Research article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Pathophysiological Aspects of the Use of Hypobaric Hypoxic Training in the Treatment of Anemia in Chronic Glomerulonephritis
*Corresponding author: Murkamilov Ilkhom Torobekovich, Kyrgyz State Medical Academy, Kyrgyzstan.
Received: September 22, 2020; Published: October 05, 2020
DOI: 10.34297/AJBSR.2020.10.001527
Summary
The course of chronic glomerulonephritis (CGN) is often accompanied by the development of anemia, which contributes to the progression of chronic kidney disease (CKD) and, in severe cases, leads to death. Therefore, correction of renal anemia at the earliest stages of CKD is important, allowing to reduce the rate of progression of renal dysfunction and delaying the onset of renal replacement therapy. Currently, erythropoietin is widely used in the treatment of renal anemia, which, however, is not always available to most patients due to its high cost. In this regard, the possibility of using it for this purpose, along with erythropoietin, and hypobaric hypoxic training, anti-anemic efficacy of which is proved by numerous studies, is of interest. The purpose of the study is to evaluate the effectiveness of correction of anemia with erythropoietin (EPO ß) monotherapy and also in combination with hypobaric barocameral training (HBT) in chronic glomerulonephritis at the pre-dialysis stage.
Methods: Patients of the group I (n = 38), along with usual therapy in hospital conditions, received EPO ß monotherapy according to the standard procedure. EPO-beta was administered subcutaneously at an initial dose of 20-50 ME/kg, three times a week, until the target Hb level was reached. In Group II (n = 41), patients received courses of hypobaric barocameral training (HBT) in combination with EPO-beta at lower doses (20-50 ME/kg, once a week). In both groups, after achieving the target Hb level, maintenance dose of EPO ß for the entire observation period (24 months) was selected individually. The HBT course was carried out in a multi-seat medical hypobaric pressure chamber according to a standard procedure.
Results: A comparative analysis of the effectiveness of the therapy methods (EPO-beta and EPO-beta + HBT) showed that both methods have a pronounced anti-anemic effect (increase in hemoglobin level with a noticeable increase in the number of platelets, red blood cells and its indices), however, a decrease in the level of daily proteinuria in the group of patients, who received combined therapy (exogenous hypoxia + EPO-beta), was greater compared with the group receiving EPO-beta monotherapy [0,669 (0,210-1,468) g vs. 1,145 (0,600-2,310) g; p<0.05].
Conclusion: Combined (EPO-beta + HBT) therapy is not only inferior to the effectiveness of EPO beta monotherapy, but it also significantly (3 times) reduces the amount of erythropoietin necessary to reach the target hemoglobin level, which should be taken into account when treating anemia in patients with CKD.
Keywords: Chronic glomerulonephritis, Anemia, Erythropoietin, Hypobaric hypoxia
Introduction
Chronic glomerulonephritis (CGN) is the top cause of chronic kidney disease (CKD). The progression of CGN is significantly affected by anemia, which may be detected at an early stage of the disease [1,2]. According to certain studies, anemia in CKD can be observed at the glomerular filtrate rate (GFR) over 90 ml/min/1.73 m² in men and over 70 ml/min/1.73 m² in women [3,4]. In severe reduced kidney function, almost all patients with CKD develop anemia [1]. The main cause of the development of anemia in chronic renal failure (CRF) is a decrease in the synthesis of erythrocyte growth hormone – erythropoietin in the peritubular cells of the proximal part of nephron in renal scarring, resulting in relatively low plasma erythropoietin levels [5,6]. Shortening of erythrocyte life influences anemia development to a lesser extent. Under normal physiological conditions in the bone marrow, 95% of cells survive to be complete red blood cells entering the bloodstream which is called effective erythropoiesis.
