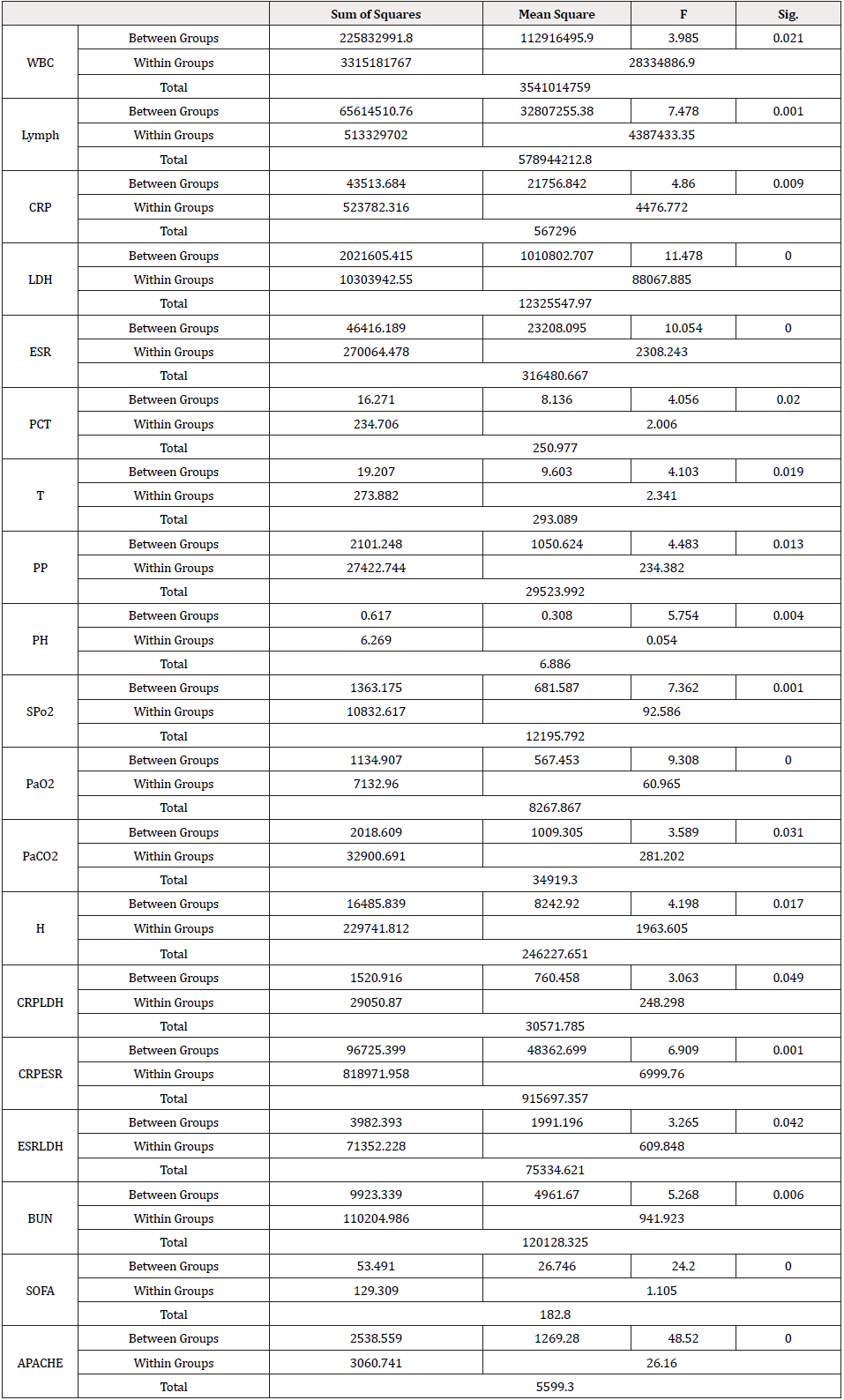
Table 6: One-way ANOVA
Tukey post hoc test was used to follow the mean difference of quantitative parameters.
