Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Preclinical Evaluation of a Modified Surgical Approach to the Maxillary Sinus – Comparison of two Endoscopic Techniques
*Corresponding author: Sandra Fest, Clinic of Otolaryngology, Head and Neck Surgery, University Hospital Leipzig, Liebigstr. 10- 14, 04103 Leipzig, Germany.
Received: June 16, 2020; Published: December 08, 2020
DOI: 10.34297/AJBSR.2020.11.001609
Abstract
Purpose: There are several approaches to the maxillary sinus for the treatment of pathologies. The endoscopic technique is the gold standard in paranasal sinus surgery. The middle meatal maxillary antrostomy (MMMA), which is the enlargement of the natural opening, is the most common method. The prelacrimal recess approach (PLRA) is known as an alternative method. However, advantages of either method have not been systematically assessed.
Methods: 8 cranial models “Sinus patient Meyer” were used for the study. The maxillary sinuses were filled with a soft silicon-based paste. Each model had a CT scan prior and after endoscopic sinus surgery and volumetry of the residual maxillary sinus volume was performed. Endoscopic MMMA and endoscopic PLRA were applied. Volumetric results were compared with standard statistical evaluation using Microsoft Excel for Mac (version 15.14).
Results: 16 surgical procedures were performed. Mean volume difference between pre- and postoperative volumes of the maxillary sinus was 73.22% by using PLRA and 41.96% by using MMMA (ΔVPLRA = 73.22% vs. ΔVMMMA = 41.96 %; p < 0.0002). In all cases, prelacrimal recess approach was superior to middle meatal maxillary antrostomy.
Conclusion: Endoscopic prelacrimal recess approach is an effective method and superior to the traditional MMMA for residual-free removal of maxillary sinus tissue.
Keywords: Middle Meatal Maxillary Antrostomy; Prelacrimal Recess Approach; Volumetry; Functional Endoscopic Sinus Surgery; Maxillary Sinus
Abbreviations: MMMA: Middle meatal maxillary antrostomy; PLRA: Prelacrimal recess approach; CT: Computerized tomography; FESS: Functional endoscopic sinus surgery
Introduction
There are several surgical approaches to the maxillary sinus. In paranasal sinus surgery the endoscopic technique became the gold standard in the last decades. The endoscopic middle meatal maxillary antrostomy (MMMA) was first described by Kennedy in 1987 and has not been modified since then [1-3]. Middle meatal maxillary antrostomy is the enlargement of the natural opening of the maxillary sinus into the middle meatus.
Sometimes an additional access like endoscopic medial maxillectomy (with and without preservation of the inferior turbinate and nasolacrimal duct) or transoral surgery like Caldwell- Luc surgery is necessary to remove maxillary sinus tissue (e.g. inverted papilloma) completely [1]. In addition, external approaches like midfacial degloving or lateral rhinotomy are possible procedures [4].
It is difficult to obtain a wide and good access to the anteromedial, anterior and inferior wall of the maxillary sinus for example to resect an inverted papilloma completely [5]. The recessus prelacrimalis – the angle between the medial and anterior wall of the maxillary sinus – is hard to reach by MMMA. Inverted papillomas are benign epithelial sinonasal tumors with risk of malignant transformation (5-15%) [4,6-8]. Despite endoscopic technisques recurrence rates over 10% are reported [7]. Therefore, aggressive and complete primary surgical resection is essential [8].
The endoscopic prelacrimal recess approach (PLRA) is often discussed as an effective and safe procedure for the treatment of inverted papilloma. It preserves the inferior turbinate and the nasolacrimal duct. This surgical method gets wide and straight access to the maxillary sinus. The use of straight endoscopes and instruments results in an easier surgical management in comparison to other accesses to the maxillary sinus [10]. The aim of this study is to compare endoscopic prelacrimal recess approach with endoscopic middle meatal maxillary antrostomy within the framework of an artificial model test.
Methods
Sinus Model
For the analysis we used the artificial model “Sinus patient Meyer” (PHACON, Leipzig, Germany, Figure 1). It is a cranium model with the relevant landmarks for sinonasal surgery. Each model has two maxillary sinuses. The maxillary sinuses of the models were filled with a soft silicon-based paste. This paste is a gelatinous substance ideal to simulate pathologies like inverted papilloma, aspergilloma or chronic paranasal sinusitis.

