Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Is 1.5% Glycine a Comfortable Assistant in the Performance of Operative Hysteroscopy?
*Corresponding author: Harris E Phillip, Consultant Obstetrician and Gynecologist, Flat 17 Centrum Courts, 2 Pooley’s yard, Ipswich IP2 0AR, United Kingdom
Received: October 12, 2020;Published: October 22, 2020
DOI: 10.35097/AJBSR.2020.10.001547
Abstract
A Hysterectomy is the most frequently performed major gynaecological surgery. Benign causes are the most frequent indication for this procedure. Since this procedure is associated with significant morbidity; It was necessary to develop less invasive tools which could effectively address many non-cancerous indications which hitherto led to a hysterectomy. The hysteroscope emerged and with it was developed hysteroscopic surgical skills.
Materials and method: We searched the literature, (google scholar, PubMed, Mesh, CINAHL, EMBASE, Scopus) using search terms : Operative Hysteroscopic intravascular absorption syndrome, Fibroid uterus, endometrial ablation, rollerball endometrial ablation and did not find any case or case series with the specifics of our case. Though the need for less invasive portals in the management of benign gynaecological pathology is to be encouraged, these less invasive procedures are occasionally accompanied by serious complications. We present a case of an operative hysteroscopy intravascular absorption syndrome (OHIA). A number of observations were made with this case which can be used to effectively inform practice going forward.
Contributing factors to this complication could be identified at both the pre-operative and the intraoperative stages. We have outlined a plan for the effective management of this condition which begins with appropriate patient selection, pre-operative endometrial preparation, a high level of suspicion, close input /output charting and early recognition of the condition. Appropriate and timely management of the syndrome once identified, is essential to reduce a potentially fatal complication to a mild case of inconvenience. A Case report of Operative Hysteroscopic intravascular absorption Syndrome (OHIA) with a review of the literature.
Introduction
Annually over 75,000 hysterectomies are performed in the United Kingdom [1] and 600,000 in the USA. About 60% of which are for benign causes. This is the second most common surgery American women undergo with 43% of American women having a hysterectomy by the age of 85 years. Among the commonest reason for a hysterectomy is heavy menstrual bleeding. This procedure even in expert hands is not without risk. Among the risks are factors attendant to the procedure such as blood loss, pain, infection, pelvic visceral injury, deep vein thrombosis and/or pulmonary emboli and the morbidity associated with the recovery from this major surgical intervention. To reduce these undesirable effects, efforts have been made to develop less invasive and less morbid practices to treat many benign hysterectomy indications such as intractable menstrual bleeding. These efforts have been greatly facilitated with the development of the hysteroscope and endometrial ablative devices.
Materials and Methods
We searched the literature, (google scholar, PubMed, Mesh, CINAHL, EMBASE, Scopus) using search terms : Operative Hysteroscopic intravascular absorption syndrome, Fibroid uterus, endometrial ablation, rollerball endometrial ablation and did not find any case or case series with the specifics of our case. Though the need for less invasive portals in the management of benign gynaecological pathology is to be encouraged, these less invasive procedures are occasionally accompanied by serious complications. We present a case of an operative hysteroscopy intravascular absorption syndrome (OHIA). A number of observations were made with this case which can be used to effectively inform practice going forward.
The Case
A 48-year-old obese patient (BMI 50) was referred to (HEP) by a colleague for an endometrial ablation. The indication for the procedure was intractable menorrhagia. The colleague’s preoperative endometrial assessment revealed benign endometrium. An examination under anaesthesia prior to the ablative procedure revealed that this patient had an 18-week sized fibroid uterus. The uterine cavity was sounded to 11.5cm from the external os to the fundus. The intracervical length measured 5cm and the length from the internal os to the fundus was measured at 6.5 cm, the cavity width was recorded at 4.5cm. Nova sure endometrial ablation was appropriately attempted.
The cavity integrity check was fired and failed on three successive occasions. After the third failed attempt, the procedure was converted to a roller ball endometrial ablation. The cervix was dilated to size 10 hegar and a 1.5% glycine solution was used as the distending medium. The fluid recovered was collected with the use of a specialized drape placed under the patient’s buttocks. This allowed fluid spilled and recovered during the procedure to drain into a pouch which was aspirated, and the volume measured.
