Commentary 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Chronic Recurrent Multifocal Osteomyelitis Evolving into Primary Bone Marrow Hodgkin Lymphoma
*Corresponding author: Daniel Benharroch, Department of Pathology, Soroka University Medical Centre, 151 Rager Blvd, P.O.Box 151, Beer-Sheva 84101, Israel
Received: May 12, 2021; Published: May 18, 2021
DOI: 10.34297/AJBSR.2021.12.001811
Abstract
Chronic recurrent multifocal osteomyelitis, a systemic inflammatory condition, prevails in children, with fever, night sweats and bone pain in the spine and to a lesser degree in the extremities. This disease is rare and is generally diagnosed with difficulty. One of the differential diagnoses thereof, the primary bone marrow Hodgkin lymphoma, displays many similarities with this disorder. However, as a malignant tumor with a poor outcome, this rare variant of classic Hodgkin lymphoma, might eventually stand out as a systemic nodal lymphoma, worsened by an HIV infection, the diagnosis being established at times with a delay as long as 17 months.
Keywords: Recurrent Multifocal Osteomyelitis; Bone Marrow Hodgkin Lymphoma; Systemic Nodal Hodgkin Lymphoma; Refractory Tumor
Chronic Recurrent Multifocal Osteomyelitis
The malady (CRMO) occurs rarely with systemic symptoms, in children, with bone pain, mainly localized in the spine, with fever and night sweats. Early, in the course of the disease, the orthopaedic surgeon should raise the differential diagnosis of a myeloproliferative disorder, or of a metastatic tumor [1]. As the patient is found in a good general condition, that she/he displays a normal blood count, and she/he shows no lymphadenopathy, the diagnosis of lymphoma is not suggested. Chronic non-bacterial osteitis is the older term used for CRMO [1].
The multifocal bone pain is the basis of the ailment (CRMO); therefore imaging and bone marrow/bone investigations are requested. Bone marrow aspirations and biopsies, in a routine work-up, may show a non-specific excess of lymphocytes, polyclonal plasma cells and fibrosis. In the process, metastatic tumors and myeloproliferative disorders are relatively easy to exclude [2,3].
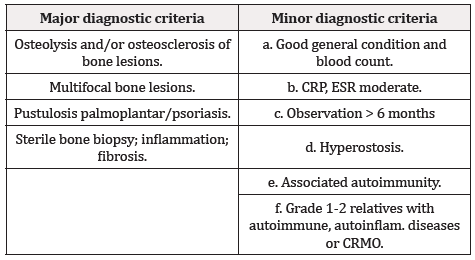
A CT scan-directed open bone biopsy should be obtained to confirm CRMO and rule out a lymphoma. In addition to the CT-scan, an MRI, as well as a 18F-FDG-PET/CT scan should be employed, the latter, to diagnose a primary bone marrow Hodgkin lymphoma [4,5]. Due to the complexity of the diagnosis of CRMO, Jansson et al have established their criteria (Table 1). Two major criteria, or one major and three minor criteria are necessary to establish the diagnosis of CRMO. However, the trial is not over. As mentioned, CRMO is rare. Moreover, most physicians are not familiar with the illness and its manifestations [3].
Primary bone Marrow Hodgkin lymphoma
To compound further the issue, a clinicopathological entity, with many similar characteristics, a poor outcome, consistent with malignancy, has been described: Primary bone marrow Hodgkin lymphoma (PBMHL), is a rare subset of classic Hodgkin lymphoma (< 1% of CHL) [5,6].
This disease entity is confined to the bone marrow of the spine, and it is multicentric. These patients show a delayed diagnosis, which might disclose a nodal CHL, after as long as 17 months from the first symptoms. During that period, no lymph node involved by CHL is to be identified. However, as a rule, the illness will progress into a nodal, systemic form of CHL, which is mostly resistant to standard therapy [4,7-8].
A further trait that will transform these cases into refractory tumors, is the association in a large part of primary bone marrow Hodgkin lymphoma, with HIV-positivity. This type of CHL have a predilection for HIV infection and with the elderly [9-11].