Figure 1: Sinus patient Meyer (PHACON®), the model used in the comparison of middle meatal maxillary antrostomy (MMMA) and prelacrimal recess approach (PLRA) regarding their efficacy to remove filling paste from the maxillary sinus.
CT Imaging
All models got a computerized tomography (CT) scan prior to surgery. The models were scanned on a 64-slice CT scanner (Brilliance 64, Philips, Best, NL). Scanning parameters were collimation 64*0.625 mm, tube voltage 120 kVp, current time product 100 mAs; dose modulations were not used. Images were reconstructed with a standard kernel for bone reconstruction (kernel C) with a slice thickness of 1 mm and a reconstruction increment of 1 mm.
Surgical Technique
For surgical resection standard paranasal sinus endoscopic instruments were used (Karl-Storz, Tuttlingen, Germany). In each case surgery was performed by an experienced surgeon in functional endoscopic sinus surgery. Randomly chosen, the two maxillary sinuses underwent one of the two procedures: On the one hand endoscopic pre-lacrimal recess approach and on the other hand endoscopic middle meatal maxillary antrostomy was applied. Visualization was realized by the use of 0°, 45° and 70° rod lens endoscopes (HOPKINS® telescopes) combined with a highdefinition camera and monitor (Karl-Storz Endoscopy, Tuttlingen Germany). Operation time was measured and noted.
Middle Meatal Maxillary Antrostomy (MMMA): As first step in endoscopic middle meatal antrostomy the uncinate process was identified and medialized. By using backbiting forceps, the uncinate process was removed. With cutting forceps, the diameter of the maxillary sinus ostium was duplicated in the posterior direction. By using angulated endoscopes (45° and 70°) and angulated instruments the filling paste was removed.
Prelacrimal Recess Approach (PLRA): Endoscopic prelacrimal recess approach to maxillary sinus was performed as follows: First a vertical incision in the lateral nasal wall along the anterior margin of the inferior turbinate was made. The incision was continued to the nasal floor, then osteotomy of the medial maxillary wall was performed. This resulted in a wide access to the maxillary sinus. By using straight and angulated endoscopes (0° and 70°) and angulated instruments the filling paste was removed. Finally, the inferior turbinate was replaced to the origin position. Postoperative all models underwent an additional CT scan (Figure 2).
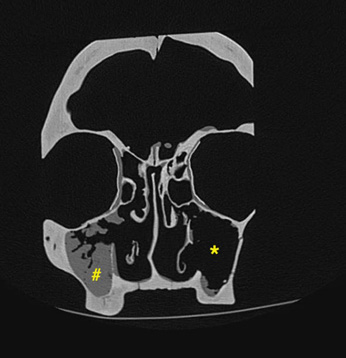
Figure 2: Postoperative paranasal sinus computed tomography scan of the coronal plane; # after middle meatal maxillary antrostomy; * after prelacrimal recess approach.
Image Post-Processing
Resulting images were post-processed with the use of dedicated software (Intellispace Portal, Philips, Best, NL). For volumetry, the filling material in each maxillary sinus was encircled on all contiguous slices in which the material was displayed. The software then created a 3D-model of the material and calculated the resulting volume by adding the product of slice area x slice thickness of the interesting structure. For further evaluation, maximum depth of the maxillary sinus was measured and divided into three equidistant parts. The primary volume was then virtually cut along these lines in three parts: anterior – middle – posterior (Figure 3). Resulting volumes were recorded respectively. Volumetric results were compared with standard statistical measuring using Microsoft Excel for Mac (version 15.14).
