Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Nissen Fundoplication Vs Linx
*Corresponding author: Shivani Modi, American International Medical University, 2901 South King Dr, Apt 115, Chicago IL-60616, USA
Received: Setember 09, 2020;Published: November 10, 2020
DOI: 10.34297/AJBSR.2020.10.001568
Abstract
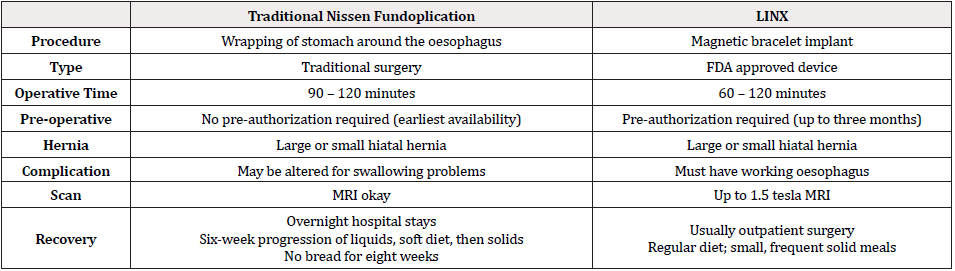
Gastroesophageal reflux disease, or GERD, is a digestive disorder that affects the lower oesophageal sphincter (LES), the ring of muscle between the oesophagus and stomach. Symptoms of GERD include heartburn, food reflux, chest pain, difficulty swallowing, sensation of lump. In throat, long-term GERD can lead to chronic cough, laryngitis, worsening of asthma. GERD is extremely common, with a prevalence of approximately 20% of adults in the western culture. The primary options for treatment have been proton pump inhibitors (PPI) or laparoscopic Nissen fundoplication (LNF) [1]. Although medications provide excellent symptom relief in most individuals, for some patients antisecretory medications fail to provide relief [1]. For such patient’s anti-reflux restorative surgery should be considered. Usually the traditional choice of treatment has been a 360° (Nissen) fundoplication. In numerous patients, this result is not too bad with suitable reflux control and durability for up-to 20 years. Disastrously, a subset of around 10 to 15 percent are not actually content with their outcome following Nissen fundoplication, on account of either irregular reflux reactions, or side effects, for instance, dysphagia, bloating and flatulence. This unexpected outcomes and invasiveness of the surgery there are a lot of patients who are unwilling to take up such option despite medically not managed GERD symptoms. Alternative treatment options have been developed, which includes four new devices—LINX, TIF, EndoStim and Stretta—have attempted to improve upon the limitations of these traditional therapies. Considering the new therapies, LINX has met patient’s concerns and also reduced adverse outcomes of Nissen’s [2]. LINX magnetic sphincter augmentation system (MSA) is a surgical technique with short-term evidence demonstrating efficacy for the treatment of GERD. Treatment with the LINX Reflux Management System diminishes costs compared to laparoscopic Nissen fundoplication (LNF). Also, LINX is less invasive comparatively. Currently, Nissen fundoplication is only the gold standard surgery for GERD [2]. Although, initial clinical trials show that LINX is more efficious and safe. In this review, we will compare meta-analysis for Nissen Fundoplication and LINX as a treatment for GERD, comparing the efficacy, safety, cost of surgery, invasiveness, and adverse outcomes.
Keywords: Gastroesophageal reflux Disease, GERD, LINX, Magnetic Sphincter augmentation system, MSA, Management, Nissen Fundoplication.
Introduction
Gastroesophageal reflux (GERD) impacts up to 27.8 % of adults in North America, and the recurrence has been extending. The fundamental decisions for treatment have been proton pump inhibitors (PPI) or laparoscopic Nissen fundoplication (LNF). By a long shot the greater part of patients are managed PPIs with extraordinary control of their symptoms. Regardless, what was at one time a panacea for treating GERD has been broken down by continuous data, suggesting that PPIs are not as effective as acknowledged, with only 32 % of patients achieving complete sign relief, and various reports including side-effects and adverse reactions, for instance, pneumonia, Clostridium difficile defilement, fracture, decreased magnesium absorption, thrombocytopenia, iron need, supplement B12 inadequacy, rhabdomyolysis and acute interstitial nephritis.
