Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Radiotherapy for Inflammatory Breast Cancer (IBC) in the Modern Multi-Modality Treatment Era: A Provincial Retrospective Review Over 12 Years
*Corresponding author: Tien Phan, Department of Oncology, University of Calgary, 1331 – 29th Street NW T2N 4N2 Calgary, AB Canada, Phone: +1-4035213077, Email: Tien.Phan@albertahealthservices.ca, Fax: 403-283-1651
Received: April 14, 2020; Published: April 22, 2021
DOI: 10.34297/AJBSR.2021.12.001776
Abstract
Purpose: The primary objective of this retrospective review was to determine the locoregional recurrence rates in non-metastatic Inflammatory Breast Cancer (IBC) patients treated with modern multi-modal therapy. Secondary objectives included assessing the impact of hypofractionation on 5-year outcomes (LRC, OS, DFS, DMFS) and identifying predictors of loco-regional relapse to select patients who may benefit from dose escalation.
Materials and Methods: All patients diagnosed with non-metastatic IBC (T4d, M0 at diagnosis) at all institutions in the province between 2000 and 2011 were identified from the Cancer Registry. Patients treated with triple modality therapy (chemotherapy, surgery and adjuvant radiation therapy) were included in the analysis. 5-year outcomes and First Site of Failure (FSOF) distributions were calculated.
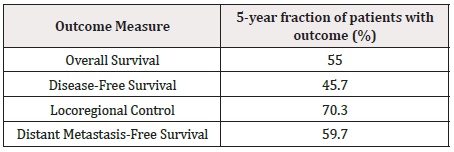
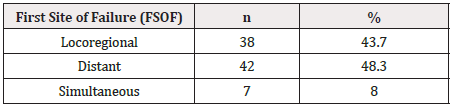
Results: A total of 177 patients met eligibility criteria, all of whom received anthracycline, and/or taxane based chemotherapy. At 5 years, LRC was 70.3%, OS was 55.0%, DFS was 45.7% and DMFS was 59.7%. 102 patients received Hypo Fractionated (HypoF) RT and 75 patients received Conventional Fractionation (CF) RT. 5-year outcomes were not statistically different between HypoF and CF regimens. Of those who recurred, FSOF were locoregional (43.7%), distant (48.3%) and simultaneous (8.0%) - there was no significant difference between HypoF and CF regimens. Patients who first failed locoregionally had significantly worsened survival outcomes. Patients with Triple Negative (TN) disease were more likely to first fail locoregionally, while patients with hormone receptor-positive, HER2-negative disease (HP+/HER2-) were less likely to first fail locoregionally.
Conclusions: IBC patients in this study experienced poor locoregional outcomes, including poor LRC and frequent LR FSOF. Survival and recurrence outcomes were independent of radiotherapy regimen, while survival outcomes were significantly worsened by LR FSOF. Hormone status was found to be a key prognostic factor for locoregional outcomes, suggesting the benefit of PMRT dose escalation in high-risk subpopulations, especially those with TN disease
Introduction
Inflammatory Breast Cancer (IBC) is a rare and aggressive subtype of breast cancer that represents 1% - 6% of all breast cancer incidence [1-6]. Although IBC is an invasive disease with rapid onset of symptoms, more than 70% of patients present with clinically localized disease at diagnosis [2,7]. As such, most patients are candidates for multimodal therapy, including neoadjuvant chemotherapy, mastectomy, and radiotherapy [4]. While the use of modern multimodal therapy has improved outcomes, prognosis remains poor with only a 30% five-year overall survival rate [5,6]. The rapid progression and early metastatic potential of IBC present challenges with high rates of both locoregional and distant failure [4,8]. Current knowledge of patterns of survival and recurrence are limited to smaller case series, and not within the context of modern multimodal therapy [9-12].
Locoregional Control (LRC) is a particularly important consideration for IBC disease management, as a strong association between Locoregional Recurrence (LRR) and Overall Survival (OS) has been demonstrated [2,13]. Post-Mastectomy Radiation Therapy (PMRT) plays a central role in the treatment course and has been shown to improve LRC and OS for non-metastatic IBC [2,5]. There is some thought that intensifying radiotherapy regimens may improve outcomes, including strategies like dose escalation, twice daily radiation treatment and hypofractionation [5,9]. However, these regimens are typically longer, more resource intensive, and can be associated with increased radiotherapy-related toxicities. Furthermore, there is difficulty in identifying high-risk candidates for dose escalation due to largely ineffective predictors of locoregional response [9,10,12,14-21]. Additionally, many previous studies that demonstrated the benefit of post-mastectomy radiotherapy in this patient population did not include patients treated with modern multi-modal therapy, namely anthracycline/ taxane based chemotherapy [9-12].