Within 10 minutes of commencing the procedure, having completed ablation of the fundus and the left side wall of the endometrial cavity, the fluid deficit was 2 liters. The procedure was immediately stopped, the patient was given 20mg of furosemide intravenously and she was catheterized. Blood was drawn for urea and electrolytes; a full blood count and clotting parameters were assessed. A diagnostic laparoscopy was immediately performed on the patient to ensure that there was no perforation of the uterus, and if there was any, to treat it and reduce the glycine load to the patient by aspirating any free fluid from her pelvis.
The initial urea and electrolyte value showed marked hyponatremia of 119mEq/L and mild hyperkaliemia of 5.3mEq/L. A repeat urea and electrolyte three hours later showed an improvement in the sodium level to 125mEq/L with a potassium level of 5.0mEq/L. The patient was hospitalized and observed in a High Dependency Unit setting overnight. A repeat of the patient’s urea and electrolytes later that evening reported a sodium level of 128mEq/L. She was communicating intelligently, and she had no signs nor symptoms suggestive of pulmonary oedema, cerebral oedema, or neurological deficit. I apologized to the patient the following day and explained to her the reason for stopping the procedure. She was discharged home later that day.
Intraoperative and post-operative findings
- A glycine deficit of 2 liters
- No free fluid seen in the patient’s pelvis
- No uterine perforation.
- Hyponatremia
- Amild hyperkalemia
- A reasonable rapid recovery
How was this possible?
This was most definitely, a case of operative hysteroscopic intravascular absorption syndrome.
There were several plausible factors which could have contributed to this condition
- The size of the uterus
- the presence of large uterine fibroids doubtlessly being fed by large blood vessels made for easy infusion of the distending medium into this patient’s circulation
- The large endometrial cavity. The distending medium would therefore have to be under greater pressure to ensure that the cavity is kept open and visibility assured
- The pressure of the distending medium in the endometrial cavity was maintained by the distending medium being forced in through the combination of exaggerated gravity with a pressure cuff placed around the bag with the distending fluid and the pole on which the distending medium was placed being raised progressively higher. The unprepared nature of the endometrium
- The type of anaesthesia.
The finding of no free fluid in the pelvis at the time of laparoscopy would suggest
- The pressure of the fluid entering the endometrial cavity was sufficient to drive the distending medium into the intravascular circulation
- The distending medium which entered the patient’s pelvis was very rapidly absorbed, as it is usual to see fluid in the pelvis when a hysteroscopy performed with normal saline as the distending medium is followed by a laparoscopy, and
- Glycine absorption from the pelvis is unusually rapid.
The pronounced hyponatremia of 119mEq/l and a deficit of 2 liters of the glycine solution would be expected if the 2 liters deficit entered the intravascular circulation [2].
The Review
Though the development of the hysteroscope can be traced back to [3] in 1806, the first successful hysteroscopy was performed by [4] in 1869. In 1981 the first practical method of hysteroscopic endometrial ablation was described. Since then, the tools have undergone significant refinement and the technique is more widely used leading to increase utility and success rates and a relative decline in the complication rates.
With the development of an increased skill set and confidence, the operative usefulness of the hysteroscope has evolved. Routine endometrial ablation for benign gynaecological conditions have benefited from second and third generation ablative devices in which visualization of the endometrial cavity during the procedure is unnecessary. However, these tend to have a fixed functional utility range which influences their best usefulness.
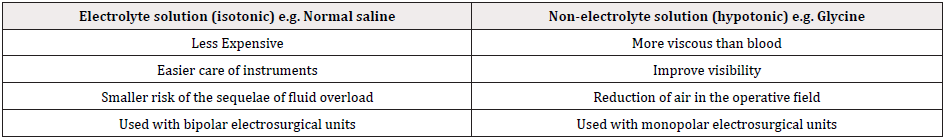
Operative hysteroscopic procedures in which visualization of the endometrial cavity during the procedure becomes an absolute necessity requires a distending medium. The first-generation instruments such as the resectoscope and the second generation myosure are used to resect large endometrial polyps, submucosal and type 0 fibroids. The first generation resectoscope functions using a mono polar current whereas myosure uses a bipolar current (Table 1).