Right when patients get treatment for gastroesophageal reflux, they need their symptoms to be soothed. They furthermore should not be bother with the treatment to make another issue which leaves them more horrible off than before their therapeutic technique [3]. The challenge here is to find a commendable outcome for all patients contemplating restorative strategy for reflux, and this has incited a consideration on systems that control reflux, yet also limit the risk and impact of the side effects which can seek after Nissen fundoplication. Therefore, numerous treatment options have been presented rather than NF. TIF and MSA were endorsed by the U.S. Sustenance and Drug Administration (FDA) in 2007 and 2012. MSA is one of the most recent techniques to treat GERD utilizing LINX framework. Be that as it may, the present literary works partner with adequacy of MSA and contrasting with Nissen medical procedure. Consequently, it is basically important to get a thorough comprehension on the differences, efficacy, and safety by comparing MSA and NF for GERD.
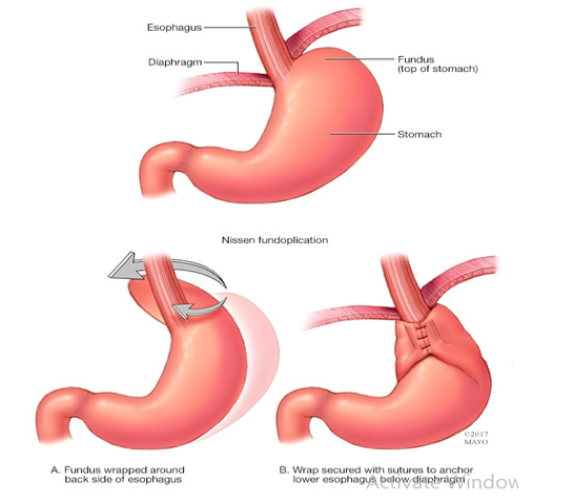
Patient is kept under general anaesthesia. Four small incisions are made at the abdomen around the stomach. A tube is passed through one of the incisions which has light and camera placed which guides the surgeon throughout the surgery. Upper part of the abdomen called the fundus is wrapped around the oesophagus, which strengthens the lower oesophageal sphincter. This whole procedure is called Nissen Fundoplication, which is named after Doctor Rudolph Nissen, who first performed the surgery in 1955 and published the results in 1956 [4,5].
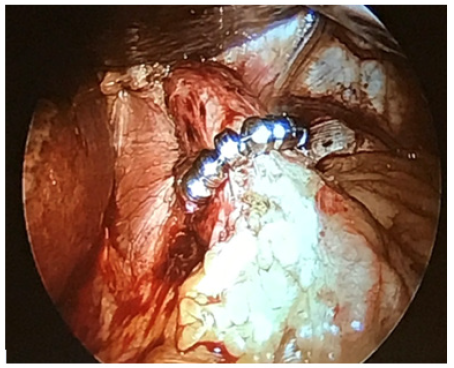
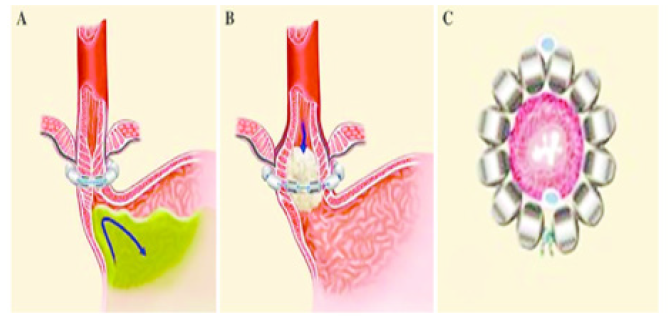
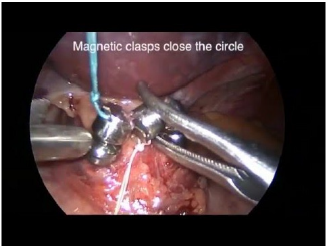
LINX Reflux Management Surgery is a band which is made up of magnetic beads covered by titanium casing and interconnected by titanium wiring. The core is made up of magnet [3]. The magnetic core allows the structure to stay in contracted form at rest as shown in Figure 1 [6]. When the bolus passes the ring expands and lets the food pass to the stomach as shown in Figure 2A [7]. The force with which the bolus passes from oesophagus to stomach is higher compared to the force with which bolus passes from stomach to oesophagus as shown in Figure 2B [7]. The device is available in multiple sizes ranging from 13 to 17 beads. Patient is under general anaesthesia; four incisions are made same as in Nissen Fundoplication. A tube is inserted with light and camera which helps the surgeon throughout the surgery [4,5]. The pars flaccida of the gastrohepatic ligament is opened to expose the right crus of the diaphragm. The appropriate position of the MSA device is two centimeters proximal to the gastroesophageal (GE) junction as determined laparoscopically by the gastric fat pad. The ends of the device and locked and placed in position as shown in Figure 3 [8].
Methods
Study Selection