In this study, to compare the mean of the measured parameters before intubation and treatment outcome, one-way variable analysis of variance was used and the results were reported as follows [Table 6]. The results of this test showed that the amount of hydrogen ion in group 1 patients (65.28±28.07) was significantly (95.37±54.96) less than group 3 patients (P-Value=0.013). Regarding the ratios of inflammatory markers, the ratio CRP/LDH% was higher in group 1 patients (16.46±12.75) than group 3 patients (8.13±7.21) (P-Value=0.049). CRP/ESR% ratio in group 1 patients was significantly higher (P-Value=0.003) than group 2 patients (73.60±21.66) and 3 patients (65.25±19.69). Also, the ESR/LDH% ratio in group 1 patients was significantly lower (P-Value=0.047) than group 3 patients (-15.33±6.39). No significant difference was found in the mean serum creatinine of patients in group 3 (P-Value=0.08). The mean of blood urea nitrogen was significantly lower in group 2 patients (21.28±11.88) than other patients. BUN/ Cr ratio was not significantly different in treatment outcome in different groups.
In comparison with the mean of vital signs, body temperature was significantly (P-Value=0.02) in group 1 compared to groups 2 (-1.08±0.39) and 3 (-0.86±0.36). The oxygen saturation (SPO2%) in group 1 patients was significantly (P-Value=0.01) higher than group 2 patients (9.03 ± 2.42) and (P-Value=0.04) in group 3 patients (7.38±2.26). The mean blood pH of patients in group 1 (7.19±0.19) was significantly (P-Value=0.004) higher than patients in group 2 (7.12±0.25) and group 3 (7.12±0.23). The mean absolute amount of hydrogen ion was similarly (P-Value=0.01) higher in patients who died within 14 days (95.37±54.96) than the other two groups. The mean values of relative pressure of carbon dioxide in groups 2 and 3 were significantly higher than those in group 1. The mean serum bicarbonate was higher in group 1 patients than other groups. Mean white blood cell count (P-Value=0.02) in group 2 patients was higher than group 3 patients (2984.74±1135.70).
In addition, total lymphocyte count in group 2 patients was higher than both groups, (P-Value=0.02) and (1875.95±542.31) compared to group 1 and to group 3 (P-Value=0.04) (146.86±446.89). In this regard, the mean absolute lymphocyte count in group 1 patients (1444.14 11 1189.89±1489.14) was significantly lower (P-Value=0.00) than group 3 (1859.23±1968.49) and group 2 (3320.10±2728.84). Mean pulse pressure was significantly different in 3 groups of patients (P-Value=0.01). This value was higher in patients in group 1 (40.50±19.21) than in groups 3 (31.45±14.67) and 2 (29.20±12.96). This difference shows that patients discharged from ICU maintained a more normal range than other groups. The mean SOFA score in group 3 patients (P-Value=0.00) was higher than group 1 patients (1.58±0.24) and 2 patients (1.05±0.22). Consistent with this mean, APCHE score in this group of patients was significantly higher (P-Value=0.00) than the other two groups of patients (9.98±1.20) compared to group 1 and (8.51±1.09) compared to group 2.
Discussion
Numerous cases before intubation can affect the treatment outcome of patients. The underlying disease or comorbid conditions of patients during hospitalization in the intensive care unit can affect the therapeutic outcome of patients. Patients with several comorbid conditions, such as aspiration pneumonia and septic shock, had the highest mortality in 14 days. Patients with Respiratory Distress Syndrome were also ranked second in mortality or hospitalization for more than 14 days. One study state that ARDS is one of the most common comorbid conditions in patients [22]. The results of a meta-analysis show that hypertension, diabetes, cardiovascular disease, and respiratory diseases were the most common conditions in patients [55]. Also, the results of an analysis show that in addition to hypertension and diabetes being the most common condition of patients, 8.2% of patients had more than one condition [56]. Although the highest rate of death occurred among patients with blood type A and the highest rate of ICU discharge was seen in patients with blood type O, it cannot be said that blood type O alone has a protective effect against disease caused by the virus and more research is needed.
One of the most important laboratory parameters studied was WBC, which on average showed mild leukocytosis in patients, as previously found by studies [35,36,38,40]. However, some studies have found leukopenia to be a more common finding in patients. They know [37]. Leukocytosis was evident in patients who remained in the ICU for more than 14 days and no significant differences were found between patients in groups 1 and 3. Lymphopenia was a common finding among patients before intubation that is consistent with the results of previous studies [37-39,41]. Lymphopenia has also been shown to be associated with poor prognosis and can be a measure of disease severity [39]. Lymphopenia, or lymphocytopenia, is a decrease in the number of circulating lymphocytes, often in which the lymphocyte count is less than 2,500 Lymphocytes Per Microliter (LCM). Patients discharged from the ICU experienced more severe lymphopenia than the other groups. The cause of lymphopenia in this group of patients may be due to the use of high doses of corticosteroids, underlying diseases, or malnutrition.
