Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Vitamin D 3 Supplementation and Parameters of Metabolic Syndrome
*Corresponding author: N Sobhi, Diabetology Service, Biochemistry Service, Central Hospital Alger, Algeria.
Received: October 05, 2020; Published: October 30, 2020
DOI: 10.34297/AJBSR.2020.10.001555
Abstract
Introduction: One of the most prolific fields of research of the last twenty years, including work on diabetes, is that of the relationship of this pathology with the nutritional status of the patient.
Materials and Methods: An experimental therapeutic test over a period of 24 weeks was carried out in 42 type 2 diabetic patients aged 40 to 80 years, randomly divided into two groups: a group on vitamin D3 and a control group without treatment. The aim of this work is to determine the effect of vitamin D3 supplementation on the insulin sensitivity index; HOMA IR, HBA1C, systolic blood pressure, diastolic and lipid profile (HDL, LDL, TG, and cholesterol).
Results: After 24 weeks of follow-up, the therapeutic test with vitamin D 3 allowed a significant increase in plasma 25 (OH) D in the group under treatment (P=0.002), while the variations in the control group are not significant, which confirms the effectiveness of the therapeutic intervention and the attendance of the patients in the study; Correction of 25 (OH) D deficiency was not associated with a statistically significant improvement in insulin sensitivity index; HOMA IR, HBA1C, systolic blood pressure, diastolic and lipid profile (HDL, LDL, TG, and cholesterol) which remain unchanged in both groups of treated and untreated patients.
Conclusion: Hypovitaminosis D is very common in the population of type 2 diabetic; conflicting results have been reported on the beneficial role of vitamin D on the parameters of metabolic syndrome and glycemic control. More vitamin D intervention trials are needed to provide conclusive evidence on the role of vitamin D in carbohydrate homeostasis.
Keywords: Hypovitaminosis D, Type 2 Diabetes, Arterial Hypertension, Hba1c, Dyslipedemia
Introduction
The importance of good nutrition is not a new idea ... Already 400 years before JC Hippocrates said that “food was our first medicine”. According to ancient Chinese medicine, food is also a remedy for which it is important to follow very specific instructions to prevent and even treat diseases [1]. Since then, research on the links between diet and health has made progress. A link between nutritional deficiencies and disease has been shown; such as blindness due to vitamin A deficiency, cretinism due to iodine deficiency. Recently, a new parameter, that of vitamin D, has been added to the environmental factors traditionally involved in the progression of metabolic and cardiovascular pathologies [1-3]. Vitamin D continues to gain the attention of health professionals; it occupies an important place in research themes, as evidenced by the impressive number of publications on the subject. In this context, a link between vitamin D and type 2 diabetes has been suggested. This relationship was elucidated in 1967, when Milner and Hales showed that in animals, calcium and magnesium [strictly regulated by the vitamin D system] are essential for the secretion of insulin. This vitamin could therefore interact with the various physiopathological mechanisms governing insulin secretion, insulin resistance and the parameters of carbohydrate homeostasis [4,5].
Material and Methods
An experimental therapeutic test over a period of 24 weeks was carried out in 42 type 2 diabetic patients aged 40 to 80 years, randomly divided into two groups: Group 1, receiving treatment with vitamin D3, one ampoule of 200,000IU per month for 3 months, then maintenance treatment at the rate of one ampoule of vitamin D3 at 200,000IU on the 5th month. The goal is to achieve a serum level of 75 nmol / L [30 ng / ml] of 25 OHD. Group 2, the control group, received no treatment. The patients were replaced at the end of our study.
The aim is to determine the long-term effect of vitamin D 3 supplementation on the following parameters:
- HBA1C and HOMA IR Index;
- The components of metabolic syndrome, lipid profile [HDL, LDL, TG and CHOL]; BMI, blood pressure;
- Evaluation of the effectiveness of the therapeutic protocol, as well as its possible drawbacks and / or adverse effects.