Author performed meta-analysis search independently using PUBMED, EMBASE, OVID, and Cochrane database. Search was performed on all studies comparing data from MSA and NF from the year 2009 to 2018. Only studies on humans and in English were considered for inclusion. Reference lists of all retrieved articles were manually searched for additional studies. Out of around 60 articles, 25 were taken into consideration after doing data analysis and inclusion criteria.
Inclusion Criteria
Articles were included in meta-analysis if they fulfilled the following criteria a) Comparing original outcomes for MSA and NF as choice of treatment for GERD. b) Comparison between adverse outcomes, blood loss, symptom relief and proton pump inhibitor use.
Exclusion Criteria
Articles were excluded from meta-analysis if; a) This was second surgery for GERD. b) Articles, scripts, cases, reports which lack a control group or not a direct comparison was made. c) TIF was used as treatment of choice.
Statistical Analysis
Patient’s in different age group were compared. Patients who underwent MSA and LNF were compared. Proton-pump inhibitor use, the number or incidence of adverse events, and complications (postoperative dysphagia, belch, and vomit) were analysed. Heterogenicity of the studies were considered and random effects were taken into consideration. All statistical data were considered significant. The confidence interval considered for this research is 95%. If It was less than 5% of a chance occurrence (P < 0.05), all statistical data were considered significant. On the off chance that accessible, the RRs with their 95% CIs and P esteems were gathered from the first article or the comparing E-sends. If not, we determined RRs and their 95% certainty interim utilizing the information of tests in each gathering or the information given by the creators. In the event that just Kaplan–Meier bends were accessible, we separated information from the graphical survival plots and assessed the RRs.
Results
Of the 20 clinical trials that initially met the inclusion criteria, 13 did not display the specific comparison of the effects of MSA and NF, 4 did not provide enough original data. Finally, 3 retrospective studies matched the selection criteria and were published between 2009 and 2018. A total of 874 patients consisted of 387 in the MSA group and 487 in the NF group. In this section the author will go in details with different kind of complications that would take place during this treatment with patients [4,9].
The 60 papers that is considered for this research is got after removal of duplicates of papers studied over a period. In these 60 papers, over 40 papers were considered were filtered based on patient’s data and titles which did not match with the study. Furthermore, filtering let to 20 papers which were considered in which 4 papers were removed as it did not have completed texts and 16 were considered which met the criteria. Out of these papers 10 papers were filtered out as it did not meet inclusion criteria. In the remaining 2 papers were removed from the lot of it was from the same author.
As an author I have gone through over 60 papers where I have chosen over 3 papers which had done research over 800 patients, all these 3 papers were used to extract the data and was used to derive outcomes, complications and different results obtained through their research.