Erythroid cells in CRF are more destroyed in the bone marrow or enter the bloodstream before they reach full maturity, which has been characterized as an ineffective erythropoiesis [1,3]. Also a certain influence has thrombocytic dysfunction, causing bleeding, the effect of uremic toxins on red blood cells, reducing iron levels due to inadequate absorption in the intestine and hemodialysis blood loss and removal of folic acid during hemodialysis [7]. Normally, the secretion of erythropoietin and erythropoiesis are in a balanced state that maintains equality between production and death of red blood cells [8]. In the development of anemia as a complication of CGN, drugs inhibiting degradation of HIF (Hypoxia-inducible factor) -1α - deferoxamine, dimethyloxalylglycine, cobazole, lactoferrin can be used [9,10], capable of stabilizing the hypoxic factor of HIF-1α transcription and activating the expression of HIF-1α-dependent erythropoietin [11,12], but inhibition of HIF-lα alone might not be sufficient to solve the problem of anemia, as there are HIF-independent ways of anemic syndrome development [13,14].
Adaptive response to hypoxia, including hypobaric, is characterized by activation of RNA and protein synthesis, which is observed not only in the brain, but also in many other vital organs, including the kidneys [15,16]. The result of such activation is an increase in the mass of the lungs, their respiratory surface and the number of alveoli, hypertrophy and increase in heart function, an increase in the number of vessels in the brain, heart, skeletal muscles and coronary channel capacity, an increase in the number of red blood cells and hemoglobin content in the blood, as well as the concentration of myoglobin in skeletal muscles and myocardium [17-19]. A significant contribution during CRF in patients with anemia is made by the associated damages of cardiovascular system, which often develops in young patients and is fatal in severe cases [20,21]. Hypoxia arising against the background of anemia leads to dilatation of peripheral vessels and reduction of vascular resistance, which in its turn leads to a decrease in blood pressure (BP).
In order to maintain normal BP, the mechanisms of vasoconstriction of peripheral vessels, increasing the heart rate and stroke volume on the background of increased activity of the sympathetic nervous system are included [22]. Slowing blood flow in the kidneys activates the renin-angiotensin-aldosterone system and the release of antidiuretic hormone [23]. Thus, the combination of CGN and anemia facilitates the progress of CKD and, in this regard, correction of anemia at the earliest stage of the disease remains one of the unsolved problems in clinical nephrology in the structure of renal and cardioprotection in patients with CKD [1,21,23]. Correction of anemia should be considered as an important part of the renoprotective strategy to reduce the risk of morbidity and mortality in this category of patients both before and after the beginning of substitutive renal therapy (SRT).Erythropoietin is now widely used for correction of anemia in CKD [1,21]. However, this drug is not always available to most patients due to its high cost. In this regard, the world is constantly searching for new methods of anemia correction, which would be cheaper, on the one hand, and more effective, on the other hand.
From these points of view, it is of interest to use hypobaric hypoxic training along with erythropoietin in the treatment of renal anemia, the efficacy of which has been proven by numerous studies, which significantly reduces the budget component of the treatment of anemia with EPO (erythropoietin) beta. The risk of endogenous hypoxia worsening during hypoxic training and the possibility of damaging effect on the organs with high oxygen deficit sensitivity cannot be completely excluded. The accumulated materials in this regard are small and incomplete, but unfortunately, no systematic comparable research has been carried out so far to study the possibility of using hypobaric hypoxia in the treatment of internal diseases, including nephrogenic anemia [17-19].
Research objective: To evaluate the effectiveness anemia correction by erythropoietin and its combination with exogenous hypoxia in chronic glomerulonephritis at the pre-dialysis stage.
Materials and Methods
This clinical trial was conducted at the Mirsaid Mirrakhimov National Center of Cardiology and Therapy. The trial consisted of the following periods: screening, randomization, individual selection of the optimal dose of erythropoietin and a combination of erythropoietin with hypoxic chamber training and observation. The diagnosis of anemia in CGN patients at the pre-dialysis stage of the disease was made based on K/DOQI (Kidney Disease Outcomes Quality Initiative) criteria developed in 2006 [24].
Entry criteria
- Patients with CGN and anemia aged 15 to 45.
- No other causes for anemia, except CGN.
Exclusionary criteria
- Age of patients under 15 and over 45 years old.
- Secondary nephropathy (hypertensive, diabetic and ischemic nephropathy, systemic diseases of connective tissue, liver cirrhosis and blood diseases).
- Patients with terminal renal insufficiency (including those receiving SRT).
- Individual intolerance to erythropoietin and hypoxic training.