The purpose of this investigation was to examine the patterns of survival and recurrence among inflammatory breast cancer patients treated multimodal therapy over a 12-year span starting in the year 2000 when anthracycline-taxane based chemotherapy was routinely implemented. The primary objectives were to determine locoregional recurrence rates in the modern multimodality treatment era and to characterize predictors of relapse to identify patients that have historically benefited from arduous dose-escalation radiotherapy regimes.
Methods and Materials
Study Population
Ethics approval was obtained from the Health Research and Ethics Board of the province for retrospective chart analysis of inflammatory breast cancer diagnoses from Jan 1, 2000-Dec 31, 2011. Patients were included as eligible if their TNM stage was T4d, M0, and they were treated with chemotherapy, mastectomy, and post-mastectomy radiotherapy. All charts of eligible patients were identified and obtained using the Provincial Cancer Registry and reviewed by the multidisciplinary team. Patients were excluded due to unavailable RT information, lack of multimodal therapy including chemotherapy, modified radical/total mastectomy surgery and adjuvant RT, palliative intent, significant comorbidities defined as ≥ Grade 3, by CTCAE v5.0, multiple primaries at diagnosis (Table 1). The charts of eligible patients were reviewed up to January 2020 for primary and secondary outcomes.
Variables
All outcome variables considered in the analyses were extracted from the Cancer Registry and individual Electronic Medical Record (EMR). All outcome variables were calculated from the date of pathological confirmation of IBC diagnosis. Primary outcome was Locoregional Control (LRC), defined as freedom from clinical or radiographic evidence of recurrent malignancy within the chest wall, sternum or regional lymph nodes. Secondary outcomes included Overall Survival (OS), Disease-Free Survival (DFS) and Distant Metastasis-Free Survival (DMFS). First site of Failure (FSOF) was classified as locoregional, distant or simultaneous.
Treatment
Radiotherapy treatment regimen variable collection included total prescribed dose and fractionation. Patients were divided into two distinct groups based on dose and fractionation of RT regimen: Hypo fractionated regimens (HypoF: >2 Gy/day; 40-50 Gy/16-20#) and Conventional Fractionation regimens (CF: 2 Gy/ day; 50 Gy/25#). Covariates included the following: patient age, tumor grade, tumor hormone status, HER2 status, Lymphovascular Invasion (LVSI) status, and nodal stage. Hormone Status was grouped by Estrogen Receptor (ER), Progesterone Receptor (PR) and Human Epidermal Growth Factor Receptor 2 (Her2) Status. Triple Positive (TP) disease is classified as positive in ER, PR and HER2 status. Triple Negative (TN) disease is classified as negative in ER, PR and HER2 status. Hormone Positive (HP) disease is classified as positive in either or both ER or PR, while Hormone Negative (HN) disease is classified as negative in both ER and PR.
Statistical Analyses
All data was collected and stored on Research Electronic Data Capture (REDCap), and all statistical analyses were performed using SPSS v16. Radiotherapy regimen group differences were determined using the chi-squared test for categorical variables, while independent sample’s T-test was used for continuous variables. Patterns of LRC, DFS, DMFS and OS were calculated using the Kaplan-Meier statistic and the log-rank sum test for significance, while 5-year outcomes were determined through life tables. Univariable association was performed using Logistic Regression, and multivariable association was performed using Cox Regression analysis. All p-values were two-sided and with the significance level α = 0.05.
Results
Demographics
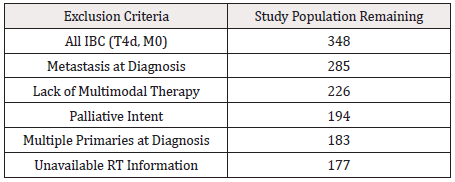
Of 348 patients who were diagnosed with Inflammatory Breast Cancer (T4d, M0) between 2000 and 2011, there were 177 patients who met the inclusion criteria (Table 1). All patients were female with a median (range) age at diagnosis of 53 years (24-81). Most patients had grade 3 disease (82.5%) and Lymphovascular invasion (71.8%). Patients received systemic therapy, surgery, additional radiotherapy, hormone or biologic therapy for locoregional or distant recurrences, dependent on disease progression and provider discretion. Median follow-up was 67 months (range 9-190 months) (Table 2).
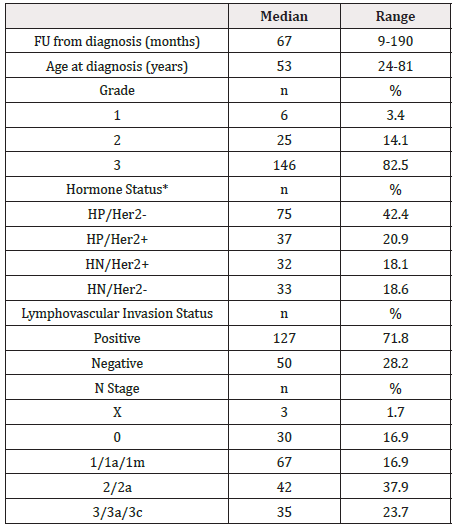
Table 2: Study population patient characteristics at initial diagnosis of IBC and subsequent treatment information
*HP: Either ER-positive or PR-positive, HN-: ER and PR negative.
