Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Relationship Between the Sizes of Blood Vessel and Selected Stent
*Corresponding author: Hui Han Lin, Division of Cardiovascular Surgery, China Medical University Hospital, Taichung, Taiwan
Received: August 14, 2020; Published: September 11, 2020
DOI: 10.34297/AJBSR.2020.10.001497
Abstract
Left subclavian artery (LSA) occlusion is often treated by stent implantation. However, it may cause In-Stent Restenosis. The most comment of In-Stent Restenosis is excessive thrombus that squeezes the stent and causes vascular occlusion; hence “Drug-Eluting Stent” and “Assurance” are produced. Besides, the selected stent size is an important factor for preventing from In-Stent Restenosis. There are no data regarding the blood vessel cross-section area versus subclavian In-Stent Restenosis. This research is to investigate the relationship between the cross-section diameter of blood vessel and the size of the selected stent after stenting for In-Stent Restenosis based on previous medical records. A doctor then can select which stent is more suitable for a patient.
Introduction
According to the statistics of report “Ten Major Causes of the Death Rank” by the Ministry of Health and Welfare (Taiwan) in 2018, heart disease and cerebrovascular disease are ranked the second and the fourth in Taiwan, which illustrates that cardiovascular disease has seriously endangered people’s health.
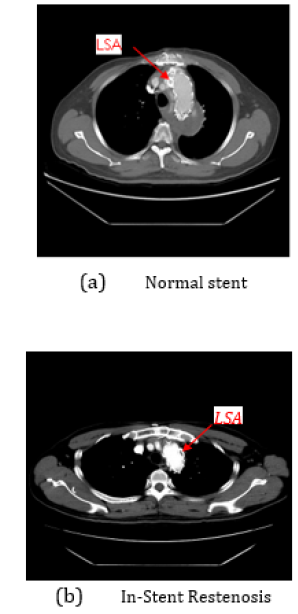
The convex side of the aortic arch has three large arteries, from right to left, the head wall artery (Brachiocephalic trunk), the common carotid artery, and the subclavian artery. The subclavian artery is the channel transporting blood to head and arm. Subclavian artery stenosis may lead in upper-extremity claudication and fatigue; it may even result in angina pectoris because of coronary artery steal with retrograde blood flow occurring after upper-extremity exercise. Frequent symptoms of subclavian artery stenosis are bruits over the subclavian artery, blood pressure decrease, and intermittent claudication of the arm ipsilateral to the affected subclavian artery. The left subclavian artery is more frequently obstructed than the right subclavian artery [1]. Figure 1 demonstrates a normal stent image and an In-Stent Restenosis image.
Vascular stent is a special cylindrical metal net. A balloon catheter with the metal stent is placed to a narrow vascular. The balloon is inflated to expand the stent, and then the stent is stayed in the vascular to improve the blood flow. However, the vascular wall is stimulated by the stent, so that platelets may be generated and become thrombus. The patient with severe occlusion of left subclavian artery, heart stent surgery is a common treatment; however, there is still 5% to 25 chance to occur In-Stent Restenosis after surgery (Figure 1) [2]. Excessive thrombus is the most common cause of In-Stent Restenosis. Although Drug-Eluting Stent can reduce this chance, they still cannot completely avoid In-Stent Restenosis [3].
Stent is an expandable device which is inserted into artery via angioplasty techniques to keep a blood vessel open. Different stents have the most appropriate expansion size. If the stent expands too much, it may happen some problems like stent deformation or vessel fracture, and the stent will lose its support [4]. There are no data regarding the cross-section diameter of stent versus subclavian In-Stent Restenosis. This research is hence to scrutinize the relationship between the cross-section diameter of blood vessel and the size of the selected stent based on previous medical records concerning In-Stent Restenosis.
Experimental Results
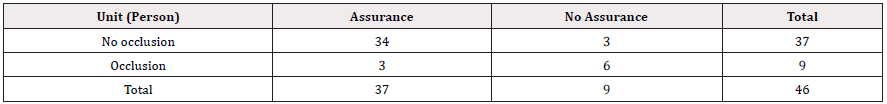
In this research, a data set from 46 patients, provided by China Medical University Hospital, Taichung, Taiwan, is used as the testing samples. In the 46 patients, 37 patients had no In-stent restenosis after surgery and 9 patients had In-stent restenosis. Out of the 46 patients, 37 patients were installed with Assurance, and 9 patients were not installed with Assurance. The 9 patients with Assurance and the 9 patients with the occlusion did not completely overlap, as shown in [Table 1].
Among the 46 patients, only three of nine stenting patients with assurance had In- stent restenosis, and other six of them did not have In-stent restenosis. Statistic results show that 66% of the patients with In-stent restenosis did not be treated by stenting with assurance, and 98% of patients without In-stent restenosis treated by stenting with assurance. One can obviously observe that the use of assurance has a high probability without In-stent restenosis.