Patients with CGN and anemia (n=79) were randomly sampled into two groups at the next stage: Group I included 38 patients (CGN and anemia), Group II included 41 patients (CGN and anemia). Both Groups I and II used the original preparation erythropoietin [erythropoietin beta (EPO beta) trade name Recormon, Hoffmann-La Roche, Switzerland], as an antianemic treatment. Patients of Group I (n=38) received EPO ß according to the standard procedure on the background of the common inpatient therapy. EPO beta was administered subcutaneously in an initial dose of 20-50 ME/kg, thrice weekly, until the target Hb level was reached. In Group II (n=41) patients received hypobaric chamber training (HCT) combined with EPO beta in lower doses (20-50 ME/kg, once a week). In both groups, after reaching the target Hb level, an individual supportive dose of EPO ß was selected during the whole period of observation. Patients with initially reduced blood serum iron level also received iron (trivalent) preparations of 200 mg per day.
The control was conducted on the 10th and 28th days, and then every three months of the whole period of prospective observation. When the target Hb level (120 g/l and more for men, 115 g/l and more for women) was reached, the dose of EPO ß was reduced to maintenance values. After one month, patients in outpatient conditions underwent a control examination, which included: clinical examination (blood pressure, heart rate monitor, respiratory rate, thermometry), general blood and urine analysis, daily proteinuria, blood creatinine, lipid spectrum, determining the glomerular filtrate rate (GFR). The above mentioned examination was subsequently performed every 3-6-9 months during the whole period of prospective observation. By the second month of the trial 10 people had dropped out of both intervention groups for various reasons; the final analysis included only 69 patients with CGN in the pre-dialysis stage of the disease (35 and 34 people in Groups I and II respectively). Patients of Group II receiving combined therapy (EPO-beta in combination with HCT (n=34)) in hospital received EPO-beta of 20-50 ME/kg, once a week and had daily barocamera training (except weekends).
Before and after each session of hypoxic training, a clinical examination was carried out, which included heart rate monitor, blood pressure, respiratory rate, evaluation of general health and oxygen saturation of peripheral blood. The course of HCT in the conditions of multi-seat medical hypobaric chamber was conducted according to the standard technique. The duration of the course of treatment was 15 - 17 sessions (lifts). Each treatment session consisted of lifting (7-10 min), staying at "height" (70 min) and descent (7-10 min). To clarify the tolerance of hypoxia patients were lifted at a speed of 2-3 m/sec, up to 1000 m on the first day. Later on, daily height increase was 500 m up to the final height of 3,200 m. All subsequent sessions were conducted at the height of 3,200 m (526 mm Hg). The descent was at a speed of 1-3 m/sec. The sessions of exogenous hypoxic training were conducted every 1, 3 and 6 months after prospective observation and further on the red blood parameters.
Documentation of Statistical Methods
Statistical documentation was performed on a Windows 2007 personal computer in Excel spreadsheets and using the “Statistica 6.0” application package. The significance of differences between groups was estimated using the Student’s t-test (for variables with normal distribution) and the Mann-Whitney test (for variables with non-parametric distribution). Data in dynamics were compared using paired Student’s t-test and Wilcoxon’s criterion. Data are presented as ± standard deviation mean for variables with normal distribution, and the median (25% - 75%) for variables with non-parametric distribution. A value of p<0.05 was considered a statistical significance level.
Results and Discussion
Initially patients of Groups I and II did not vary significantly among themselves in age, sex, duration of the disease, hemodynamic indices (Table 1). There were no essential differences between patients of the compared groups in iron and fibrinogen content. One of the known side effects of erythropoietin in patients with anemia and CKD is its effect on the BP level, increases systemic BP. No such negative shifts from both systolic and diastolic BP have been observed in our study, as seen from Table 2. This was possibly due to adequate intake of antihypertensive drugs. Analysis of clinical and laboratory parameters dynamics under the influence of different types of therapy showed improvement of peripheral blood parameters in patients with CGN after their 12-month mono (EPO-beta) and combined therapy (EPO-beta in combination with HCT). The parameters of peripheral blood in patients on different regimens of antanemic therapy are shown in Tables 3 & 4. Thus, an increase of Hb level was observed in dynamics after 24 months in both groups: up to 124 g/l in Group I and 129.9 g/l in Group II.