The results of a meta-analysis showed that lymphopenia is directly related to the severity of the disease and less than 1,500 lymphocytes can predict clinical outcome [59]. Patients who remained in the ICU for more than 14 days had the highest mean lymphocyte count [40]. Serial evaluation of lymphocyte count seems to be a predictor of patient outcome [41]. Chronic diseases and aging cause chronic endothelial dysfunction. Endothelial dysfunction causes separation of intercellular junctions, endothelial cell death, and rupture of the blood-tissue barrier with increased adhesion and leukocyte leakage, which may play a role in explaining the lymphopenia observed in severe COVID-19 patients [60]. It can be said that high lymphocyte counts (more than 3320) predict longterm stay of patients in the ICU. No significant platelet count was found, and on average patients’ platelets were within the normal range (thrombocytopenia and thrombocytosis were very rare). Studies have shown that thrombocytopenia is associated with disease severity [42-44] and is a common finding in these patients.
Unlike studies [35] that reported PaO2/FiO2 and SPO2/FiO2 ratios in the evaluation and prognosis of acute lung injury and respiratory distress syndrome, in the present study, no significant results (P-Value=0.7) were found between these two ratios with the prognosis of coronavirus pneumonia 2019 [45,46]. Various studies have addressed the importance of inflammatory markers in the diagnosis and severity of coronary heart disease. Procalcitonin is one of the factors that affect the outcome of treatment [47]. However, the diagnostic value of this factor seems to be lower than CRP and interleukin-6 (alone) [48]. One of the factors influencing the therapeutic outcome in this study was lactate dehydrogenase index, which various studies confirm the importance of this inflammatory index in the evaluation and response to treatment of coronavirus-induced pneumonia [49,50], so that increasing this index indicates high disease severity and its reduction indicates an appropriate response to treatment and prognosis of patients [41].
Reactive protein C is one of the inflammatory markers that in the early stages of the disease is widely associated with the severity and spread of the disease [45,46]. However, in this study, no significant association was found with high CRP levels prior to intubation and treatment outcome. Of course, values above 50 of these factors can predict the severity of the disease. Arterial/venous blood gas parameters (PH, PaO2, PaCO2, HCO3, H+) influenced the therapeutic outcome of patients. The mean pH of all patients was less than 7.35. This indicates that all patients had some degree of acidosis before intubation. However, the discharged patients PH ranged from 7 to 7.38 which was near to 7.35. Patients in group 2 ranged from 7.37 to 6.97 and patients in group 3 ranged from 7.35 to 6.99, indicating a higher severity of acidosis in these two groups of patients. The amount of hydrogen ions, which is directly related to blood pH, was similarly higher in group 3 patients than in groups 2 and 1 (respectively) [51-58].
High levels of relative pressure of carbon dioxide in group 2 and 3 patients may indicate acute respiratory failure or respiratory distress syndrome in these patients before intubation. Group 1 patients had normal serum bicarbonate levels before intubation, while the other two groups experienced a decreased mean. This decrease may indicate metabolic disorders such as metabolic acidosis or diabetic ketoacidosis [59-60]. The results of some studies show that patients with coronavirus show some degree of respiratory and metabolic acidosis [4,61]. Since many patients also have diabetes, monitoring bicarbonate levels to prevent diabetic ketoacidosis or ketosis can be helpful. COVID-19 infection appears to cause ketosis or ketoacidosis and induce diabetic ketoacidosis in diabetics, and ketosis can increase mortality and length of hospital stay [62]. Although the mean serum creatinine of patients in all 3 groups was not significantly different, the amount of blood urea nitrogen in patients in group 1 was higher than in groups 2 and 3. This increase may be related to acute renal impairment or sampling/laboratory error or drug side effects.
However, Glomerular Filtration Rate (GFR) was not calculated in patients, so increasing blood urea nitrogen alone in group 1 patients alone could not indicate acute renal impairment. However, mean blood urea nitrogen was lower in patients who were in the ICU for more than two weeks than in other patients. BUN/Cr ratio, considering that this ratio is a good indicator for differentiating the causes of pre-renal or post-renal failure, and the mean increase (51.36±45.11) in all patients, can be said to be one of the reasons for increasing this value which can be caused by causes such as gastrointestinal bleeding [53], decreased renal perfusion, shock, hypovolemia, hypotension and dehydration. Serum Nitrogen Urea (BUN), Creatinine (Cr), Urinary Inhibitor C (CysC) and Retinol-Binding Protein (RBP) can be used for early detection of kidney damage [54]. SOFA and APACHE scores were significantly associated with treatment outcome in all three groups of patients. These two criteria were higher in patients who died within 14 days than in the other two groups. Also, patients who were hospitalized in the intensive care unit for more than 14 days had higher scores than patients who were discharged from the intensive care unit for 14 days.
