Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Mini review on Malignant Transformation of Benign Parotid Gland Tumors
*Corresponding author: El Bouhmadi Khadija, Otorhinolaryngology and Head and Neck surgery department, 20 August 1953 Hospital, Morocco.
Received: December 13, 2020; Published: December 18, 2020
DOI: 10.34297/AJBSR.2020.11.001633
Summary
The majority of parotid gland tumors is benign with a vast histologic diversity. But, malignant transformation, even though rare, can occur for almost each histological type. Multiple predictive factors are determined as well as the histologic findings corresponding to the transformation. Through this mini review, we expose the malignant potential of each histological type of benign parotid gland tumors, describing the incidence and the forms of the transformation.
The main aim to this mini review is to highlight the importance of always considering the malignant potential of benign parotid tumors in order to provide the best care and the least number of interventions to our patients.
Keywords:Benign; Malignant transformation; Parotid gland; Tumours
Introduction
The majority of parotid gland tumors is benign (80%) with a vast histologic diversity. The treatment often consists of a total excision of the lesion through partial parotidectomy. But even though considered benign, these tumors have a propensity for recurrence after treatment and mostly a no negligible risk of malignant transformation concerning almost all the histological types, requiring early care and close follow up.
Histologic diversity
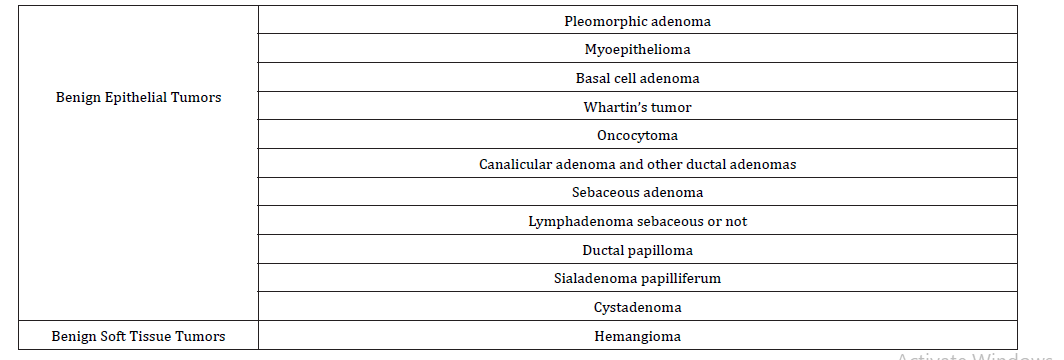
The Table 1 shows the 4th and last World Health Organization (WHO) histological classification of benign salivary gland tumors of 2017 [1].
Malignant transformation
Pleomorphic adenoma is the most common benign parotid gland tumor. It represents 70-80% of benign salivary gland tumors, affecting the parotid gland with a highest rate of 84% predominantly on its superficial lobe. The most frequently concerned age ranges are the third to sixth decades with a discrete feminine predominance [2].
There is a considerable risk for malignant transformation up to 5 -15% [3], increasing with time, more likely to arise in older patients [4] and is proportional to the duration the lesion is in situ (1.5% in the first five years, 9.5% after 15 years) [2]. The medical history of diagnosis or therapeutic radiation, the clinical large size [2] and the number of local relapses [5] are also influencing factors.
The treatment should take into account the risk of malignant change and aim to prevent it. Thus, some authors recommend adjuvant irradiation (in first intention or after recurrence) to improve local control [5] but it still controversial regarding the after all benign nature or the tumor and the risk of radio-induced cancer. Another surgical option can be suggested based on a total parotidectomy with conservation of the facial nerve [6]. If only a superficial parotidectomy is performed, the tumor capsule should be respected and the excision complete to avoid recurrence [3].
Whartin’s tumor, also known as cystadenoma lymphomatous, is the second most common benign salivary gland tumor, almost exclusively found in the parotid [3]. Initially described as benign with no risk of malignant change, multiple clinical reports proved the opposite [7]. Indeed, even though extremely rare, the malignant transformation can occur in 0,3% of the cases [8], into mucoepidermoid carcinoma, squamous cell carcinoma, oncocytic adenocarcinoma, undifferentiated carcinoma or adenocarcinoma [7,9].