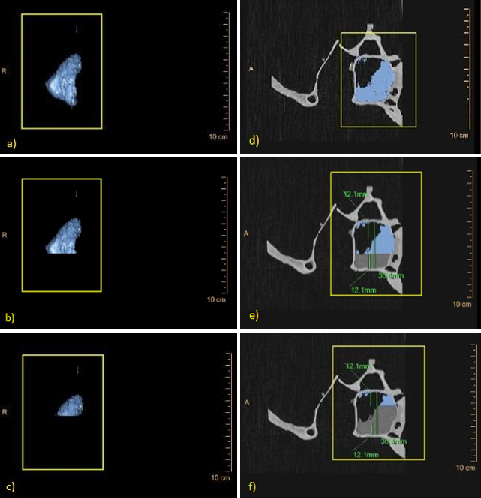
Figure 3: Imaging and illustration of measures derived from volumetry of the maxillary sinus a-c: 3D-models, and d-f: 2D-models CT-scan sagittal plane of a right maxillary sinus, the blue marked areas represent the filling paste of the maxillary sinus; a) total volume; b) volume of the middle and posterior area; c) volume of the posterior area; d) sagittal plane of the total area; e) middle and posterior area; f) posterior area.
Results
A summary of the two different surgical approaches regarding operation and volumetry data is shown in Table 1. Overall, the MMMA and also the PLRA were performed in eight cases. The mean operation time for the prelacrimal recess approach (tPLRA) was 18.24 minutes (range: 15.8-20.05 minutes). The mean surgical time of the middle meatal maxillary antrostomy (tMMMA) was 12.37 minutes (range: 8.33 – 15.67 minutes). This difference was statistically significant (tMMMA = 12.37 min vs. tPLRA = 18.24 min; p = 1.36 x10-4). The mean resected volume by using endoscopic prelacrimal recess approach was 11.94 cm3 (range: 10.8 – 15.0 cm3). Volumetry showed a mean volume difference (ΔVPLRA) between pre- and postoperative volumes of the maxillary sinus of 73.22% (range: 66.87 – 87.72%). The resected volume via middle meatall maxillary antrostomy was 6.1 cm3 (range: 4.9 – 8.8 cm3). We established a mean volume difference ΔVMMMA of 41.96% (range: 32.67 – 66.17%) for endoscopic middle meatal maxillary antrostomy. A significant volume difference between the preoperative and postoperative volume of the maxillary sinus was obtained (ΔVPLRA = 11.63 cm3 vs. ΔVMMMA = 6.10 cm3; p = 3.89 x 10-7; ΔVPLRA = 73.22% vs. ΔVMMMA = 41.96%; p = 1.66 x 10-4; Figure 4).
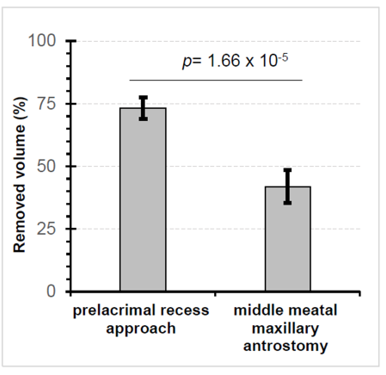
Figure 4: Comparison of percentage removed volume of the filling paste of maxillary sinus after prelacrimal recess approach (PLRA) and middle meatal maxillary antrostomy (MMMA) differ significantly (p value from 2-sided heteroscedastic t test).
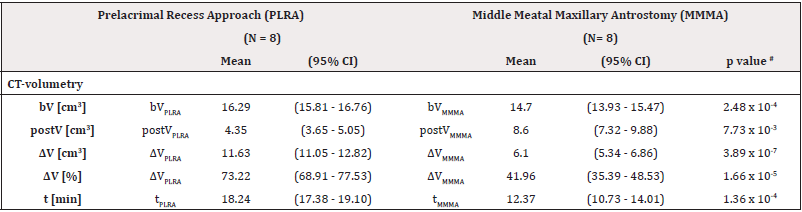
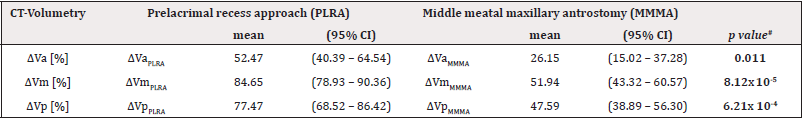
Table 1: Various parameters assessed by CT-based volumetry for comparison of prelacrimal recess approach (PLRA) and middle meatal maxillary antrostomy (MMMA).