The bone marrow biopsy in these patients, will identify small regular lymphocytes, histiocytes, reticular fibrosis and relatively few Hodgkin/Reed-Sternberg cells, expressing CD30+, CD15+, MUM1+; PAX5+ (weak).
A CRMO patient might either progress to PBMHL, or she/he might prove to be a PBMHL from inception [12,13]. The patient might progress eventually to a systemic nodal CHL. In a series of 12 CRMO children, only one child developed the picture of PBMHL. Rarely, a PBMHL patient will respond to therapy [14].
Conclusions
Two rare maladies have been described in a single context. They display analogous clinical features, although, one is a benign inflammatory lesion, while the other is an aggressive malignant tumor, which shows a propensity to occur together with an HIV infection. Although, early in the course of the disease they may be confounded, they remain entirely distinct.
References
- Bhat CS, Anderson C, Harbinson A, McCann LJ, Roderick M, et al. (2018) Chronic non-bacterial osteitis (CRMO) a multi-centre study. Pediatr Rheumatol 16: 74-80.
- Rao AP, Mallya PP, Ranjani S, Raghuram J (2018) Chronic recurrent multifocal osteomyelitis – a case series from India. Indian J Orthop 52: 672-677.
- Kumar TKJ, Salim J, Shamsudeen TJ (2018) CRMO-a rare clinical presentation and review of the literature. J Orthop Case Rep 8(3): 3-6.
- Citow JS, Rini B, Wollmann R, Macdonald RL (2001) Isolated primary extranodal Hodgkin disease of the spine. Neurosurgery 49(2): 453-456.
- Breibach F, Julian A, Laurent C, Eric Anglade, Arnaud Constantin, et al. (2009) Contribution of the 18F-FDG-Pet/CT to the diagnosis of primary osseous Hodgkin lymphoma. BMJ Case Rep 2009:1-8.
- Sekine I, Sasaki Y, Hasebe T, Umeda T, Mukai K, et al. (1997) Coxalgia as the initial symptom of Hodgkin disease: a case report. Jpn J Clin Oncol 27: 353-356.
- Ha-ou-nou FZ, Benjilali L, Essaadouni L (2013) Sacral pain as the initial symptom in primary Hodgkin’s lymphoma of bone. J Cancer Res Ther 9: 511-513.
- Uehara M, Takahashi J, Hirabayashi H, Jun Kitahara, Tetsuyoshi Kamijyo, et al. (2013) Hodgkin disease of the thoracic vertebrae. Spine J 13: e59-63.
- Shah BK, Subramariniam S, Peace D, Garcia C (2010) HIV-associated primary bone marrow Hodgkin lymphoma: a distinct entity? J Clin Oncol 28: e459-e460.
- Ponzoni M, Fumagalli L, Rossi G, Massimo Freschi, Alessandro Re, et al. (2002) Isolated bone marrow manifestations of HIV-associated Hodgkin lymphoma. Mod Pathol 15: 1273-1278.
- Ponzoni M, Ciceri F, Crocchiolo R, G Famoso, C Doglioni (2006) Isolated bone marrow occurrence of classic Hodgkin lymphoma in an HIV-negative patient. Haematologica 91: 1-2.
- Pham M, Ressler S, Rosenthal A, Kelemen K (2017) Classical Hodgkin lymphoma masquerading as chronic recurrent multifocal osteomyelitis. J Medical Case Rep 11: 45.
- Griguolo G, Mazzucchelli L, Cavalli F, et al. (2015) A case of Hodgkin lymphoma in a patient with a history of bone pain and an initial diagnosis of chronic osteomyelitis. Tumori 101(3): e99-e102.
- Nagaharu K, Masuya M, Kageyama Y, Takanori Yamaguchi, Ryugo Ito, et al. (2018) Successful treatment of primary bone marrow Hodgkin lymphoma with brentuximab vedotin. J Med Case Report 12(1): 151.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.