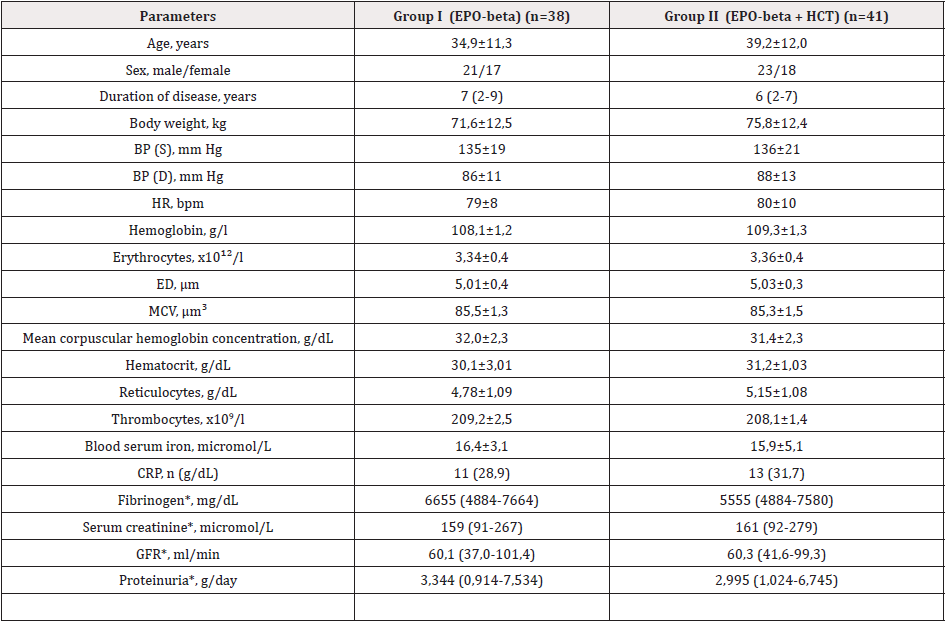
Table 1: Initial clinical and laboratory characteristics of the examined groups with chronic glomerulonephritis and anemia.
Notes: EPO – erythropoietin; GBT – hypoxic chamber training; BP – blood pressure; S – systolic; D – diastolic; HR – heart rate; ED – erythrocyte diameter; MCV – erythrocyte mean volume; ‰ - ppm; CRP – C reactive protein; GFR – glomerular filtrate rate; * - median presented data (25%-75%)
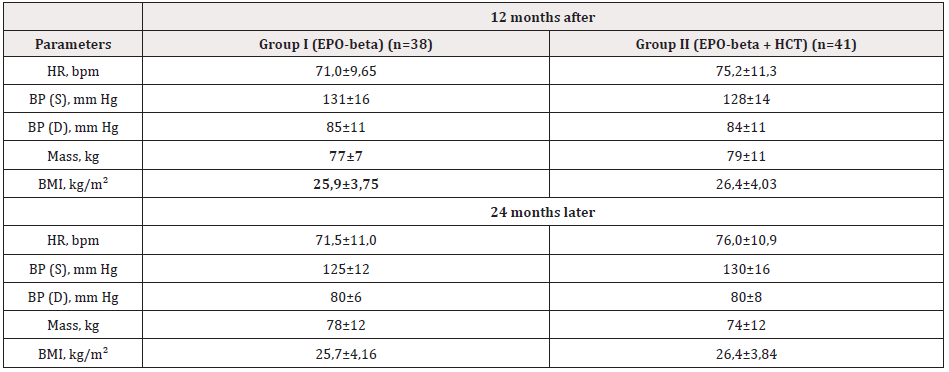
Table 2: Dynamics of clinical parameters in CGN patients under the influence of erythropoietin-beta
(Gr. I) and its combination with exogenous hypoxia (Gr. II). Notes: HR – heart rate; BP – blood pressure; S – systolic; D – diastolic; BMI - body mass index.