Distending media available are placed into two broad categories a) Nonelectrolyte and b) An electrolyte. In monopolar usage the electrolyte tends to dampen the effect of the current thus reducing its power density. To be effective and to reduce the risk of injury, the monopolar current is more safely used in a non-electrolyte medium. For bipolar electrosurgical units, it is safe to use an electrolyte as the distending medium. Among the more commonly used electrolyte preparations are Hartman's solution and normal saline. The non-electrolytes in common use are mannitol 5% which is isotonic, 1.5% glycine, 3% sorbitol, and 5% Dextrose which are all hypotonic. The remainder of the discussion will be focused on the complication of Operative Hysteroscopic Intravascular Absorption (OHIA) as seen in this case report.
Operative hysteroscopic intravascular absorption syndrome (OHIA
)This defines a condition in which excessive amounts of the distending medium used in operative hysteroscopy is absorbed into the patient circulation leading to fluid overload and its attendant toxicity syndrome [5]. It is like prostate TURP syndrome [6].
Discussion
Guidelines from the British Society of Gynecological Endoscopy (BSGE) [7] and the European society of Gynecological Endoscopy (ESGE) [7] consider a threshold of 1000ml can be absorbed without significant ill effect while using hypotonic non-electrolyte solutions, whilst a volume of 2,500mls of isotonic electrolyte solution as used with bipolar electrosurgical units can be absorbed without significant sequelae in healthy women. In women with pre-existing co-morbidities, the allowable volumes are lower, 750mls for non-electrolyte hypotonic media and 1500mls for isotonic media.
These patients with OHIA may present suddenly but because of the effect of the anaesthesia, the condition may not be readily detectable. If the patient is under general anaesthesia for example, early signs may be masked. The most useful marker would therefore be monitoring the fluid deficit using the values suggested by both BSGE and ESGE. If the guidance is closely followed, monitoring of the input/output volumes and calculating the fluid deficit, every 10 minutes, would greatly reduce the incidence of this complication. In our patient, though, there was a negative balance of 2 liters within 10 minutes.
Features
Earliest features may be noted by an observant anesthetist, there will be a drop in the peripheral capillary oxygen saturation (Sp02) and concomitant rise in Airway Pressure with diminished breath sounds and tachycardia. Blood pressure may also drop. If the patient is awake, she will experience headaches, visual disturbance, and nausea; she may vomit.
Blood studies will reveal hyponatremia, hyper kalmia, hypoosmolality and metabolic acidosis.
Clinical examination may reveal features of pulmonary and cerebral oedema. Operative hysteroscopic intravascular absorption syndrome is reported in world literature as a rare entity occurring in less than 5% of women [8] and virtually identical to TURP syndrome seen in about 1.1% of men.
Aupleniz et al. reported an incidence of fluid overload in 0.1 to 0.2% in his series of 21,676 hysteroscopes. In the patient above the fluid was driven into the endometrial cavity through an extension of the gravity system using a simple pressurized delivery system which was created by positioning a pressure cuff around the bag filled with glycine. This approach unfortunately does not allow for the precise control of the pressure with which the distending fluid is driven through the endometrial cavity. Additionally, with a large uterus, higher pressures are required for appropriate visualization.
Doubtlessly the 18 weeks sized uterus would have presented a relatively larger surface area for the glycine to be absorbed, and large vessels feeding these fibroids would have provided easy direct access of the pressurized glycine to the patient’s circulation. Adding to this is the difficulty of accurately calculating the systemic absorption which can be complicated by at least four factors
- It may be difficult to collect all the media that passes out of the uterus including that which falls on the procedure or operating room floor,
- The actual volume of media solution in 3-liter bags is typically more than the labelled volume,
- Difficulties in estimating the volume of media left in a used or emptied infusion bag and
- Systemic absorption of the distending fluid can be very rapid.
Bergeron ME (2009) [9] indicated that the choice of anaesthesia impacts on fluid absorption with larger volumes of fluid absorbed in patients under general anaesthesia than with sedation and local anaesthesia. Glycine though, a useful distension medium in improving visibility during hysteroscopic surgical procedures and being a poor conductor of electricity is ideal with the use of monopolar electrosurgical units for performing operative hysteroscopic procedures. The operative hysteroscopy, however, must be cautiously observant and cannot be overly comfortable.