The particularity of this tumor is its tendency for synchronous multiple tumors, with the most frequent combination is its association with mucoepidermoid carcinoma. Thus, to conclude at a malignant transformation of Whartin’s tumor, a synchronous bening and malignant parotid gland tumors should be eliminated [3]. Also, some elements need to be present on the histologic analysis as the transitional zones from a benign oncocytic to malignant epithelium or the infiltrating growth in the nearby lymphoid tissue [9].
All in all, Whartin’s tumor still considered as a plainly bening tumor, so, the treatment proposed in the literature can be based on a parotidectomy reducing the risk of recurrence or, more conservative, an enucleation or only a close follow-up without removal [9].
The lymphadenoma is a rare and sporadic benign tumor, mostly affecting the parotid gland (>80%), with two forms, the nonsebaceous adenoma with epithelial cell nests and often prominent lymphoid stroma and the sebaceous variant, more common, accounting for approximately two-thirds of lymphadenomas, with a partial sebaceous differentiation [3,10].
Its malignant transformation is extremely rare turning into a sebaceous carcinoma in most cases, basal cell adenocarcinoma or undifferentiated carcinoma [3,10]. But the possibility of the cancer development from sebaceous glandular remnants in a lymph node is to consider [3].
Sebaceous adenoma is a very rare tumor representing less than 0,5% of all salivary gland adenomas. Only very few cases were reported on the literature and the rare cases of occurrence of sebaceous carcinoma appeared to have arisen de novo not secondary to malignant transformation [3].
The oncocytoma represents 2% of all salivary glands tumors and is mostly located in the parotid gland. Regarding its possible multifocality, a lesion not resected in the first procedure can be later considered as a recurrence [3]. Its malignant transformation on oncocytic carcinoma is unusal and difficultly diagnosed considering its histological similarities with the benign form [11]. Even if some cases of malignant oncocytoma had been reported, the literature hardly provides substantial evidence of their arising from a preexisting oncocytoma [3,11].
The cystadenoma is a slow growing neoplasm representing 4% of benign salivary gland tumors, more frequent on the parotid. If they have no tendency to recurrence, on very rare occasions, a malignant transformation on a cystadenocarcinoma can occur [3].
Sialadenoma papilliferum affects mostly the intraoral salivary glands while its neoplastic part is the salivary ductal cells in the submucosa [3,12]. Very few cases of malignant transformation were cited on the literature, located exclusively on the oral cavity, not concerning the parotid gland [12]. Thus we may consider the parotid sialadenoma papilliferum having no proven malignant potential [3].
Two types of ductal papillomas are described, the intraductal type, mainly seen on minor salivary glands, with no tendency to recur and only one reported case of a papillary adenocarcinoma possibly arising from it [3,13]. The inverted type is more common with a recurrence and malignant change not reported yet [3].
Canalicular adenoma virtually never occurs in the major salivary glands and no malignant transformation was described [3].
On the opposite, basal cell adenoma is predominantly a tumor of major salivary glands with a rate of 75-80% in the parotid. Four types are described, the solid type, the trabecular type, the tubular type and the membranous type. The recurrence is only seen on the membranous type with a rate of 25%, while the malignant transformation can develop in all types [3]. The Nagao et al. [14] study reported a rate of malignant transformation up to 4,3% as basal cell adenocarcinoma, adenoid cytic carcinoma, duct carcinoma, adenocarcinoma not otherwise specified or intracapsular myoepithelia carcinoma. This malignant transformation seems to develop multifocally with an infiltrative growth pattern and an apparent transitional zone between benign and malignant areas. Also, it concerns older patients regarding the basis of long standing presence before malignant change.
The myoepithelioma is located on the parotid gland in 40 to 90% of the cases. The risk of recurrence is very low and still related to incomplete surgical excision. The malignant transformation is extremely rare on the reports describing a myoepithelial carcinoma, it usually appears de novo or in a recurrent pleomorphic adenoma and only very rarely from a pre-existing myoepithelioma [3].