In this study, SOFA and APACHE scores were measured only once before intubation. Since the frequency of SOFA score is more important, it is recommended to calculate the SOFA score serially for patient follow-up.
Pulse pressure is the difference between systolic and diastolic blood pressure [57] and is one of the parameters that had a significant impact on the outcome of treatment. Normal values are 40 mm Hg, in the presence of hypoperfusion, flattening of the pulse pressure is due to Systemic Vascular Resistance (SVR). Low blood pressure can also be a sign of heart problems despite a narrow pulse pressure. Patients discharged from the ICU maintained a normal mean, while patients who died had a lower mean and patients who remained in the ICU had a lower mean. The most common cause of low pulse pressure is a drop in left ventricular shock volume. In trauma, low or narrow pulse pressure indicates significant blood loss [58] (insufficient preload leads to decreased cardiac output).
Due to the significant decrease in pulse pressure in both groups of patients, it seems that these patients have some degree of heart failure, shock, aortic stenosis or in some cases cardiac tamponade. In this study, by examining different criteria, we obtained three inflammatory ratios that can be helpful in determining the prognosis of patients who have an indication for intubation. CRP/ESR%, ESR/ LDH% and CRP/LDH% ratios had a significant effect (respectively) in determining the prognosis of patients. Due to the small number of quantitative values, the percentage of these parameters was used. The CRP/LDH% ratio was lower in patients who died than in other groups, and discharged patients had the highest mean. CRP/ ESR% ratio was higher in discharged patients than other groups and had the lowest mean in group 2. However, ESR/LDH% had the highest mean in group 2 and the lowest mean in group 1.
As in a study based on blood group association and coronavirus infection and therapeutic outcomes, a significant association was found in this study, indicating higher mortality in people with blood type A than in other blood groups. Also, the lowest death rate was observed among people with blood type O. Although some studies suggest [61] BCG vaccination can have a positive effect on the immune system against Covid-19, but in this study, no relationship was found between vaccination and therapeutic outcome and even the severity of the disease [62]. Limitations of this study include the extent of patients in the intensive care units of Imam Khomeini Hospital. Also, due to the critical situation, there may be errors in data collection, laboratory reports and even blood sampling.
Conclusion
According to the results, white blood cell count and absolute lymphocyte count, blood urea nitrogen, SOFA and APACHE scores, CRP/LDH%, CRP/ESR% and ESR/LDH% Arterial blood gas indices, pulse rate and patient temperature before intubation are among the parameters that can affect the patient’s 14-day prognosis. The CRP/LDH% ratio seems to be a good indicator for predicting the prognosis of discharge or death of patients within 14 days, but CRP/ESR% and ESR/LDH% are suitable criteria for determining the prognosis of discharge or stay of more than 14 days in Be ICU. Inflammatory ratios were obtained experimentally from this study, and the reliability and cut-off determination of these values require further research. Mortality seems to be higher among people with blood type A than other blood groups. No significant relationship has been found between BCG vaccination and therapeutic outcome of patients.
The patient’s comorbid conditions had a significant effect on treatment outcome, although the underlying disease did not differ significantly in treatment outcome. However, further studies are needed to investigate the effect of underlying disease on treatment outcome or mortality in patients. We would like to thank all the esteemed staff of Imam Khomeini Hospital in Tehran. Special thanks to the doctors, nurses and all the clinical staff of the intensive care unit who helped us in this project in times of crisis. The researchers have been greatly thanked and appreciated.
Funding
The study was not financially supported.
Acknowledgments
The authors are thankful to all the respondents for their voluntary participation and staff in research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Paules CI, Marston HD, Fauci AS (2020) Coronavirus infections-more than just the common cold. Jama 323(8): 707-708.
- Meng L, Qiu H, Wan L, Ai Y, Xue Z, et al. (2020) Intubation, and ventilation amid the COVID-19 outbreak: Wuhan’s experience. Anesthesiology 132(6): 1317-1332.
- Yang X, Yu Y, Xu J, Shu H, Liu H, et al. (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8(5): 475-481.