Patient Outcomes
Locoregional control at 5 years was 70.3%, while OS was 55.0%, DFS was 45.7% and DMFS was 59.7% (Table 3). A total of 87 patients recurred following diagnosis, and First Site of Failure (FSOF) was locoregional for 38 (43.7%) patients, distant for 42 (48.3%) patients and simultaneous locoregional and distant for 7 (8.0%) patients (Table 4). Patients who first failed locoregionally had significantly worse 5-year outcomes, including overall survival (36.8% LR FSOF vs. 61.1% in others, p < 0.001), disease free survival (15.8% LR FSOF vs. 54.9% in others, p <0.001), locoregional control (15.8% LR FSOF vs. 89.2% in others, p < 0.001), and distant metastasis free survival (43.9% vs 64.9%, p = 0.019) (Table 5).
Impact of Regimen on Patient Outcomes
There were no significant differences of patient characteristics including age, grade, hormone status, LVSI or N stage between HypoF and CF regimen groups. Differences in 5-year survival outcomes between regimen groups were not statistically significant. At 5 years, patients who received HypoF regimens trended towards improved OS (59.2% HypoF vs. 53.2% CF, p = 0.981), DFS (50.2% HypoF vs. 43.7% CF, p = 0.976), LRC (74.5% HypoF vs 68.8% CF, p = 0.809) and DMFS (65.8% HypoF vs. 57.2% CF, p = 0.757) (Table 6). FSOF differences between regimens groups were not significant (p = 0.191), although patients who received hypo-fractionated regimens trended towards more frequent distant (50.0% HypoF vs. 45.7%% CF) and simultaneous (11.5% HypoF vs. 2.9% CF) first sites of failure. Patients who received conventional fractionation regimens trended towards more frequent locoregional (38.5% HypoF vs. 51.4% CF) first site of failure (Figure 1).

Table 5: 5-year outcomes for study population, with comparison between locoregional first site of failure and all other patients.
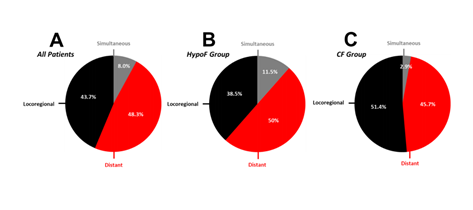
Figure 1: Distribution of FSOF, by RT regimen groups. Panel A represents distribution of FSOF within total study population, while Panel B represents FSOF within HypoF regimen group and Panel C represents FSOF within CF regimen group. Black sections represent locoregional recurrence, red sections represent distant recurrence and grey sections represent simultaneous recurrence.
Predictors of Locoregional Recurrence
On univariate logistic regression, FSOF was demonstrated to be significantly associated with hormone status (p = 0.025). On multivariate cox regression, locoregional control was demonstrated to be significantly associated with hormone status (p = 0.028). Regimen group was not significantly associated with FSOF or LRC. HP/HER2- patients were significantly less likely to have locoregional FSOF (26.3% HP/HER2-vs 57.1% in others, p = 0.004), while TN patients were significantly more likely to have locoregional FSOF (72.2% TN vs 36.2% in others, p = 0.006) (Figure 2). Individual hormone status was also significantly associated with LRC, with significantly worsened LRC among TN patients (57.2% TN vs. 73.3% in others, p = 0.044).
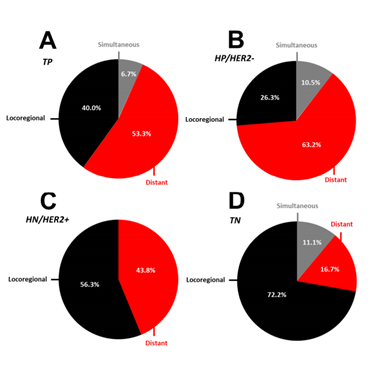
Figure 2: Distribution of FSOF, by hormone receptor status. Panel A represents TP (Triple Positive) patients, Panel B represents HP/Her2- patients, Panel C represents HN/Her2+ patients and Panel D represents TN (Triple Negative) patients. Black sections represent locoregional recurrence, red sections represent distant recurrence and grey sections represent simultaneous recurrence.