Mechanism
OHIA results from the distension medium entering the intravascular space. The distension medium can be absorbed into the intravascular space through three different portals
- Distension medium flowing through the fallopian tube and entering the peritoneal cavity from where it is absorbed,
- Directly through the endometrium, so the larger the endometrial cavity, the greater the relative surface area available through which absorption can occur and
- Directly through broken vessels, sinuses or superficial vessels in a vascular endometrium.
The rate at which the absorption occurs is influenced by the pressure of the distending medium within the endometrial cavity. The higher the pressure of the distending fluid relative to the mean arterial pressure, the more likely fluid will flow from the distending medium into the intravascular space. The bigger the cavity the greater the pressure of the distending medium required to appropriately visualize the endometrial cavity.
The distending medium enters the intravascular space at a variable rate which is dependent on the pressure of distending medium within the endometrial cavity, the size of the channel through which the fluid enters, duration of the operative procedure and the depth of incursion into the myometrium.
If the fluid is hypotonic, relative to plasma, as is the 1.5% glycine, a concentration gradient is established in which the distending medium will flow from the hypotonic extravascular fluid into the cells which causes them to swell. This is most harmful in the brain. The brain cells cannot distend significantly because of the bony skull. As a result, the patient, if awake, may develop prickling sensation in the face and neck as well as restlessness, headaches, visual disturbances, nausea, and projectile vomiting depending on the volume of fluid absorbed.
Herniation of the brain stem and death may also occur. The syndrome in its most severe form has a 25% mortality rate [8,10] reports a 50% mortality rate in his case series.
It is believed that the mechanism of this syndrome is based on the Na+/K+ ATPase pump. Initially, the brain responds to the incursion of the distension medium through the Na+/K+ ATPase pump. The pump uses ATP to transfer 3Na+ out of the cells into the extracellular fluid and transfer 2K+ into the cells. The functioning of this Na+/K+ ATPase pump is believed to be influenced by sex hormones [11]. It is inhibited by estrogen. The syndrome is seen more commonly among the pre-menopausal women. Hence premenopausal women are 25 times more likely to suffer from the syndrome and have permanent brain damage than men or postmenopausal females. Sex steroid impact on the Na+/K+ ATPase pump can be pre-empted by pre-op use of a gonadotrophin- releasing hormone analogue (GnRHa). Unfortunately, the patient above had no pre-op GnRHa. In patients with this syndrome, there is an elevated level of vasopressin which may exacerbate or even cause the syndrome.
Management
The management of this condition can be divided into preoperative preparation, the intraoperative and postoperative management/treatment.
Pre-operatively
Careful and proper patient selection.
Appropriate counselling informing the patient of the risk associated with the procedure. Discussion on the type of anaesthesia and the need for the use of preoperative GnRHa. If the patient has decided to use a general anesthetic, discussion with regards to the addition of 1% ethanol [12] to the distending medium is advisable. This allows for early detection of intravascular absorption of the distending medium, by being able to detect ethanol breath.
Intra-operatively
- Strict attention to Input/output every 5-10 minutes, (a good rule of thumb would be 5 minutes in the case of a larger uterus greater than 8 week size and in which there is significant endometrial destruction and 10 minutes in the case of smaller sized uterus's)
- A high index of suspicion
- Preference for regional anaesthesia. This will allow for the identification of the Miners canary [13] which portends impending brain or cardiac dysfunction. If a general anesthetic is used, the need for an attentive anesthetist, the ability to perform the ethanol breath test and to assess the parotid area sign [14] would be additional sources of reassurance.
- Once the deficit reaches a liter the procedure must be stopped in a fit healthy patient, in a patient with co morbidities, if the deficit reaches 750mls, the procedure must be stopped.
Medical Management
- Loop diuretic e.g. furosemide intravenously to induce diuresis and to treat acute pulmonary oedema, if present (Hahn 2006)
- Catheterise the patient to facilitate input/output measurement.
- Relevant bloods such as U+E, FBC and clotting
- Imaging of the chest (X-ray)
- If sodium is less than 120mmol, consider 3% NaCl at 100 mls/hr. This can be repeated three times, then a slower infusion of 3% NaCl can be continued at a rate of <1m mol/L/ till the Na+ is corrected. Rapid correction can lead to Pontine myelinolysis [14-15].
