Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
22g Cannula - Vascular Occlusion After Nasal Filling with Hyaluronic Acid
*Corresponding author: Fernanda Bortolozo, Avenida das Américas, 3301-Bloco 4, Sala 301, Barra da Tijuca, Rio de Janeiro/RJ, Brasil
Received: April 01, 2020; Published: April 08, 2021
DOI: 10.34297/AJBSR.2021.12.001762
Abstract
Introduction: Tissue filling, which can be used in some cases of aesthetic dysfunction, may be an alternative to rhinoplasty. The use of dermal fillers can cause some complications depending on the planning, quantity and type of product, and characteristics of each patient. When compared to a needle, cannulas have been described in the literature as a considerably safer alternative to prevent vascular occlusion. Studies have found the 22G cannula to be the safest.
Objective: This study aimed to report a case, not described in the literature thus far, of late vascular occlusion in the nose caused by a tissue filler despite the use of a 22G cannula.
Methodology: This is a case report of vascular occlusion after a nasal filling using a 22G cannula.
Conclusion: The use of a 22G cannula in facial filling, in spite of being safer than needles, can also cause vascular occlusion.
Keywords: Hyaluronic acid; Vascular occlusion; 22G cannula; Complication; Tissue fillers; Rhinomodelation.
Introduction
Rhinoplasty is a delicate surgery that requires a lot of skill and experience from the plastic surgeon. In addition to choosing the professional, the patient must also consider factors of extreme importance, such as the high cost of the procedure, recovery time, possible interruption of daily activities, etc. [1].
Bearing in mind these considerations, the number of nonsurgical aesthetic procedures has grown considerably around the world [2]. Tissue filling can be an alternative to rhinoplasty. Known as rhinomodelation, it can be used in some cases of aesthetic dysfunctions. For this technique, either hyaluronic acid (HA) or polymethylmethacrylate (PMMA) can be used as fillers [2,3].
The use of soft-tissue fillers can cause some complications depending on the planning, quantity and quality of the product, and characteristics of each patient. Among the mildest complications there are edema, erythema, and hematoma. Moderate complications, such as overcorrection, Tyndall effect, and granuloma formation, can also be observed. Moreover, even though they are significantly less common events, more serious complications, such as anaphylaxis, stroke, and local necrosis, may occur. Regarding the most serious adverse outcomes, vascular occlusion, which can lead to necrosis, was the most prevalent [4-9].
When a vascular occlusion occurs, it is usually at the time of the procedure and, thus, the signs of this complication are detected by the responsible doctor. Hitherto, there are not studies showing vascular compression as a possible cause of necrosis days after the procedure.
In order to reduce the risks of this type of procedure, several safety protocols are followed. When compared to a needle, cannulas have been described in the literature as a considerably safer alternative to prevent vascular occlusion, because they have atraumatic, blunt tips. The 22G cannula has been found the safest. To date, there is no scientific evidence showing that soft-tissue filling done with a 22G cannula can cause vascular occlusion. Nevertheless, in this study, a clinical case in which there was vascular occlusion using this cannula size will be presented [10].
Methodology
This is a retrospective study of the clinical medical records of a patient who had vascular occlusion after undergoing a nose filling procedure with hyaluronic acid using a 22G cannula. The patient authorized the use of the information by signing an Informed Consent Form. This study was approved by the Veiga de Almeida University Research Ethics Committee under protocol number 43306620.4.0000.5291.
Clinical Case
A 43-year-old female patient was injected with 1 mL of hyaluronic acid (Rennova Ultra-Deep-Lido). The filler was distributed using a 22G cannula in the nasal dorsum, tip, and columella. Entry points on the nasal dorsum and lower columella region were done using 0.1 mL of 2% lidocaine without vasoconstrictor. Fourteen days after, 0.1 mL of hyaluronic acid (Rennova Lift) was injected in the columella for greater projection of the nasal tip. The procedure was carried out with no complications or signs of tissue distress. On the third day after the injection, the patient started to feel pain in the left nasal ala and contacted the clinic.
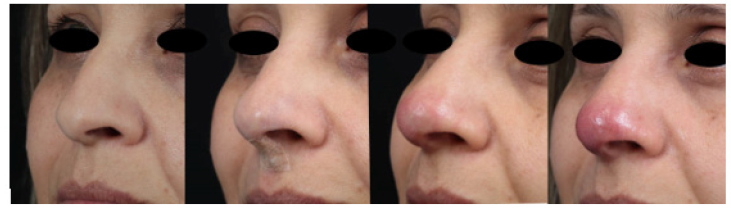
The patient was seen by the doctor immediately. She had 1 cm of gray skin on the left nasal ala with an erythematous halo across the nasal tip and columella. Hyaluronidase (1000UI) was injected followed by local massage. Immediately after it, blood flow returned to the ischemic area, leaving an erythema. The patient was prescribed acetylsalicylic acid (ASA) 300 mg/day, prednisone 40 mg/day, amoxicillin 875 mg + clavulanate potassium 125 mg for 7 days. Fifteen days after the beginning of the treatment, the patient had recovered fully without sequelae Figure1.