Note*: b = baseline; post = postoperative; V = volume; t = time; # p value from 2-sided heteroscedastic t-tests
Via PLRA more tissue could be removed in all of the three thirds compared to the MMMA. Mean volume difference in the anterior (ΔVa), in the middle (ΔVm) and posterior (ΔVp) third was statistically significant (ΔVaPLRA = 52.47% vs. ΔVaMMMA = 26.15%; p = 0.011; ΔVmPLRA = 84.65 % vs. ΔVmMMMA = 11.94%; p = 8.12 x 10-5; ΔVpPLRA = 77.47% vs. ΔVpMMMA = 47.59%; p = 6.21 x 10-4). By using PLRA in each case, the volume of the resected material was higher than after MMMA. Most of the tissue could be removed in the middle third followed by the posterior and anterior third in both procedures (Table 2).
Discussion
In functional endoscopic sinus surgery (FESS), the middle meatal antrostomy has become the golden standard for the treatment of chronic maxillary sinus disease. However, Hosemann et al. [11] described different cases of chronic, recurrent or diffuse diseases of the maxillary sinus, in which full removal could not be achieved by middle meatal antrostomy despite the use of angled endoscopes, curved instruments or wide antrostomy. They have shown that the alveolar recess, the medial and anterior parts of the maxillary sinus are hard to reach. In contrast, the use of PLRA allows an easier access to the anterior parts of the maxillary sinus like the alveolar recess and the prelacrimal recess [12,13]. With our model test we could demonstrate that more tissue/volume could be removed in all parts of the maxillary sinus by using the PLRA. With a clear view and easier access another reduction of recurrence rates e.g. of sinonasal inverted papilloma is conceivable. With PLRA protection of risc structures like the nasolacrimal duct is possible.
Other reported endoscopic techniques for maxillary sinus access like the removal of the lower parts of the nasolacrimal duct or only its transposition by partially removal of the lacrimal bone with a diamond drill are more invasive and complications like stenosis of the nasolacrimal duct are conceivable. In our preclinical evaluation the MMMA requires less operation time than the PLRA. The PLRA requires a higher surgical workload compared to the MMMA – more steps are necessary to open the maxillary sinus. The use of a drill is required. For the MMMA the surgeon only has to enlarge the naturally ostium of the maxillary sinus with a punch. Overall, during the PLRA, instruments like Blakesley forceps had to be used more often to achieve removal of the tissue. Historically, the PLRA was developed by modifying endoscopic endonasal medial maxillectomy. Endoscopic endonasal medial maxillectomy was developed by Eloy et al. [9] and involves a complete resection of the medial wall of the maxillary sinus.
This procedure usually includes removal of the inferior turbinate and the nasolacrimal duct even if they are not involved in the disease. Postoperative complications like dry nose with crusting, epiphora or dacryocystitis are possible consequences. These are some of the reasons why different surgeons modified this approach to reduce the surgically caused morbidity and the complication rates. Preservation of the inferior turbinate could also help to avoid the empty nose syndrome [14]. Weber et al. [15] recommended medial maxillectomy with preservation of the inferior turbinate to treat patients with inverted papilloma of the maxillary sinus. In this surgical approach, the inferior turbinate is excised temporarily and reinserted at the end of the procedure. They propose to occlude the nose postoperative for at least 14 days. Suzuki et al. [10] reported a modified transnasal endoscopic medial maxillectomy with medial shift of the preserved inferior turbinate and nasolacrimal duct to resect inverted papilloma.
In this technique, a vertical incision was made along the anterior margin of the inferior turbinate to the nasal floor. Additionally, the medial maxillary wall was removed but the lateral nasal mucosa, nasolacrimal duct and inferior turbinate were shifted in the medial direction. In some cases, it was necessary to dissect the apertura piriformis and the anterior maxillary sinus bone. Nakayama et al. [4] also reported about endoscopic medial maxillectomy with preservation of the inferior turbinate and nasolacrimal duct. If the floor of the maxillary sinus is lower than the floor of the nose, it is difficult to remove the tumour from the inferior medial wall of maxillary sinus. In 2013, Zhou et al. [12] described the intranasal endoscopic prelacrimal recess approach to the maxillary sinus for the treatment of inverted papilloma, recurrent nasal polyps and cysts of the maxillary sinus. In their case series of 19 patients no intraoperative complications were noted. Postoperative well cured mucosa and normal inferior turbinate could be evaluated endoscopically.