- Wang D, Hu B, Hu C, Zhu F, Liu X, et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Jama 323(11): 1061-1069.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl j me 382(18): 1708-1720.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223): 497-506.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223): 507-513.
- Mao L, Wang M, Chen S, He Q, Chang J, et al. (2020) Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China. Jama Neurol 77(6): 1-9.
- Zuo M, Huang Y, Ma W, Xue Z, Zhang J, et al. (2020) Expert Recommendations for Tracheal Intubation in Critically III Patients with Noval Coronavirus Disease 2019. Chin Med Sci 35(2): 105-109.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223): 507-513.
- Liu WJ, Zhao M, Liu K, Xu K, Wong G, et al. (2017) T-cell immunity of SARS-CoV: Implications for vaccine development against MERS-CoV. Antiviral Res 137: 82-92.
- Fan E, Brodie D, Slutsky AS (2018) Acute respiratory distress syndrome: advances in diagnosis and treatment. Jama 319(7): 698-710.
- Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, et al. (2019) Acute respiratory distress syndrome. Nature reviews Disease primers 5(1): 1-22.
- Badawi A, Ryoo SG (2016) Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis 49: 129-33.
- Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, et al. (2017) Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol 198(10): 4046-4053.
- Jaillon S, Berthenet K, Garlanda C (2019) Sexual dimorphism in innate immunity. Clin Rev Allergy Immunol 1: 1-4.
- Dryden M, Baguneid M, Eckmann C, Corman S, Stephens J, et al. (2015) Pathophysiology and burden of infection in patients with diabetes mellitus and peripheral vascular disease: focus on skin and soft-tissue infections. Clin Microbiol Infect 21: 27-32.
- Hu B, Zeng LP, Yang XL, Ge XY, Zhang W, et al. (2017) Discovery of a rich gene pool of bat SARS-related coronaviruses provides new insights into the origin of SARS coronavirus. PLoS pathogens 13(11): e1006698.
- Song HD, Tu CC, Zhang GW, Wang SY, Zheng K, et al. (2005) Cross-host evolution of severe acute respiratory syndrome coronavirus in palm civet and human. Proc Nati Acad Sci 102(7): 2430-2435.
- Yin Y, Wunderink RG (2018) MERS, SARS, and other coronaviruses as causes of pneumonia. Respirol 23(2): 130-137.
- Song Z, Xu Y, Bao L, Zhang L, Yu P, et al. (2019) From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses 11(1): 59.
- Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, et al. (2020) COVID‐19 patients' clinical characteristics, discharge rate, and fatality rate of meta‐analysis. J med Virol 92(6): 577-583.
- Chen L, Liu HG, Liu W, Liu J, Liu K, et al. (2020) Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 43(0): 005.
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229): 1054-1062.
- Singer M, Deutschman CS, Seymour CW, Shankar HM, Annane D, et al. (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). Jama 315(8): 801-810.
- Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. Jama 286(14): 1754-1758.
- Wang J, Zhou M, Liu F (2020) Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp infect 105(1): 100-101.
- Yang M, Ng MH, Li CK (2005) Thrombocytopenia in patients with severe acute respiratory syndrome. Hematology 10(2): 101-105.
- Jolicoeur P, Lamontagne L (1995) Impairment of bone marrow pre-B and B cells in MHV3 chronically infected mice. Adv Exp Med Biol 380: 193-195.
- Han Y, Zhang H, Mu S, Wei W, Jin C, et al. (2020) Lactate dehydrogenase, a risk factor of severe COVID-19 patients. MedRxiv.
- Zhang, Hu, Luo, Fang, Chen, et al. (2020) Clinical features and outcomes of 221 patients with COVID-19 in Wuhan, China. MedRxiv 127: 104364.
- Zhao J, Yang Y, Huang HP, Li D, Gu DF, et al. (2020) Relationship between the ABO Blood Group and the COVID-19 Susceptibility. MedRxiv.
- Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, et al. (2020) Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiological study. MedRxiv.
- Hegarty PK, Kamat AM, Zafirakis H, Dinardo A (2020) BCG vaccination may be protective against Covid-19. Indian J Tuberc.
- Bilan N, Dastranji A, Behbahani AG (2015) Comparison of the spo2/fio2 ratio and the pao2/fio2 ratio in patients with acute lung injury or acute respiratory distress syndrome. J Cardiovasc Thorac Res 7(1): 28-31.