Outcomes
GERD patients who underwent LNF or MSA, there is not much difference in the operative time, number of days stayed in the hospital, blood loss, or symptom relief. Various studies have been compared from the year of 2014 to 2016 and a graph is made comparing number, sex, mean age, BMI, OR time and length of stay for MSA surgery and LNF surgery as shown in Figure 4a-4b.
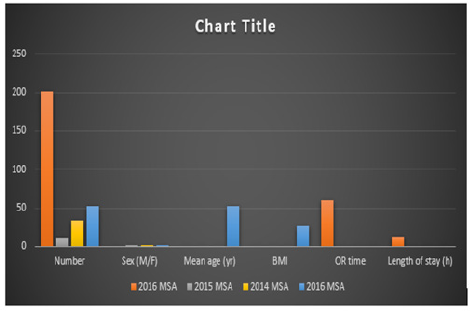
Figure 4A: Compares the number, sex, mean age, BMI, OR time and length of stay for MSA surgery for the year 2014,2015 and 2016 from different articles [4].
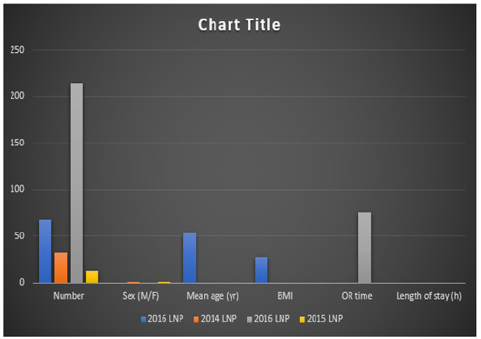
Figure 4B: Compares the number, sex, mean age, BMI, OR time and length of stay for MSA surgery for the year 2014,2015 and 2016 from different articles [4].
Complications
Huge post-usable dysphagia happened in most of MSA patients with the typical beginning of side effects 5-10 days post operation. Half of MSA patients required endoscopic dilation for progressing dysphagia with weight reduction, while no LNF patients required dilation. Requirement for expansion did not correspond with the size of LINX gadget, hiatal hernia, sex, BMI, or manometry. 33% of LNF patients complained of stomach swelling or hyper flatulence; no MSA patients complained these side effects. The two surgeries successfully treated reflux manifestations, with 75% of MSA and 83% of LNF patients relieving symptoms at a mean follow-up of 7 months. Contrasted with LNF, MSA patients had a shorter operative time. Post-operative hospital length of stay was identical in the two gatherings (1 versus 1.1 days) [4,10].
Conclusion
Gastroesophageal reflux ailment (GERD) is a stomach related issue that affects the lower oesophageal sphincter. The sphincter typically keeps food from moving out of the stomach and back up into the throat. At the point when an individual has GERD, the sphincter muscle ends up losing function, causing food and stomach acids to stream back (reflux) into the throat. The coating of the throat can end up aggravated or bothered from these acids. Individuals with serious, oesophageal reflux may require surgical procedure to address the issue if their manifestations are not diminished through medications. Whenever left untreated, chronic gastroesophageal reflux can cause long term issues, for example, esophagitis, oesophageal ulcers, or scarring of the oesophagus (Figure 5).
Laparoscopic Nissen Fundoplication is utilized in the treatment of GERD when medications are not effective. Laparoscopic Nissen Fundoplication is a minimally invasive procedure that remedies gastroesophageal reflux by making a compelling valve component at the base of the oesophagus by the upper part of the stomach, called the fundus. Laparoscopic Nissen fundoplication is an outpatient procedure that takes about an hour and a half to complete. Individuals treated with laparoscopic fundoplication can return home the day of medical procedure. Your PCP may approach you to take fluids for possibly 14 days after medical procedure and afterward slowly start with soft food.