Concerning the soft tissue tumors, the hemangioma is a benign neoplasm originated from endothelial cells including the capillary and the cavernous types [15]. It is the most common salivary gland tumor in young children, particularly in girls (<1 year) with a rate of 90% presented as unilateral compressible bluish mass rapidly enlarging after birth; while its occurrence in adults still rare and unusual [16]. The spontaneous regression is the main evolution and the possible present mitotic activity does not predict by itself any malignant behavior. The risk of its malignant transformation is related to radiotherapy and then, considered as a sequel [15].
Conclusion
Even though the majority of parotid tumors are benign, their malignant potential should always be considered specifically on long standing tumors, multiple local relapses and after radiotherapy. Thus, the treatment should be precocious with quality resection preserving the facial nerve and close follow up.
Conflict of interest
None.
References
- Seethala RR, Stenman G (2017) Update from the 4th edition of the world health organization classification of head and neck tumours: tumors of the salivary gland. Head Neck Pathol 11(1): 55-67.
- Bokhari MR, Greene J (2020) Pleomorphic Adenoma. In: Stat Pearls Ed., (2020) Treasure Island (FL): StatPearls Publishing.
- Hellquist H, Paiva-Correia A, Vander Poorten V, Miquel Q,, Juan CH, et al. (2019) Analysis of the Clinical Relevance of Histological Classification of Benign Epithelial Salivary Gland Tumours. Adv Ther 36(8): 1950-1974.
- Tarakji B, Baroudi K, Hanouneh S, Kharma MY, Nassani MZ, et al. (2013) Extensive review in the detection of the malignant transformation of pleomorphic adenoma. Gulf J Oncolog 1(13): 67-82.
- Jardel P, Fakhry N, Makeieff M, Ferrie JC, Milin S, et al. (2014) Adénomes pléomorphes parotidiens récidivants : place de la radiothérapie [Radiation therapy for pleomorphic adenoma of the parotid]. Cancer Radiother 18(1): 68-76.
- Lavorgna G, Savastano G, Rubino C (1992) La recidiva cancerizzata dell'adenoma pleomorfo della parotide. Considerazioni da un caso [The cancerous recurrence of a pleomorphic adenoma of the parotid. Comments on a case]. Minerva Stomatol 41(4): 145-50.
- Laccourreye O, Lépine C (2020) Whartin’s tumour: Not so benign! Editorial European Annals of Otorhinolaryngology, Head and Neck Diseases 137(6): 449.
- Therkildsen MH, Christensen N, Andersen LJ, Larsen S, Katholm M (1992) Malignant Warthin's tumour: a case study. Histopathology 21(2): 167-171.
- Limaiem F, Jain P. Warthin Tumor. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing.
- Kara H, Sönmez S, Bağbudar S, Güllüoğlu M, Başaran B (2020) Malignant Transformation of Parotid Gland Non-sebaceous Lymphadenoma: Case Report and Review of Literature. Head Neck Pathol 14(4): 1123-1128.
- Korbi A, Jellali S, Njima M, Harrathi K, Bouatay R, et al. (2019) Parotid Gland Oncocytoma: A Rare Case and Literature Review. Journal of Medical Cases 10(5): 146-149.
- Liu W, Gnepp DR, de Vries E, Bibawy H, Solomon M, et al. (2009) Mucoepidermoid carcinoma arising in a background of sialadenoma papilliferum: a case report. Head Neck Pathol 3(1): 59-62.
- Shiotani A, Kawaura M, Tanaka Y, Fukuda H, Kanzaki J (1994) Papillary adenocarcinoma possibly arising from an intraductal papilloma of the parotid gland. ORL J Otorhinolaryngol Relat Spec 56(2):112-115.
- Nagao T, Sugano I, Ishida Y, Matsuzaki O, Konno A, et al. (1997) Carcinoma in basal cell adenoma of the parotid gland. Pathol Res Pract 193(3): 171-178.
- Stefania D, Barbara C, Fabrizio N, Guido C, Franco B (2003) Primary angiosarcoma of the parotid gland arising from benign congenital hemangioma. Oral and maxillofacial pathology 96(1): 66-69.
- Lester DRT (2019) Hemangioma of the parotid. ENT pathology clinic.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.