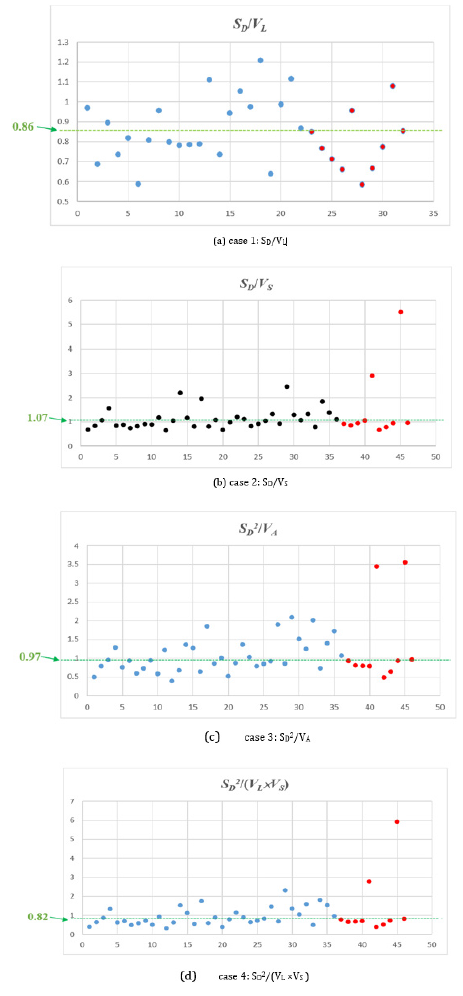
Let SD be the a cross-section diameter of the stent used in the stenting surgery for a patient, VL the distance between two farthest pixels P1 and P2 on the contour of the left subclavian artery before stenting surgery, and VS the distance of two pixels P΄ and P΄ which are located on the contour of the subclavian artery. In addition, the line L΄ connecting P΄ and P΄ passing through the central point of P1 and P2; and L΄ is perpendicular to the line connecting P1 and P2. Also let VA the area of the cross-section area of the subclavian artery. This research is to investigate the relationships between In-Stent Restenosis and four cases C1=SD/VL, C2=SD/VS, C3=S2/VA, C4=S2/(VL×VS). [Figure 2] illustrates the four cases. In Fig.2, the blue points represent non-occlusion patients and the red points represent the occlusion patients.
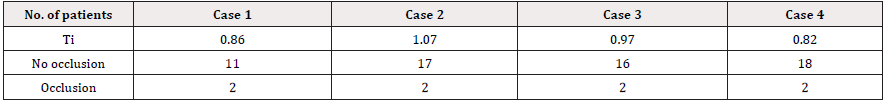
In this research, a threshold Ti is given for case i. It means that given Ci>Ti can reduce the occurrence of In-Stent Restenosis. Table 2 demonstrates the number of patients occurring In-Stent Restenosis in four cases with different Ti. [Table 2] obviously shows that case 4 with Ti=0.82 can offer the most satisfying effect. Since the vessels of patients 41 and 45 are fracture, there is a big chance to occur In-Stent Restenosis after surgery for both patients.
Conclusions
This research is to analyze the type and the size of the stent used in stenting implantation. It is helpful for the healthcare professional to select the fittest stent so that the incidence of In-Stent Restenosis can be reduced after vascular stent surgery. The results obtained by analyzing previous medical records illustrate that When given C4>0.82, a lower incidence of In-Stent Restenosis will be obtained. Moreover, this research also explored the other case assurance stent. Assurance is also a bare metal stent that helps maintain the original stent support on the vascular wall.
References
- Felipe Fregni, Luiz Eduardo Coutinho Castelo Branco, Adriana Bastos Conforto, Fabio Iuji Yamamoto, Cynthia Resende Campos, et al. (2003) Treatment of Subclavian Steal Syndrome with Percutaneous Transluminal Angioplasty and Stenting. Arq Neuro Psiquiatr 61(1): 95-99.
- Yingkun He, Tianxiao Li, Weixing Bai, Liangfu Zhu, Meiyun Wang, et al. (2019) Cerebrovascular Drug-Eluting Stent versus Bare-Metal Stent in the Treatment of Vertebral Artery Stenosis: A Non- Inferiority Randomized Clinical J Stroke 21(1): 101-104.
- Evan Shlofmitz, Micaela Iantorno, Ron Waksman (2019) Restenosis of Drug-Eluting Stents: A New Classification System Based on Disease Mechanism to Guide Treatment and State-of-the-Art Circ Cardiovasc Interv 12(8): e007023.
- P D Williams, M Awan (2017) Stent selection for percutaneous coronary intervention. Continuing Cardiology Education 3(2): 64-69.
- Irving S Wright and Donald Cameron (1965) The Subclavian Steal and Other Shoulder Girdle Syndromes. Trans Am Clin Climatol Assoc 76: 13-25.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.