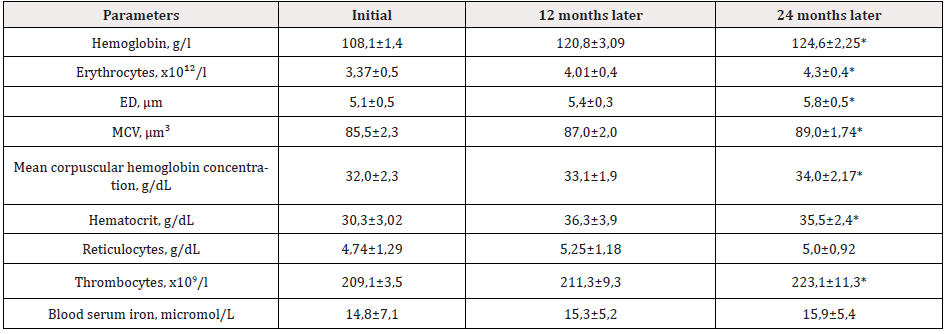
Table 3: Parameters of peripheral blood in CGN patients treated with EPO-beta (Group I).
Notes: EPO – erythropoietin; ED – erythrocyte diameter; MCV – erythrocyte mean volume; ‰ - ppm; (*) p<0,05 – compared to initial data.
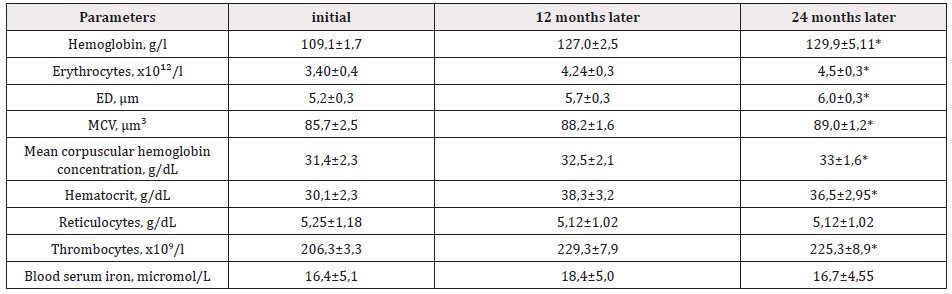
Table 4: Influence of combined therapy of EPO ß + HCT (Group II) on peripheral blood parameters in CGN patients.
Notes: ED – erythrocyte diameter; MCV – erythrocyte mean volume; ‰ - ppm; (*) p<0,05 – compared to initial data.
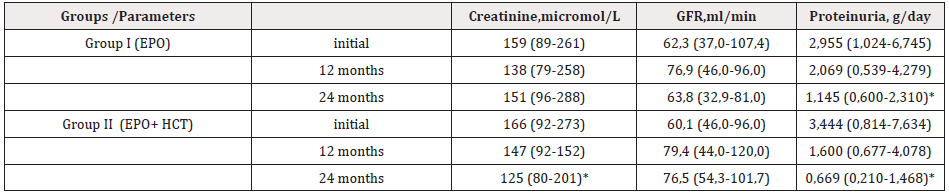
Table 5: Dynamics of laboratory parameters under the influence of mono and combined therapy of anemia in CGN patients.
Notes: EPO – erythropoietin; HCT - hypoxic barochamber training; GFR – glomerular filtrate rate; (*) p<0,05 – compared to initial data.
In addition, a noticeable increase in the number of thrombocytes, erythrocytes and their indices was observed in both groups in the dynamics of the prospective study. The main mechanism of the adaptation effect of all types of hypoxic training is due to the activation of stress-limiting systems of urgent adaptation and the formation of a structural trace of long-term adaptation focused on compensating for oxygen deficiency in inhaled air. At the same time, body functions are stimulated, including erythropoiesis [17-19]. It is known that EPO level increases in response to exogenous hypoxia [1,17,18]. It was found that in progressive kidney diseases EPO products in response to exogenous hypoxia can be preserved at the GFR level of more than 30-40 ml/min/1.73 m² [25,26]. Through b2-adrenor receptors, EPO-synthesizing kidney cells and the system of secondary intermediaries in them (cAMP and cGMP), adrenaline and noradrenaline cause increased synthesis and secretion of EPO in blood [17,18,27,28].