Discussion
According to the literature and the experience of several professionals, the use of 22G cannulas for injectable procedures is safer than needles, as those entail a lower risk of bursting a blood vessel and causing vascular occlusion [11].
As demonstrated in this report, vascular occlusion can happen three days after the injection of the tissue filler. It is believed that the overhydration caused by hyaluronic acid could be responsible for late occlusion, as well as extrinsic compression of the angular artery and lateral nasal artery branch.
Even though reperfusion is not guaranteed, early diagnosis and immediate initiation of filler dissolution, along with mechanisms of vasodilation, reduction of inflammation, and prevention of infection, allow for better results in the ischemic area in cases of extrinsic compression.
In this study, the patient recovered completely, with no sequelae, from the ischemic event related to the rhinomodelation with hyaluronic acid.
Conclusion
This study demonstrated that late vascular occlusion of the lateral nasal artery branch can happen even with the use of the cannula size recommended by current studies. Although the use of a 22G cannula may prevent intravascular injection of the product, late extrinsic compression should be considered by the doctor, and treatment should be carried out as early as possible.
References
- Armitage SJ, Jasim SA, Marks AE, Parker AG, Usik VI, et al. (2011) The southern route “out of Africa”: Evidence for an early expansion of modern humans into Arabia. Science 331(6016): 453-456.
- Lawler A (2011) Did Modern Humans Travel Out of Africa Via Arabia? Science 331(6016): 387-387.
- Rasmussen M, Guo X, Wang Y, Lohmueller KE, Rasmussen S, et al. (2011) An Aboriginal Australian genome reveals separate human dispersals into Asia. Science 334(6052): 94-98.
- López S, Van Dorp L, Hellenthal G (2016) Human Dispersal Out of Africa: A Lasting Debate. Evolutionary Bioinformatics 11(Suppl 2): 57-68.
- Lazaridis I, Patterson N, Mittnik A, Renaud G, Mallick S, et al. (2014) Ancient human genomes suggest three ancestral populations for present-day Europeans. Nature 513(7518): 409-413.
- Botigue LR, Henn BM, Gravel S, Maples BK, Gignoux CR, et al. (2013) Gene flow from North Africa contributes to differential human genetic diversity in southern Europe. Proceedings of the National Academy of Sciences 110(29): 11791-11796.
- Currat M, Excoffier L (2005) The effect of the Neolithic expansion on European molecular diversity. Proceedings of the Royal Society B: Biological Sciences 272(1564): 679-688.
- Lazaridis I, Mittnik A, Patterson N, Mallick S, Rohland N, et al. (2017) Genetic origins of the Minoans and Mycenaeans. Nature 548(7666): 214-218.
- Lazaridis I, Nadel D, Rollefson G, Merrett DC, Rohland N, et al. (2016) Genomic insights into the origin of farming in the ancient Near East. Nature 536(7617): 419-424.
- Qin P, Zhou Y, Lou H, Lu D, Yang X, et al. (2015) Quantitating and Dating Recent Gene Flow between European and East Asian Populations. Scientific Reports 5: 9500.
- Font-Porterias N, Arauna LR, Poveda A, Bianco E, Rebato E, et al. (2019) European Roma groups show complex West Eurasian admixture footprints and a common South Asian genetic origin. PLoS Genetics 15(9): e1008417.
- Mendizabal I, Lao O, Marigorta UM, Wollstein A, Gusmão L, et al. (2012) Reconstructing the population history of European Romani from genome-wide data. Current Biology 22(24): 2342-1349.
- Moorjani P, Patterson N, Loh PR, Lipson M, Kisfali P, et al. (2013) Reconstructing Roma history from genome-wide data. PLoS One 8(3): e58633.
- Hellenthal G, Busby GBJ, Band G, Wilson JF, Capelli C, et al. (2014) A genetic atlas of human admixture history. Science 343(6175): 747-751.
- Lipson M, Loh PR, Levin A, Reich D, Patterson N, et al. (2013) Efficient moment-based inference of admixture parameters and sources of gene flow. Molecular Biology and Evolution 30(8): 1788-1802.
- Li H, Durbin R (2009) Fast and accurate short read alignment with Burrows-Wheeler Transform. Bioinformatics 25(14): 1754-1760.
- Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, et al. (2009) Genome Project Data Processing Subgroup, The Sequence Alignment/Map format and SAMtools. Bioinformatics 25(16): 2078-2079.