The most common symptom of laparoscopic Nissen fundoplication is trouble swallowing after medical procedure. This goes on for just half a month, until your oesophagus gradually modifies. The fixed oesophageal muscle is at first so solid that gas may wind up caught in the stomach causing swelling and flatulence. Research has demonstrated that most by far of individuals who experience laparoscopic Nissen fundoplication never again require medicine for the treatment of GERD. The main stay surgery till today for the treatment for GERD is “Nissen fundoplication,” which can possibly cause adverse reactions that lead numerous delays in the surgery.
A year ago, the Food and Drug Administration affirmed another treatment called the LINX Reflux Management System to offer another way to deal with treating GERD, an infection that is expanding at a rate of 30 percent consistently. When patients undergo a procedure for gastroesophageal reflux, they want their symptoms to be cured. They also do not want the treatment to generate a new problem which leaves them worse off than before their surgery. The quest to minimize side effects has followed divergent paths in different parts of the world. Many surgeons have been reluctant to consider alternative fundoplication options which might reduce side effects [11].`
LINX is an adaptable ring of little magnets placed around the lower oesophageal sphincter. The attractive ring expands when a patient swallows bolus from oesophagus to the stomach allowing the food to pass through. Although it stays in contracted position at rest, not allowing the bolus and acid to pass from stomach to the oesophagus [9]. There are various studies going on about the LINX procedure, amongst which one is a study performed in 2019 in Highmark Health’s Allegheny Health Network showing that LINX is more cost effective than LNF [12].
LINX procedure eliminates most patients’ need for medications, along with the side effects associated with those medications, and nutritional deficiencies. LINX resolves moderate to severe regurgitation and issues with gas bloating. Limits long-term health effects of reflux disease, including oesophageal cancer, stricture and difficulty swallowing, chest pain, and pulmonary and ENT problems [13-16]. LINX also does not require anatomical alterations to the stomach as with a Nissen fundoplication. It is reversible unlike Nissen Fundoplication. LINX cannot be considered as a choice of treatment if the patient requires any other gastroesophageal surgeries. LINX is generally a same-day procedure and takes less than an hour. LINX also allows patients to resume a normal diet following surgery unlike LNF [16].
The adverse effects include dysphagia, bloating/gas, difficulty to burp and regurgitation at low rates in both MSA and LNF [17-20]. Unfortunately, dysphagia remains the most continuous and serious postoperative complexity. Obviously, side effect of dysphagia will be better and better in 1-2 week after the surgical procedure in most of the patients. In the event where dysphagia has not selfresolved in more than 3 months, endoscopic widening is required. If endoscopic dilation has failed, MSA device needs to be removed [21-25].
There are yet numerous unanswered inquiries whether MSA is yet suitable for hiatal hernias which are more than 3cm, regardless of whether the long-term outcomes of MSA are same as short-term outcomes. The incidence of LINX device removed and erosion will increase as time goes on, and so on. Thus, it is significant and important to perform randomized controlled trials to depict the viability of MSA compared with NF in short-term and long-term [26-28].
Conclusion
MSA is a novel careful choice for the administration of GERD. While MSA is simpler and quicker to perform than LNF. Dysphagia happens as an adverse effect in both MSA and LNF, although more frequently in MSA. There is not much difference between MSA and LNF when comparing the length of hospital or the operative time. Although, MSA is more preferable when it comes to adverse effects like bloating, flatulence and mild regurgitation initially after the surgery. Also, MSA is less invasive and reversible. However randomized controlled trials are required proving MSA as best therapeutic treatment than LNF depending on more evidence.
References
- Antunes C, Aleem A, Curtis SA (2020) Gastroesophageal Reflux Disease. Stat pearls.
- Heartburn Surgery. WebMD.
- Mazen R, Al Mansour, Kyle A, Perry, Jeffrey W Hazey, et al. (2017) The current status of magnetic sphincter augmentation in the management of gastroesophageal reflux disease. Annals of laparoscopic and endoscopic surgery 2(9).
- Ming Yu Chen, Di Yu Huang, Angela Wu, Yi Bin Zhu, He Pan Zhu, et al.(2017) Efficacy of Magnetic Sphincter Augmentation versus Nissen Fundoplication for Gastroesophageal Reflux Disease in Short Term: A Meta-Analysis. Can J gastroenterol Heptol 2017: 9596342.