- Yamada T, Wakabayashi M, Yamaji T, Chopra N, Mikami T, et al. (2020) Value of leukocytosis and elevated C-reactive protein in predicting severe coronavirus 2019 (COVID-19): A systematic review and meta-analysis. Clinica Chimica Acta 509: 235-243.
- Li YX, Wu W, Yang T, Zhou W, Fu YM, et al. (2020) Characteristics of peripheral blood leukocyte differential counts in patients with COVID-19. Zhonghua Nei Ke Za Zhi 59: E003.
- Mastaglio S, Ruggeri A, Risitano AM, Angelillo P, Yancopoulou D, et al. (2020) The first case of COVID-19 treated with the complement C3 inhibitor AMY-101. Clin Immunol 215: 108450.
- Tan L, Wang Q, Zhang D, Ding J, Huang Q, et al. (2020) Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther 5(1): 33.
- Guo T, Fan Y, Chen M, Wu X, Zhang L, et al. (2020) Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA cardiology 5(7): 1-8.
- Terpos E, Ntanasis SI, Elalamy I, Kastritis E, Sergentanis TN, et al. (2020) Hematological findings and complications of COVID‐19. Am J Hematol 95(7): 834-847.
- Lippi G, Plebani M, Henry BM (2020) Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta 506: 145-148.
- Zulfiqar AA, Lorenzo VN, Hassler P, Andrès E et al. (2020) Immune thrombocytopenic purpura in a patient with Covid-19. N Engl J Med 382(18): e43.
- Yang X, Yang Q, Wang Y, Wu Y, Xu J, et al. (2020) Thrombocytopenia and its association with mortality in patients with COVID‐19. J Thromb Haemost 18(6): 1469-1472.
- Ling W (2020) C-reactive protein levels in the early stage of COVID-19. Med Mal Infect 50(4): 332-334.
- Tan C, Huang Y, Shi F, Tan K, Ma Q, et al. (2020) C‐reactive protein correlates with computed tomographic findings and predicts severe COVID‐19 early. J Med Virol 92(7): 856-862.
- Zheng Z, Peng F, Xu B, Zhao J, Liu H, et al. (2020) Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect 81(2): 16-25.
- Liu F, Li L, Xu M, Wu J, Luo D, et al. (2020) Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol 127: 104370.
- Yuan J, Zou R, Zeng L, Kou S, Lan J, et al. (2020) The correlation between viral clearance and biochemical outcomes of 94 COVID-19 infected discharged patients. Inflamm Res 69(6): 599-606.
- Zhao D, Yao F, Wang L, Zheng L, Gao Y, et al. (2020) A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infec Dis 71(15): 756-761.
- O’Neill LA, Netea MG (2020) BCG-induced trained immunity: can it offer protection against COVID-19? Nat Rev Immunol 20(6): 335-337.
- Escobar LE, Molina CA, Barillas MC (2020) BCG vaccine protection from severe coronavirus disease 2019 (COVID-19). Proc Natl Acad Sci U S A 117(30): 17720-17726.
- Urashima M, Toyoda S, Nakano T, Matsuda S, Kobayashi N, et al. (1992) BUN/Cr ratio as an index of gastrointestinal bleeding mass in children. J Pediatr Gastroent Nutr 15(1): 89-92.
- Zhu N, Zhang L, Zhang H, Fengyu XI, Feng T (2017) Clinical Significance of Serum Bun, Cr, Cys C and RBP Combined Detection for Early Diagnosis of Renal Damage in Patients with Lupus Nephritis. J Mod Labor Med 32(2): 114-116.
- Yang J, Zheng Y, Gou X, Pu K, Chen Z, et al. (2020) Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Inter J Infect Dis.
- Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, et al. (2020) Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. Eur Respir J 55(5): 2000547.
- Homan TD, Cichowski E (2019) Physiology, pulse pressure. InStatPearls [Internet].
- Johnson P (2016) Practical Assessment of Volume Status in Daily Practice. Top Companion Anim Med 31(3): 86-93.
- Zhao Q, Meng M, Kumar R, Wu Y, Huang J, et al. (2020) Lymphopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A systemic review and meta-analysis. Int J Infect Dis 96: 131-135.
- Bermejo JF, Martín FM, López MC, Duque P, Almansa R (2018) Shared features of endothelial dysfunction between sepsis and its preceding risk factors (aging and chronic disease). J Clin Med 7(11): 400.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223): 497-506.
- Li J, Wang X, Chen J, Zuo X, Zhang H, et al. (2020) COVID‐19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab 1-7.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.