Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Should we shift to Another Technical Paradigm in the Endovascular Exclusion of Complex Thoracic Aortic Aneurysms?
*Corresponding author: Gaetano La Barbera, Vascular Surgery Unit, Department of Cardiovascular disease, Civic Di Cristina Benfratelli Hospital of Palermo, Italy.
Received: February 15, 2021; Published: February 25, 2021
DOI: 10.34297/AJBSR.2021.12.001720
Short Communication
Open surgical and endovascular repair are the current treatments of the atherosclerotic aneurysms and dissections of the aorta. The traditional open surgical repair is burdened with significant postoperative morbidity and mortality rates, while endovascular repair allows comparable results, despite advanced age and increased comorbidity [1]. For this reason, in recent years, the endovascular repair with aortic Stent Graft (SG) progressed significantly, both in hybrid procedures with surgical supraortic debranching [2], and in totally endovascular procedures with fenestrated [3] and branched devices [4]. As a disadvantage, these are complex endovascular techniques that require a high level of expertise and, compared to surgical treatment, are burdened with a higher complication rate during follow-up.
Furthermore, the effectiveness of endovascular repair is conditioned, by both the anatomy of the affected aortic segment and the technical characteristics of the aortic SG. Regarding the anatomy, the aortic arch and the descending aorta can make the treatment complex because the particular anatomic geometry of this aortic segment and the supraortic branches take-off. Regarding the technical characteristics of the aortic SG, to date, there are several different commercial endograft systems for the treatment of the abdominal aorta diseases, but only a few devices have been specifically developped for the treatment of the thoracic aorta. The SG available on the market, for the treatment of the thoracic aorta, are devices similar to those of the abdominal aorta, in structure, in the principle of operation and delivery. Even the custom devices limit their specific design and construction to safeguarding the patency of the supraortic trunks by fenestrations and branches, without taking into account the morphological and hemodynamic characteristics specific to the aortic arch and the releasing techniques for navigating the curved region of the thoracic aorta.
Two years ago, in order to simplify the endovascular repair of the Thoraco-Abdominal Aortic Aneurysms (TAAA), it appeared on the market a new custom-made SG platform, the Dominus (Braile Biomedica®, São José do Rio Preto, Brasil on the design of Endovsmart s.r.l.™, Bergamo, Italy), that relies on three principles: 1) the rigorous engineering customization of the SG, 2) the modulation of the radial force by a new stent and fabric design and, 3) a new concept of fenestration that allows the patency of the supraortic branches reducing the need for surgical debranching or a branched or fenestrated SG [5]. The peculiar engineering customization technique follows millimeter by millimeter the anatomy of the aorta, in order to adapt the SG to the specific anatomic features of the arterial wall. The nitinol stents of the metal scaffold and the Dacron fabric are designed and sutured in all shapes and sizes to modulate the radial force for effective anchoring and sealing, allowing for uncovered areas of the stent graft that ensure patency of the take-off of the supraortic branches [Figure 1].
The preliminary experience with Dominus Braile SG, on complex TAAA, considered unfit for endo-repair, and refused by current manufacturers, has recently been published [6]. Figure 2 shows a TAAA, 6,5 cm in diameter, in a patient treated 12 years before by EVAR and surgical repair of ascending aorta aneurysm. Because the complex anatomy, this patient was rejected by the current producer of custom-made SG. The preoperative angio-CT shoved a dissecting type I thoracic aneurysm with a significant aortic size discrepancy, involving the aortic arch. There was a 5 cm aneurysm of the left subclavian artery [Figure 2a] that was excluded by ligation and a left carotid-subclavian bypass. To obtain an efficient anchoring and sealing, the proximal landing zone was moved to the level of the aortic arch. The proximal SG was 36x44x215 mm in size, with a 122° fenestration for both brachio-cephalic trunk and left common carotid artery.
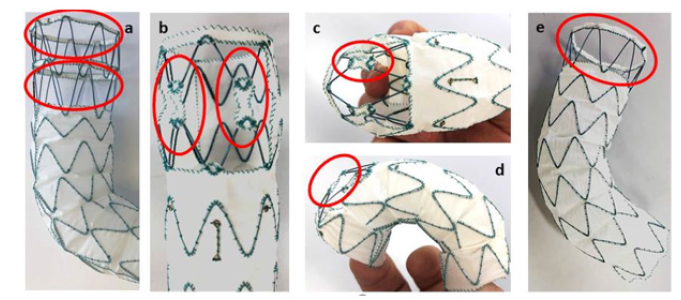
Figure 1: a) Superior oval ring: interconnexion of the apexes of the free-flow with a 3 mm Dacron collar fabric; inferior oval ring: 360° fenestration for left subclavian; b) oval rings: frontal view of the inter-stents connecting Dacron patch at the level of a 122° fenestration; c) oval ring: superior view of the inter-stents connecting Dacron patch at the level of a 122° fenestration; d) oval ring: lateral view of the inter-stents connecting Dacron patch at the level of a 122° fenestration; e) oval ring: : interconnexion of the apexes of the free-flow with a thin Dacron collar textile.