- Danecek P, Auton A, Abecasis G, Albers CA, Banks E, et al. (2011) The variant call format and VCFtools. Bioinformatics 27(15): 2156-2158.
- Alexander DH, Novembre J, Lange K (2009) Fast model-based estimation of ancestry in unrelated individuals. Genome Research 19(9): 1655-1664.
- Talevich E, Shain AH, Botton T, Bastian BC (2016) CNVkit: Genome-Wide Copy Number Detection and Visualization from Targeted DNA Sequencing. PLOS Computational Biology 12(4): e1004873.
- Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, et al. (2006) Principal components analysis corrects for stratification in genome-wide association studies. Nature Genetics 38(8): 904-909.
- Pickrell JK, Pritchard JK (2012) Inference of population splits and mixtures from genome-wide allele frequency data. PLoS Genetics 8(11): e1002967.
- Reich D, Thangaraj K, Patterson N, Price AL, Singh L (2009) Reconstructing Indian population history. Nature 461(7263): 489-494.
- Raghavan M, Skoglund P, Graf KE, Metspalu M, Albrechtsen A, et al. (2014) Upper Palaeolithic Siberian genome reveals dual ancestry of Native Americans. Nature 505(7481): 87-91.
- Busing FMTA, Meijer E, Van Der Leeden R (1999) Delete- m Jackknife for Unequal m. Statistics and Computing 9: 3-8.
- Bai H, Guo X, Narisu N, Lan T, Wu Q, et al. (2018) Whole-genome sequencing of 175 Mongolians uncovers population-specific genetic architecture and gene flow throughout North and East Asia. Nature Genetics 50(12): 1696-1704.
- Browning BL, Browning SR (2013) Improving the accuracy and efficiency of identity-by-descent detection in population data. Genetics 194(2): 459-471.
- Browning BL, Browning SR (2011) A fast, powerful method for detecting identity by descent. American Journal of Human Genetics 88(2): 173-182.
- Xu S, Huang W, Qian J, Jin L (2008) Analysis of genomic admixture in Uyghur and its implication in mapping strategy. American Journal of Human Genetics 82(4): 883-894.
- Mills RE, Walter K, Stewart C, Handsaker RE, Chen K, et al. (2011) Mapping copy number variation by population-scale genome sequencing. Nature 470(7332): 59-65.
- Conrad DF, Pinto D, Redon R, Feuk L, Gokcumen O, et al. (2010) Origins and functional impact of copy number variation in the human genome. Nature 464: 704-712.
- Rodriguez-Flores JL, Fakhro K, Agosto-Perez F, Ramstetter MD, Arbiza, L, et al. (2016) Indigenous Arabs are descendants of the earliest split from ancient Eurasian populations. Genome Research 26(2): 151-162.
- Raveane A, Aneli S, Montinaro F, Athanasiadis G, Barlera S, et al. (2019) Population structure of modern-day Italians reveals patterns of ancient and archaic ancestries in Southern Europe. Science Advances 5(9): eaaw3492.
- Hunter-Zinck H, Musharoff S, Salit J, Al-Ali KA, Chouchane L, et al. (2010) Population Genetic Structure of the People of Qatar. American Journal of Human Genetics 87(1): 17-25.
- Regueiro M, Garcia-Bertrand R, Fadhlaoui-Zid K, Álvarez J, Herrera RJ (2015) From Arabia to Iberia: A Y chromosome perspective. Gene 564(2): 141-152.
- Dumas L, Kim YH, Karimpour-Fard A, Cox M, Hopkins J, et al. (2007) Gene copy number variation spanning 60 million years of human and primate evolution. Genome Research 17(9): 1266-1277.
- Jones RJ, Tay GK, Mawart A, Alsafar H (2017) Y-Chromosome haplotypes reveal relationships between populations of the Arabian Peninsula, North Africa and South Asia. Annals of Human Biology 44(8): 738-746.
- Lupski JR (2007) Genomic rearrangements and sporadic disease. Nature Genetics 39(7 Suppl 1): S43-S47.
- Lebling RW (2009) "The Saracens of St. Tropez". Saudi Aramco World.
- Metspalu M, Kivisild T, Metspalu E, Parik J, Hudjashov G, et al. (2004) Most of the extant mtDNA boundaries in south and southwest Asia were likely shaped during the initial settlement of Eurasia by anatomically modern humans. BMC Genetics 5: 26.
- Gonzalez AM, Garcia O, Larruga JM, Cabrera VM (2006) The mitochondrial lineage U8a reveals a Paleolithic settlement in the Basque country. BMC Genomics 7: 124.
- Redman CL (1978) The rise of civilization. From early farmers to urban society in the ancient Near East. WH Freeman and Company, San Francisco, USA, pp. 183.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.