After performing the postoperative CT scan at the 12-monthsfollow- up, they noticed a shrunken maxillary sinus with thickened mucosa. The PLRA can avoid additional incision and avoid damage to the anterior maxilla wall, to the infraorbital nerve and upper alveolar nerve [16]. Some authors support to combine MMMA and PLRA to provide a better drainage route for the maxillary sinus mucosa and to get wider access for postoperative endoscopic clinical follow-up [10,16]. For the treatment of malignant sinunasal tumors modified endoscopic maxillectomy via transnasal prelacrimal recess approach is a feasible therapeutic option. He et al. [17] described the resection of early stage maxillary carcinomas combined with pre- and/or postoperative radiotherapy in a small case series of 10 patients. The minimal invasive procedure may help to reduce the morbidity of open approaches. The PLRA provides a wide, clear and straight access to the maxillary sinus. These benefits are useful for other medical specialties like ophthalmology, oral maxillofacial surgery or skull base surgery.
The PLRA can be used to reach the pterygopalatine fossa and the infratemporal fossa by removing the posterolateral wall of the maxillary sinus. Gao et al. [13] dissected ten adult heads from formalin fixed cadavers. In this study, the distances were measured from the base of the columella to different anatomical landmarks of the pterygopalatine fossa and infratemporal fossa (sphenopalatine foramen, infraorbital artery and nerve, pterygopalatine ganglion or foramen rotundum). The authors reported about a clear visual field, wide range of exposure and preservation of the integrity of nasal structures. It is possible to resect lesions in the pterygopalatine and infratemporal fossa completely and safely by using the PLRA. There are also some case reports of removed schwannoma in the pterygopalatine fossa via the PLRA [18,19]. The PLRA describes an additional or alternative minimal invasive approach in skull base surgery. It is conceivable that biopsies of orbital tumors – intra- and extraconal lesions – are taken via the PLRA for further histological examination.
The PLRA can also be an alternative to external approaches like transconjunctival approach for treatment of orbital blow-out fractures. A lower eyelid complication rate of up to 5% (eyelid retraction, scleral show or ectropion) is reported after subciliary or transconjunctival incisions [20]. Endoscopic techniques like the transantral endoscopic approach were developed to repair orbital floor fractures. But there are still some disadvantages: large intraoral incision, frequent necessity of additional open approach and creation of a hole in the anterior wall of the maxillary sinus that is associated with a longer healing process. The PLRA is a better minimal invasive endoscopic procedure with less postoperative complications than the transantral endoscopic approach. Nevertheless, further research and preclinical tests are necessary to possibly integrate PLRA in orbital surgery. However, there are some limitations of our model test. Artificial skull models with physiological anatomical landmarks were used for our evaluation.
Each model was nearly identical without anatomical variants. The collected data apply only for the utilized Phacon sinus model with a predefined homogeneous anatomy. Because of the sticky texture of the filling material, no aspirators were used during the operation procedures. It is not possible to remove more tissue out of the maxillary sinus than the prepared filling material. Therefore, observations regarding postoperative complication rates like the appearance of bleedings, epiphora or necrosis of the inferior turbinate are not possible. Additionally, recurrence rates cannot be evaluated.
Conclusion
In summary, the prelacrimal recess approach is a suitable and minimal invasive method for volume reduction of pathologic tissue in the maxillary sinus in functional endoscopic sinus surgery. The PLRA provides a wide range of exposure and a clear visual field. All surgical steps can be performed by using 0° endoscopes and the integrity of nasal structures is preserved. The PLRA has the potential to be integrated more into the routine clinical use to treat various pathologies – not only in the maxillary sinus.
Acknowledgments
The authors thank Dr. Petersen for performing CT scans of the PHACON® models.
Compliance with ethical standards
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Ethical Statement
This article does not involve studies with any human participants or animals performed by any of the authors.
Informed Consent
This type of study does not require any informed consent.
References
- Weber RK, Hosemann W (2015) Comprehensive review on endonasal endoscopic sinus surgery. GSM Curr Top Otorhinolaryngol Head Neck Surg 14: Doc08.
- Kennedy DW, Adappa ND (2011) Endoscopic maxillary antrostomy: not just a simple procedure. Laryngoscope 121(10): 2142-2145.