- The patient must be observed in a high Dependency /ICU setting till signs of stability are noted.
- VTE prophylaxis in the form of mechanical compression devices is advised.
Conclusion
Whereas we believe that Randomized control trials (RCTs) represent the gold standard in clinical research to inform protocol and guidelines development; We believe that case reports and case series make an important contribution to the medical literature. RCTs are restrictive and may fail to explore features unique to a particular case through its fabricated inclusion and exclusion criteria. Case reports on the other hand, are able to delve into features unique to the specific case, thereby advising on the approach to similar cases. Case reports must be included in the medical literature to improve our knowledge and inform our practice.
We wish to avoid the common pitfall of case reports. We will not make an outlandish claim after a single observation, but we believe our case highlights several learning points that cannot be ignored:
- The risk of OHIA is increased in the larger uterus,
- The need for closer attention to the distending medium deficit with a shorter time interval of 5 minutes in the larger uterus as opposed to the suggested 10-minute interval.
- Our case dispels the view that significant destruction of the endometrium is necessary for OHIA since the rollerball technique was employed and less than half of the cavity had been ablated.
- The role of the intra cavity pressure of the distending medium is highlighted, as plausibly among the most important factor leading to OHIA.
It also suggests that in large uterine cavities, the use of bipolar instruments is a safer option, since a larger volume of distending medium can be absorbed before OHIA can be manifested.
References
- Hysterectomy.
- Magos AL, Baumann R, Lockwood GM, Turnbull AC (1991) Experience with the first 250 endometrial resections for menorrhaggia. Lancet 337(8749): 1074-1078.
- Philipp Bozzini.
- Tarneja P, Duggal BS (2011) Complications of Hysteroscopic Surgery. Med J Armed forces India 58(4): 331-334.
- Jackson S, Lampe G (1995) Operative hysteroscopy intravascular absorption syndrome. West J Med 162(1): 53-54.
- Serocki G, Hanss R, Bauer M, Scholz J, Bein B (2009) The gynaecological TURP Syndrome, Severe hyponatremia and pulmonary oedema during hysteroscopy. Anaesthesist 58(1) 30-34.
- Umranikan S, Clarke TJ, Saridogan E, Miligkos D, Arambage K, et al. (2016) BSGE/ESGE guideline on management of fluid distension media in Operative Hysteroscopy. Gynecol surgery 13: 289 -303.
- Hahn RG (2006) Fluid absorption in endoscopic surgery. Br J Anaesth 96(1): 8-20.
- Bergeron ME, Ouellet P, Bujold E, Cote M, Rhéaume C, et al. (2011) The impact of anesthesia on glycine absorption in operative hysteroscopy: a randomized controlled trial. Anesth Analg 113(4): 723-728.
- Baggish MS, Andrew IB, Rosenswerg B, Barbot JE, Indman PD (2009) Fetal Acute glycine and sorbitol Toxicity during operative hysteroscopy. Journal of Gynecologic surgery 9: 3.
- Taskin O, Buhur A, Birincioglu M, Burak F, Atmaca R, et al. (1998) Endometrial Na+, K+-ATPase pump function and vasopressin levels during hysteroscopic surgery in patients pretreated with GNRH agonist. J Am Assoc Gynecol Laparosc 5(2): 119-124.
- Hall JM, Tingey WR, Gillmer MD (2003) The use of glycine-ethanol irrigating fluid for the early detection of fluid absorption during endometrial resection. Gynaecol Endosc 6(1): 39-44.
- Sethi N, Chaturvedi R, Kumar K (2012) Operative hysteroscopy intravascular absorption Syndrome: A bolt from the blue. Indian J Anaesth March April 56 (2): 179 -182.
- Sinha M, Hegde A, Sinha R, Goel S (2007) Parotid area sign: A clinical test for the diagnosis of fluid overload in hysteroscopic surgery. J Minim Invasive Gynecol 14(2): 161-168.
- Glacsser MH (2005) Hysteroscopy: Managing and minimising operative complications. OBG Management 17(2): 42-57.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.