- Patients have been advised to report all side effects of vitamin D treatment:
- Nausea, vomiting, abdominal pain;
- Urinary problems, nephritic colic;
- Muscle cramps;
- Hypercalcemia [> 2.50 mmol / l];
Patients are subjected to the therapeutic test, after having ruled out the presence of a contraindication to replacement therapy with vitamin D 3.
The rare contraindications for treatment with vitamin D are:
- Hypercalcemia [> 2.5 mmol / L], calcium urolithiasis;
- Known hypersensitivity to vitamin D [exceptional];
Patients were instructed not to change the type or dosage of their medications throughout the study. The follow-up is done on an outpatient basis, comprising a double clinical and biological evaluation in the two groups at inclusion and at the 6th month.
The inclusion criteria are:
Type 2 Diabetic Patients, aged 40 to 80 years with:
- Glycated hemoglobin [HbA1c] greater than 7%;
- Insulin resistance [HOMA-IR ≥ 2];
- Vitamin D deficiency [25 [OH] D <20 ng / ml].
The exclusion Criteria are: Patients taking insulin, lipid-lowering therapy and treatment for high blood pressure (Figure 1).
Results
The basic characteristics of the subjects who participated in the study are comparable between the two groups of patients (no significant difference). It was noted that after 24 weeks in both groups with and without vitamin D treatment:
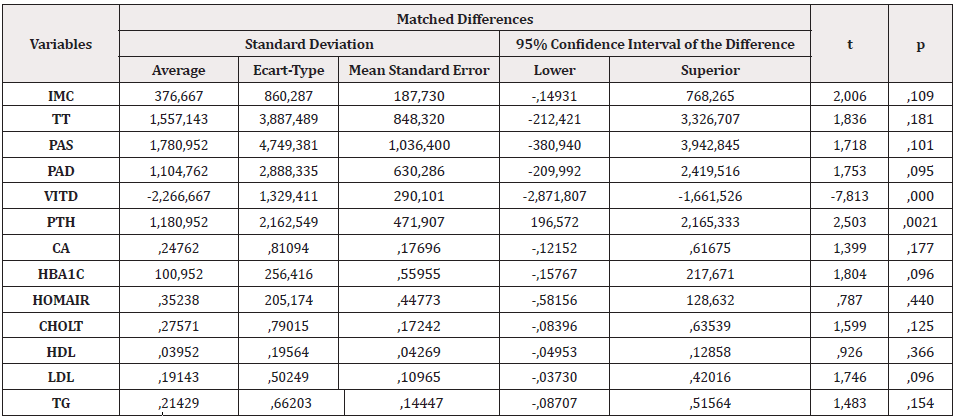
a) Plasma 25 (OH) D increased significantly in the vitamin D group with an average of 32.81ng/ml after 24 weeks of treatment (P=0.002), while the variations in the control group were not not significant, which confirms the efficacy of the therapeutic intervention and the attendance of patients in the study;
b) No statistically significant change in the treatment group for systolic and diastolic blood pressure and lipid profile (HDL, LDL, TG, and cholesterol).
c) No statistically significant changes between the two groups, for the insulin sensitivity index; HOMA IR and IMC.
Discussion
Glycemic Balance
Vitamin D3 treatment did not cause a significant change in HbA1c or insulin sensitivity index; HOMA IR. Indeed, our results agree with those reported in the literature in two meta-analyzes by Pittas et al. [6,7] which reported 8 observational cohort studies and 11 randomized controlled trials, they found no effect on carbohydrate metabolism. Pittas AG, in 2010, of the six intervention trials reviewed (five with vitamin D alone and one with calcium and vitamin D), none produced a remarkable change in carbohydrate metabolism in type 2 diabetics [8,9]. In George PS's meta- analysis [10], published in 2012, there was insufficient evidence to support a beneficial role of vitamin D on hyperglycemia or insulin resistance. Von Hurst et al. [11] showed no improvement in insulin sensitivity after six months of cholecalciferol supplementation. Conflicting results have been reported in an Iranian randomized clinical trial on 90 people with diabetes who took twice a day for three months a drink fortified or not with vitamin D3. A drop in blood sugar, HBA1C, with a significant decrease in their body mass index and their fat mass were noted in the group taking vitamin D [12].