It has been suggested that even short-term hypoxic stimulation may increase the production of EPO with life-span of 30 min [25,29]. Differences between groups in our studies were also noted in achieving the target Hb value. Thus, the target Hb concentration achievement was established in 29 (82, 8%) patients who received EPO-beta, whereas the target hemoglobin level was reached in 32 (94, 1%) patients in Group II. No complications were observed in using both types/regimens of therapy. The data of Table 5 show that the degree of proteinuria in the individuals of Group I significantly decreased in the dynamics (24 months) [1.145 (0.600-2.310) g against 2.955 (1.024-6.745) g; p<0.05]. At the same time, there was only a tendency to increase the GFR: 63.8 (32.9-81.0) ml/min vs. 58.0 (30.6-110.4) ml/min. The group of patients who received exogenous hypoxia in combination with EPO-beta also registered a significant decrease in the value of daily proteinuria [0.669 (0.210-1.468) g vs.3.444 (0.814-7.634) g; p<0.05].By the end of the prospective study (24 months later), a comparative analysis between the groups showed that a more effective reduction in the degree of daily proteinuria was observed in the group of patients receiving exogenous hypoxia + EPO-beta compared to the group receiving only EPO-beta [0.669 (0.210-1.468) g vs. 1.145 (0.600-2.310) g; p<0.05 (0.210-1.468].
The adaptation effect in hypobaric hypoxia will be more pronounced than in normobaric. Less dense, thin air at height will have less resistance to breathing and functioning of the circulatory system closely related to the respiratory movements. Therefore, compensatory reactions of the cardiorespiratory system in high-altitude hypoxia will be more effective and economical than in normobaric hypoxia, which should be taken into account, above all, in the treatment of patients with bronchopulmonary and cardiovascular diseases [17,18]. During the time of observation there were significant shifts in fibrinogen parameters in the group of EPO-beta in combination with hypoxic training. It is noteworthy that after 12 months of treatment with HCT in combination with EPO-beta, the patients' blood fibrinogen content decreased (p<0, 05), while in Group I the decrease of fibrinogen concentration did not reach statistical significance. Reducing oxygen stress in the blood stimulates the synthesis of erythropoietin in the kidneys.
Erythropoietin in turn activates the red shoot function in the bone marrow, resulting in an increased number of red blood cells [30,31]. Thus, patients who received EPO-beta combined therapy (EPO-beta in combination with HCT), which significantly reduced the budget component of anemia treatment, had reliable changes in peripheral blood parameters with increased concentration of hemoglobin, hematocrit, erythrocyte and thrombocyte, which makes it advisable to use hypobaric hypoxic training as one of the components of the Renoprotective strategy in CGN patients at the pre-dialysis stage of the disease.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The study had no sponsorship.
References
- Moiseev V S, Mukhin N A (2014) cardiovascular risk and chronic kidney disease: cardio-nephroprotection strategies. Clinical Nephrology 2: 4-29.
- Madu A J, Ughasoro M D (2017) Anaemia of Chronic Disease: An In-Depth Review. Med Princ Pract 26(1): 1-9.
- McClellan W, Aronoff S L, Bolton W K (2004) The prevalence of anemia in patients with chronic kidney disease. Curr Med Res Opin 20 (9): 1501-1510.
- Fishbane S, Block G A, Loram L (2017) Effects of ferric citrate in patients with nondialysis-dependent CKD and iron deficiency anemia. Journal of the American Society of Nephrology 28(6): 1851-1858.
- Becherucci F, Roperto R M, Materassi M, Romagnani P (2016) Chronic kidney disease in children. Clinical Kidney Journal 9(4): 583-591.
- Özdemir N (2015) Iron deficiency anemia from diagnosis to treatment in children. Turkish Archives of Pediatrics Türk Pediatri Arşivi 50(1): 11-19.
- Novikov V E, Levchenkova O S (2013) Hypoxia induced factor as a target of pharmacological action. Reviews of clinical pharmacology and drug therapy 11(2): 8-16.
- A I Vorobyov (1985) Manual on hematology/Ed. Medicine 2.M.
- Levchenkova O S, Novikov V E (2014) Inductors of the regulatory factor of adaptation to hypoxia. Russian Medical and Biological Herald academician I P Pavlova 32: 134-144.
- Levchenkova O S, Novikov V E, Pozhilova E V (2012) Pharmacodynamics and clinical use of antihypoxants. Reviews of clinical pharmacology and drug therapy 10(3): 3-12.