- Kennedy DW, Zinreich SJ, Shaalan H, Kuhn F, Naclerio R, et al. (1987) Endoscopic middle meatal antrostomy: theory, technique, and patency. Laryngoscope 97(3): 1-9.
- Nakayama T, Asaka D, Okushi T, Yoshikawa M, Moriyama H, et al. (2012) Endoscopic medial maxillectomy with preservation of inferior turbinate and nasolacrimal duct. Am J Rhinol Allergy 26(5): 405-408.
- Lund VJ, Stammberger H, Nicolai P, Castelnuovo P, Beal T et al. (2010) European Rhinologic Society Advisory Board on Endoscopic Techniques in the Management of Nose, Paranasal Sinus and Skull Base Tumours: European position paper on endoscopic management of tumors of the nose, paranasal sinuses and skull base. Rhinol Suppl 22: 1-143.
- Philpott CM, Dharamsi A, Witheford M, Javer AR (2010) Endoscopic management of inverted papillomas: long-term results - the St. Paul’s Sinus Centre experience. Rhinology 48(3): 358-363.
- Goudakos JK, Blioskas S, Nikolaou A, Vlachtsis K, Karkos P, et al. (2018) Endoscopic Resection of Sinonasal Inverted Papilloma: Systematic Review and Meta-Analysis. Am J Rhinol Allergy 32(3): 167-174.
- Dean NR, Illing EA, Woodworth BA (2015) Endoscopic resection of anterolateral maxillary sinus inverted papillomas. Laryngoscope 125(4): 807-812.
- Eloy P, Mardyla N, Bertrand B, Rombaux P (2010) Endoscopic endonasal medial maxillectomy: case series. Indian J Otolaryngol Head Neck Surg 62(3): 252-257.
- Suzuki M, Nakamura Y, Nakayama M, Inagaki A, Murakami S et al. (2017) Modified transnasal endoscopic medial maxillectomy with medial shift of preserved inferior turbinate and nasolacrimal duct. Laryngoscope 121(11): 2399-2401.
- Hosemann W, Scotti O, Bentzien S (2003) Evaluation of telescopes and forceps for endoscopic transnasal surgery on the maxillary sinus. Am J Rhinol 17(5): 311-316.
- Zhou B, Han DM, Cui SJ, Huang Q, Wang CS (2013) Intranasal endoscopic prelacrimal recess approach to maxillary sinus. Chin Med J (Engl) 126(7): 1276-1280.
- Gao L, Zhou L, Dai Z, Huang X (2017) The Endoscopic Prelacrimal Recess Approach to the Pterygopalatine Fossa and Infratemporal Fossa. J Craniofac Surg 28(6): 1589-1593.
- Hildenbrand T, Weber RK, Brehmer D (2011) Rhinitis sicca, dry nose and atrophic rhinitis: a review of the literature. Eur Arch Otorhinolaryngol 268(1): 17-26.
- Weber RK, Werner JA, Hildenbrand T (2010) Endonasal endoscopic medial maxillectomy with preservation of the inferior turbinate. Am J Rhinol Allergy 24(6): 132-135.
- Yu QQ, Guan G, Zhang NK, Zhang XW, Jiang Y, et al. (2018) Intranasal endoscopic prelacrimal recess approach for maxillary sinus inverted papilloma. Eur Arch Otorhinolaryngol 275(9): 2297-2302.
- He S, Bakst RL, Guo T, Sun J (2015) A combination of modified transnasal endoscopic maxillectomy via transnasal prelacrimal recess approach with or without radiotherapy for selected sinonasal malignancies. Eur Arch Otorhinolaryngol 272(10): 2933-2938.
- Zhou B, Huang Q, Cui SJ, Wang CS, Li YC (2013) Removal of Schwannoma in the pterygopalatine and infratemporal fossa via endoscopic prelacrimal recess approach. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 48(10): 802-806.
- Guo T, Sun JW, Wang YF, Sun JQ (2014): Endoscopic endonasal surgery for pterygopalatine fossa schwannoma via prelacrimal recess-maxillary sinus. B-ENT 10(1): 81-86.
- Farwell DG, Sires BS, Kriet JD, Stanley RB (2007) Endoscopic Repair of Orbital Blowout Fractures Use ore Misuse of a new approach. Arch Facial Plast Surg 9(6): 427-433.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.