- Jennifer L Wilson, Brian E Louie (2014) New Options for the Management of GERD. Esophageal/reflux surgery.
- Jaime ponce (2017) LINX procedure can alleviate reflux in post-bariatric surgery patients.
- Luigi Bonavina. The LINX device in the closed position. B the LINX device in the open position. C The closed position showing no compression of the esophageal wall. Research gate.
- (2016) LINX Reflux Management System Procedure.
- Daniel Skubleny, Noah j A Switzer, jerry dang, Rich deep S gill, Xinzhe Shi, et al. (2013) LINX® magnetic esophageal sphincter augmentation versus Nissen fundoplication for gastroesophageal reflux disease: a systematic review and meta-analysis. Surg Endosc 31(8): 3078-3084.
- Eric G Sheu, Peter Nau, Barbara Nath, Braden Kuo, David W Rattner, et al. (2020) A Comparative Trial of linx versus lap nissen: caveats for patient selection. Sages.
- David I Watson (2019) Is LINX the way to go for GERD surgery? No. AGA
- http://www.bariatricnews.net/?q=news/113452/linx-reflux-system-reduces-costs-vs-laparoscopic-nissen-fundoplication.
- Katrin Schwameis, Milena Nikolic, Devis G, Sebastin F Schoppmann, Barbara Zoner, et al. (2018) Crural Closure improves Outcomes of Magnetic Sphincter Augmentation in GERD patients with Hiatal Hernia. Scientific Reports. 7319.
- LINX® Reflux Management System. Jnj medical devices.
- (2015) LINX, Nissen fundoplication comparably improve quality of life in chronic GERD patients. Healio.
- https://www.gundersenhealth.org/for-clinicians-professionals/medlink-news/issues/august-2018/linx-relieves-gerd-long-term-without-invasive-surgery-or-ppi-med/
- Ming Yu Chen, Di Yu Huang, Angela Wu, Yi Bin Zhu, He Pan Zhu, et al. (2017) Efficacy of Magnetic Sphincter Augmentation versus Nissen Fundoplication for Gastroesophageal Reflux Disease in Short Term: A Meta-Analysis. Can J Gastroenterol Hepatol.
- https://www.google.com/url?sa=i&source=images&cd=&cad=rja&uact=8&ved=2ahUKEwjsxv3qkrbjAhVpkeAKHcd-DVcQjRx6BAgBEAQ&url=https%3A%2F%2Fwww.mayoclinic.org%2Fdiseases-conditions%2Fgerd%2Fmultimedia%2Fgerd-surgery%2Fimg-20006950&psig=AOvVaw3iHqTkRzQ4RItWrsU0Ozbw&ust=1563252655513615
- Emily Speer (2017) Anti-Reflux Surgery Nissen Fundoplication or LINX System. National Jewish health.
- (2018) Nissen Fundoplication or LINX for Gastroesophageal Reflux Disease? The great debates.
- Surgery for gastroesophageal reflux disease. NYU langone Health.
- Baltimore (2019) LINX Reflux Management System Has Been Shown to Reduce Medical Costs More Than Traditional Anti-Reflux Surgery in First Year Following Procedure. Ethicon.
- https://www.gundersenhealth.org/for-clinicians-professionals/medlink-news/issues/august-2018/linx-relieves-gerd-long-term-without-invasive-surgery-or-ppi-med
- Steven D schwaitwaitzberg (2020) surgical management of gastroesophageal reflux in adults. Up to date.
- Joe Mehaffey, Daniel Smith, Mayo Clinic, Jacksonville Fl (2014) my recovery from Acid Reflux Surgery following Linx ring implant.
- Dengler (2018) ten things you need to know about LINX. Reflux MD.
- Laparoscopic Antireflux Surgery. Cleveland clinic.
- (2020) Nothing Tough to Swallow About This Data. Mddi qmed.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.