- Ivanova L N, Lavrinenko V A, Babina A B (2008) Structure and concentrating ability of the kidneys of the Brattleboro rats under conditions of prolonged vasopressin injection. Bulletin of Experimental Biology and Medicine 11: 580-584.
- Fedoseeva L A, Dymshits G M, Markel A L (2009) Characteristics of the renin system of the kidney in rats of the NISAG line with stress sensitive arterial hypertension. Bulletin of Experimental Biology and Medicine 2: 134-138.
- Fiocchi E H, Cowgill L D, Brown D C (2017) The Use of Darbepoetin to Stimulate Erythropoiesis in the Treatment of Anemia of Chronic Kidney Disease in Dogs. J Vet Intern Med 31(2): 476-485.
- Faivre A, Scholz C C, de Seigneux S (2020) Hypoxia in chronic kidney disease: towards a paradigm shift? Nephrology Dialysis Transplantation.
- Yupatov G I, Dotsenko E A, Yupatov Y G (2013) Application technologies of hypobaroadaptation in the clinic of internal diseases. Literature Review 9-10.
- Tsuruya K, Yoshida H, Suehiro T (2016) Erythropoiesis-stimulating agent slows the progression of chronic kidney disease: a possibility of a direct action of erythropoietin. Renal failure 38(3): 390-396.
- Meyerson F Z (1973) Overall adjustment mechanism and prevention. M: Medicine
- Mirrakhimov M M (1977) Treatment of internal diseases mountain climate. M: Medicine
- Ushakov I B, Chernyakov I N, Shishov A A (1977) A method for increasing human resistance to the flight stressors. Patent for invention M.
- Bartnicki P, Stępień M, Rysz J (2017) Methoxy polyethylene glycol-epoetin beta as a novel erythropoiesis stimulating agent with possible nephroprotective and cardiovascular protective effects in non-dialysis chronic kidney disease patients. Curr Pharm Biotechnol 18(4): 303-308.
- Locatelli F, Fishbane S, Block G A, Macdougall I C (2017) Targeting Hypoxia-Inducible Factors for the Treatment of Anemia in Chronic Kidney Disease Patients. American Journal of Nephrology 45(3): 187-199.
- Hattori M (2017) Hemoglobin target in children with chronic kidney disease: valuable new information. Kidney International 91(1): 16-18.
- Lullo L Di, Bellasib A, Barberaa V (2017) Pathophysiology of the cardio-renal syndromes types 1-5: An uptodate. Indian Heart Journal 69(2): 255-265.
- (2006) National Kidney Foundation. K/DOQI clinical practice guidelines and clinical practice recommendations for anemia in chronic kidney disease. Am J Kidney Dis 47(Suppl 3): S1-S146.
- Fishbane S, Schiller B, Locatelli F (2013) Peginesatide in Patients with Anemia Undergoing Hemodialysis. N Engl J Med 368(4): 307-319.
- Mark J, Koury Volker, Haase H (2015) Аnaemia in kidney disease: harnessing hypoxia responses for therapy. Nature Reviews Nephrology 11(7): 394-410.
- Trinh K V, Diep D, Chen K J Q, Huang L, Gulenko O, et al. (2020) Effect of erythropoietin on athletic performance: a systematic review and meta-analysis. BMJ Open Sport & Exercise Medicine 6(1): e000716.
- Kiriakidis S, Henze A T, Kruszynska Ziaja I (2015) Factor-inhibiting HIF-1 (FIH-1) is required for human vascular endothelial cell survival. J FASEB 29(7): 2814-2827.
- Sanchis Gomar F, Martinez Bello V E, Domenech E (2009) Effect of intermittent Hypoxia on hematological parameters after recombinant human erythropoietin administration. Eur J Physiol 107(4): 429-436.
- Semenza G L (2009) Regulation of oxygen homeostasis by hypoxia-inducible factor 1. Physiology (Bethesda) 24: 97-106.
- Murkamilov I T (2014) Hypoxic pressure chamber training in the treatment of anemia in chronic glomerulonephritis. Izvestiya universities of Kyrgyzstan. Publishing house science and new technologies, Bishkek 6: 71-76.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.