Nikooyeh B [13], in his study concluded that vitamin D can help restore blood sugar balance over 12 weeks. 90 diabetic patients randomly divided into 3 groups, in the first group, they consumed a natural drink; in the second group, a drink enriched with 500 IU of vitamin D and 150 mg of calcium, and in the third group, a drink containing 500 IU of vitamin D and 250 mg of calcium. In the two groups supplemented with 25 ug per day of vitamin D, the fasting blood glucose values fell after 3 months on average by 13%, the glycated hemoglobin by 0.4%, the waist circumference by approximately 4% and the body fat index by 1%, while vitamin D increased by 32%. It was concluded that the daily intake of vitamin D at 25ug per day with or without added calcium, improves blood sugar balance in patients with type 2 diabetes. Recently, in a meta-analysis published in 2015 [14], on studies with more than 3 months of follow-up, a non-significant improvement in HbA1c was observed [15-18]. These studies show that the information pooled in the intervention trials of vitamin D, has not provided conclusive evidence on the role of vitamin D in carbohydrate homeostasis. All studies reported a change in baseline 25OHD level, amount of vitamin D, type of vitamin D, duration of supplementation, number of patients, characteristics of subjects, overweight and drug resistance. insulin from patients.
The Lipid Profile
The results of our study did not find any modification in the lipid profile of type 2 diabetic patients after oral supplementation with vitamin D 3 for 6 months. Although there is no consensus between interventional studies of the effects of 25 (OH) D3 on the lipid profile, it has been suggested that vitamin D may alter the lipid profile through direct and indirect effects. Wang, in 2009, found that vitamin D can lower plasma triglycerides by increasing the activity of lipoprotein lipase in obese people [19-21], in in vitro studies showed that PTH reduced lipolysis by increasing the level of cytosolic calcium and the expression of fatty acid synthesis. Calcium influences lipid levels by interfering with fatty acid absorption through the formation of insoluble fatty calcium complexes in the intestine. This results in an increased conversion of cholesterol to bile acids [22]. But the association of 25 (OH) D3 with cardiometabolic parameters in these studies appears to be influenced by other factors such as duration of diabetes, patient weight and glycemic control.
Treatment with vitamin D and Blood Pressure
In our study, oral vitamin D3 supplementation for 6 months did not influence the systolic and diastolic blood pressure of type 2 diabetics. The relationship between vitamin D status and blood pressure is poorly established due to conflicting epidemiological data. Krause R et al. [23], in an intervention study published in 1998, shows that exposure to UVB, versus UVA, three times a week for six weeks, in people with moderate arterial hypertension not treated, allows a decrease in systolic and diastolic arterial pressures of 6mm Hg. In the group subjected to UVB, 25 (OH) D went from 23 ng / ml to 60 ng / ml, whereas in the group subjected to UVA, it has not evolved. Pfeifer M et al. [24], in 2001 it was observed in a group supplemented with 800 IU of vitamin D and 1200 mg of calcium per day, while another group received 1200 mg of calcium per day, for 8 weeks, a decrease systolic blood pressure of 5 mm Hg in 81% of subjects in the first group, against 47% of the second group [25-27] found in type 2 diabetic patients with vitamin deficiency D, divided into two groups, one group on a single 100,000 IU dose of vitamin D2 and the other group on placebo, the supplemented group saw its systolic blood pressure decrease by 7.3 mm Hg vs 6.6mm Hg in the placebo group. According to Witham MD in type 2 diabetics, high doses of vitamin D improve systolic blood pressure and lower the level of type B natriuretic peptide, with no effect on DBP. The beneficial effect of vitamin D on arterial pressure could only be observed in subjects initially deficient, which explains why some larger intervention studies [28-29] in subjects with little or no deficiency, supplemented do not find significant variation. Additional studies are essential to better define the relationship between vitamin D and hypertension, an essential condition for recommending systematic supplementation in hypertensive patients. Regulation by vitamin D of the expression of renin would be independent of its action on calcium metabolism. However, work by Pfeiffer [25] in older women shows that supplementation with calcium and vitamin D at the same time reduces systolic blood pressure and PTH levels in the short term. Studies carried out in a Scandinavian community have revealed that the level of PTH was predictive of long-term cardiovascular mortality [30,31].