Discussion
Triple modality (surgery, chemotherapy, and radiotherapy) has been the primary recommendation in definitive treatment for nonmetastatic IBC since the early 2000s [4]. However, locoregional recurrence rates have remained high despite routine use of PMRT in the order of ~30-40% [5,6]. Several studies have shown improvement in locoregional control and improved survival in patients who receive escalation of PMRT doses via hyper fraction and/or use of electron bolus [9,10,16-20]. However, many studies investing inflammatory breast cancer outcomes and patterns of recurrence, are limited to an era before multimodal therapy or modern chemotherapy [9-12]. This study, the largest multiinstitutional retrospective review investigating PMRT dosing strategy in IBC, was conducted to investigate the impact of RT regimen hypofractionation on an IBC population in a modern therapeutic context.
Study 5-year patient outcomes were comparable with other studies and institutional data [7,22-25], in local control as well as survival data. Approximately half of this cohort of patients experienced recurrent malignancy, and the incidence of locoregional and distant recurrence as FSOF was like previous. Locoregional recurrence appears to be a crucial disease management consideration, as it was significantly associated with worse 5-year survival outcomes.
Survival outcome differences at 5 years were not statistically significant between hypofractionation and conventional regimens. Hormone receptor status was significantly associated with patterns of recurrence on both univariate and multivariate analysis. Patients with triple negative disease did particularly poorly, with significantly worse LRC, with 72% failing locoregionally within 5 years. HP/HER2- disease on the other hand was significantly less likely to fail first locoregionally. These findings align with previous studies that have shown the association between hormone receptor and HER2 status of disease and survival outcomes in patients with IBC, but this also identifies hormone status as a key prognostic indicator for locoregional outcomes, including locoregional control and locoregional recurrence [15,24-26]. Radiation dose escalation might be a relevant strategy in dealing with the particularly poor locoregional control in patients with triple negative IBC. This strategy is supported with improved LRC in recent IBC case series from MDACC with the radiation dose escalation to > 60 Gy EQD21.
The large sample size of 177 patients distinguishes this study as the largest multi-institutional retrospective study investigating PMRT dosing strategy for IBC in patients treated with modern multimodal therapy. As compared to existing investigations into PMRT dosing strategy in IBC, this study builds current knowledge on patterns of survival and recurrence of IBC patients in the context of modern multimodal treatment regimens. In addition, this study demonstrated hormone status as a key prognostic factor for locoregional outcomes, in the context of conventional PMRT dose regimens. However, as a retrospective study, this analysis has several limitations. Although registry data was comprehensive, data was not collected for primary use, and several important clinical confounders may be absent. Despite having a large sample size in comparison to previous analyses, power of statistical analysis may be limited due to the low incidence of IBC, even over a 10-year period across a major Canadian province. Furthermore, there were large differences in dose and fractionation specifications within regimen groups, which may indicate shifting clinical RT practices over the longitudinal study period.
Conclusions
IBC patients receiving modern multimodal therapy from 2000- 2011 still demonstrated poor locoregional outcomes, including LRC and frequent LR FSOF. Outcomes were found to be independent of fraction of radiotherapy regimen, with no significant differences in patterns of survival or recurrence between hypo fractionated and conventional fractionation regimen groups. Importance of locoregional control was demonstrated by significantly worsened survival outcomes in patients with locoregional recurrence as the first site of failure. Hormone status was found to be a key prognostic factor for locoregional outcomes, and findings on individual hormone statuses suggest that escalation of radiation dose may especially benefit high-risk subpopulations, such as patients with triple negative disease.
Conflict of Interest Statement: The authors declare no conflicts of interest.
Grants and Financial Support: None
References
- REGULATION (EU) 2017/745 OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC.
- COUNCIL DIRECTIVE 93/42/EEC of 14 June 1993 concerning medical devices.
- Wright E, Roy F, Roussanov A (2010) Understanding the promotion of medical devices in the European Union. Journal of Medical Device Regulation 7(1): 3-6.
- Dennis A (2020) Advertising medical devices in the EU – Do the MDR and IVDR represent a change in EU law? Journal of Medical Device Regulation 17(1): 21-25.
- (2018) Connecting Europe - False advertising in life sciences. Hogan Lovells Publications.
- DIRECTIVE 2005/29/EC OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 11 May 2005 concerning unfair business-to-consumer commercial practices in the internal market and amending Council Directive 84/450/EEC, Directives 97/7/EC, 98/27/EC and 2002/65/EC of the European Parliament and of the Council and Regulation (EC) No 2006/2004 of the European Parliament and of the Council (‘Unfair Commercial Practices Directive’).
- DIRECTIVE 2006/114/EC OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 12 December 2006 concerning misleading and comparative advertising.
- Directive 2006/114/EC of the European Parliament and of the Council of 12 December 2006 concerning misleading and comparative advertising.
- (2012) EASA Best Practice on Claims Substantiation. European Advertising Standards Alliance (EASA), Belgium.
- (2015) The MedTech Europe Code of Ethical Business Practice. MedTech Europe, Belgium.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.