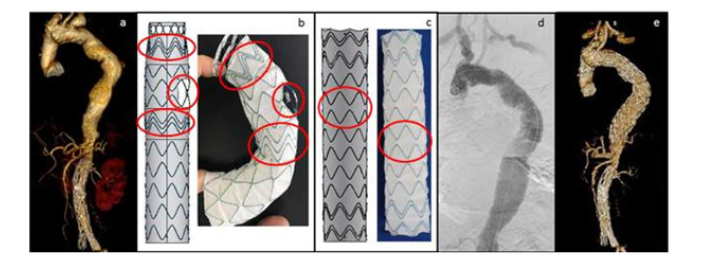
Figure 2: a) dissecting type I TAAA, involving the aortic arch with a 5 cm aneurysm of the left subclavian artery; b) Proximal SG. Technical drawing on the left and SG model on the right: oval rings: triple stent proximally and distally the fenestration for higher radial force; round ring: 122° fenestration for both brachiocephalic trunk and left common carotid artery; c) Distal SG. Technical drawing on the left and SG model on the right: oval rings: peak-to-peak stent configuration for higher support; d) final arteriography: absence of any leak, with good perfusion of the brachiocephalic trunk, left common carotid artery and carotid-subclavian bypass; e) 6 months postoperative 3D-view: effective conformation of the ASG at the level of the aortic arch, correct alignment of the 122° fenestration with the brachio-cephalic and left common carotid artery take-off.
This SG was engineered with a triple stent proximally and distally the fenestration for higher radial force and more efficient anchoring and sealing [Figure 2b]. The distal landing zone was 1 cm above the coeliac trunk. The distal SG was 48x44x220 mm in size, with peak-to-peak stent configuration for more support [Figure 2c]. Postoperative result is shown in Figure 2d. The 3-month postoperative computed tomography angiography confirmed the effective results in terms of ASG conformation and sealingat the level of the aortic arch, absence of the Bird-Beack sign, alignment of the fenestration with the brachiocephalic trunk and left common carotid artery and patency of the supraortic branches [Figure 2e].
Conclusions
In this last decade, the less invasive endovascular approachs with aortic SGs has progressed significantly, but there is not yet in the market the ideal SG able to negotiate any different anatomical morphology. Furthermore, the treatment of the thoracic aorta is challenging due to the presence of the curvature of the aorticarch, the detachment of the supraortic branches and the forces of migration due to blood pressure and aortic movement transmitted by the heart pump. The SGs present on the market for the treatment of the thoracic aorta have the same structure of the abdominal aorta devices and do not take into account the unique morphological, hemodynamic and structural characteristics of the thoracic aorta.
If we want to expand the effective use of endovascular procedures in the treatment of complex atherosclerotic diseases of the thoracic aorta, we probably have to change our mind by thinking about a new idea of SG. The peculiar suggestive construction method of the Dominus (Braile Biomedica®) SG, allows to design the SG according to any change of the anatomy of the aorta. The typical fenestrations, variable in size, and the possibility to modulate the radial force, make this SG able to extend more proximally and distally the landing zone for an effective anchoring and sealing, assuring in the same time the patency of the supraortic branches. Current clinical experience is still based on a few cases. More patients need to be enrolled. A registry is recommended for objective analysis of results.
Conflict of interest
The authors declare the following potential conflicts of interest with respect to the research, authorship, and/or publication of this short communication: the corresponding author Gaetano La Barbera is proctor for Endovsmart s.r.l.
References
- De Rango P, Ferrer C, Coscarella C, Musumeci F, Verzini F, et al. (2015) Contemporary comparison of aortic arch repair by endovascular and open surgical reconstructions. J Vasc Surg 61(2): 339-346.
- Damrauer SM, Fairman RM (2015) Visceral Debranching for the Treatment of Thoracoabdominal Aortic Aneurysms. AORTA 3(2): 67-74.
- Tsilimparis N, Law Y, Rohlffs F, Spanos K, Debus ES, et al. (2020) Fenestrated endovascular repair for disease involving the aortic arch. J Vasc Surg 71(5): 1464-1471.
- Spear R, Haulon S, Ohki T, Tsilimparis N, Kanaoka Y, et al. (2016) Editor’s choice – Subsequent results for arch aneurysm repair with inner branched endografts. Eur J Vasc Endovasc Surg 51(3): 380-385.
- G La Barbera (2018) 8th International Congress. Aortic surgery peripheral and venous. How to do it. Milan, Italy.
- Talarico F, La Barbera G, Valentino F, Filippone G, Ferro G, et al. (2020) A new technical solution in custom- made aortic stent-graft for complex aortic aneurysms. J Vasc Endovasc Ther 5(6): Pp 35.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.