Treatment of Hypovitaminosis D
The patients included in our work significantly increased their vitamin D level, after treatment at a rate of 200,000 IU per month for three months and one ampoule of vitamin D at 200,000 IU on the 5th month. The mean rate at inclusion was 10.14ng/ml and it increased to 32.81 ng / ml at the 6th month (P= 0.002), while the variations in the control group were not significant (P=0.612). This confirms the efficacy of the treatment and the attendance of the patients in our study (Table 1). The significant increase, but lower than expected in 25 (OH) D, despite our intensified treatment regimen, may be due to the storage of vitamin D by adipose tissue, knowing that our patients are overweight of the android type. Souberbielle et al. [29] recommend the use of a loading dose, in order to quickly increase the level of vitamin D which varies according to the initial level. [32]
According to Holick et al. [4,29] a dose of 100,000 units every 2 to 3 months would be sufficient to maintain at 30ng/ml. J Aloia et al. [30] specified that to reach 32 ng ml, with a level below 20ng/ml, a daily dose of 4000 IU is needed and to stay around 80 nmol/ l it takes 2000 IU / d. R Vieth et al. [32] should rather receive 2000 IU / D and joins the Italian authors and RP Haeney [33] who recommend doses varying between 800 to 2000 IU / D (157). Heaney et al. [33] also have demonstrated the benefit of high-dose supplementation in 67 patients receiving 0, 25, 125 or 250μg / d (0, 1000, 5000 or 10,000 IU / d) for 20 weeks during the winter. The majority of this consumption comes from reserves produced by skin synthesis during the summer. They then justify the benefit of increasing vitamin D intake in patients with reduced skin synthesis. In October 2011, the "Endocrine Society Clinical Practice Guideline" published a summary of the different situations; according to the risk factors of people aged between 18 and 50 years, the authors recommend doses of up to 6000 IU / D for 8 weeks to correct severe deficits and doses of 600 IU / D to 2000 IU / D to maintain the serum level of vitamin D around 75nmol/ l. According to S Cangoz [34] vitamin D supplementation in type 2 diabetic patients, with risk factors for hypovitaminosis D, should be done with an initial loading dose and a regular maintenance dose of vitamin D (Table 2).
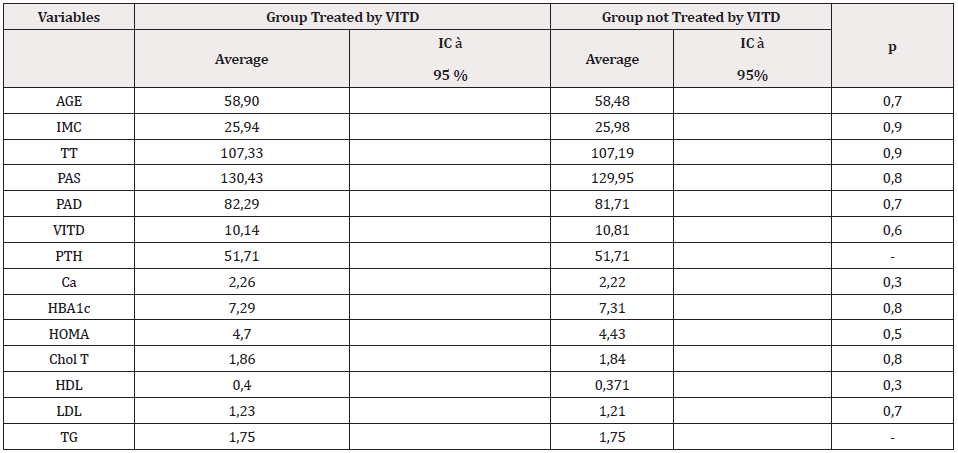
Table 1: The basic characteristics of the subjects who participated in the study.
Note: comparison of the two groups at time 0
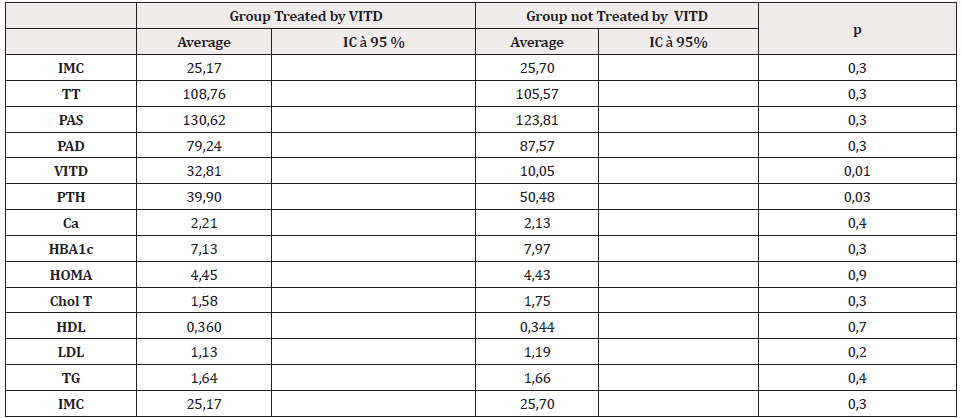
Table 2: Comparison and changes after 24 weeks in the two groups.
Note: comparison of the two groups at Time 6.
Overdose, Toxicity and Side Effects of Vitamin D Treatment
In our study, vitamin D3 supplementation did not cause side effects related to hypercalcemia. None of the patients had biochemical hypercalcemia (> 2.50 mmol/L), no nausea, vomiting, abdominal pain, or urinary tract problems. In our study, the average level of vitamin D after treatment was 32.82 ng / ml, clearly below the value considered as the upper limit, i.e. 150 ng / ml, despite the 800,000 IU distributed over 6 months. According to Jones G [35], studies in animals and humans have indicated that the threshold for symptoms of toxicity is around 300ng /ml. Hypercalcemia would only appear at regular vitamin D concentrations between 150 and 200 ng / ml. No serum overdose was found in a study conducted by Pepper KJ [36] in Georgia. 48 patients received 450,000 IU over 5 months, 80 patients had 300,000 IU over 6 months and 27 received 900,000 IU over 6 weeks. For Vieth R et al. [37-38] an intake above 1250μg / d, i.e. 50,000 IU / d, corresponds to a toxic dose (NOAEL = No Observed Adverse Effect Level), which makes it possible to calculate the upper limit of the tolerable dose (Tolerable Upper Intake Level or UL) at 250μg / d or 10,000 IU / d. While in the study by Tucci JR [39] the risk of overdose is almost zero, since it would take 10,000 IU daily to see side effects. Vieth's [40] study also clarified that to bring up a low level of 25 (OH) D, the dose of 100μg / d (ie 4000IU / d) was without danger of toxicity. Holick [4] has shown that the rare cases of hypervitaminosis D are due to accidental ingestion and following an interaction with drugs such as a thiazide on unfavorable ground such as renal failure.
Conclusion
One of the most prolific fields of research of the last twenty years, including work on diabetes, is that of the relationship of this pathology with the nutritional status of the patient (Table 3). Our study is the first in this field in Algeria, structured on the evaluation of an experimental therapeutic protocol [41-44]. The therapeutic test with vitamin D 3 allowed: A significant increase in plasma 25 (OH) D in the treated group, to an average of 32.81 ng/ ml and we did not report any side effects. This confirms the efficacy and safety of vitamin D. The toxic dose is far from current recommendations. A statistically significant decrease in PTH in the group receiving vitamin D3 treatment. Conversely, our study did not identify a correlation between: Hypovitaminosis D and cardiovascular risk factors [45-46]. The HOMA-IR index and the HbA1c, which remain unchanged, which could be explained by the short duration of the treatment or by the initial HbA1c level not very high (less than 8%). Additional studies are essential to better define the relationship between vitamin D, diabetes, hypertension and dyslipidemia, an essential condition to recommend systematic supplementation in diabetic patients.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.