Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Compound Heterozygous HBB: C.79G>A Associated with HBB: C.-78A>G Mutation of HBB Gene Leading to Β-Thalassemia Intermedia in A Vietnamese Patient: A Case Study
*Corresponding author: Tien Anh Ngo, Vinmec Tissue Bank, Vinmec Health Care System, Vietnam.
Lý Thị Thanh Hà, Department of Medical Genetic, Vinmec Health Care System, Vietnam.
Received: May 31, 2021; Published: June 10, 2021
DOI: 10.34297/AJBSR.2021.13.001842
Abstract
β-thalassemia is an inherited blood disorder that is the most common single-gene disorder worldwide and in Vietnam. This study reports an intermedia β thalassemia patient in a family from Northern Vietnam. The mother has compound heterozygous thalassemia presenting mutation of hemoglobin HBB: c.79G>A associated with HBB: c.-78A>G. The result indicates that the determination of molecular characterization of subjects presenting normal HbA2 level associated with abnormal red cell indices is needed for accurate diagnosis and improved genetic counseling.
Keywords: β-thalassemia intermediate, HBB: c.79G>A, HBB: c.-78A>G
Abbreviations: Hb: Hemoglobin; MCH: Mean Corpuscular Hemoglobin; MCV: Mean Corpuscular Volume; RBC: Red blood cell count
Introduction
Thalassemia is an inherited disorder of autosomal disorders with a carrier prevalence of 5% globally [1]. This disorder is the primary cause of hemolytic anemia worldwide, especially in Southeast Asian countries, including Vietnam. There are two main types of thalassemia, including α-thalassemia (causing by mutations in α-globin gene) and β-thalassemia (causing by mutations in β-globin gene). Clinical severity forms the basis of β-thalassemia classification, as follows:
a) β-thalassemia major, the severest type of β-thalassemia,
with patients suffering from severe anemia and transfusion
dependency,
b) β-thalassemia intermedia, sporadic or no transfusions are
required for anemia,
c) β-thalassemia minor, called β-thalassemia trait, this form is
usually asymptomatic [2]. This study will focus on the case
of β-thalassemia intermedia without blood transfusion from
childhood to the present time.
Materials and Methods
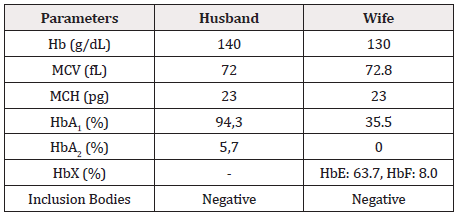
An unrelated couple in the Vietnamese Kinh group was admitted to the Human Genetics Department, National Children’s Hospital, for genetic counseling for thalassemia. They have two children who have been identified as β-thalassemia major who need treatment and regular blood transfusions. Based on laboratory findings, including complete blood count and hemoglobin electrophoresis (Table 1), this couple is highly likely to be β-thalassemia carriers. DNA testing for mutations in the Hbb gene is indicated for both husband and wife to confirm the diagnosis. They are assigned to test for 09 common mutations in the β-globin gene including: -28 [A>G], codon 17 [A>T], codon 26 [G>A] HbE, IVS 1.1 [G>T], IVS 1.5 [G>C], codon 41/42 [-TTCT], codon 71/72 [+A], codon 95 [+A], IVS 2.654 [C>T] by multiplex ARMS PCR. Sanger sequencing was then performed to confirm. According to the manufacturer, amplification products generated by PCR were purified using PureLink™ PCR Purification Kit (Invitrogen) and were cycle sequenced using Big Dye v3.1 reagents (Applied Biosystems) protocol. Sequencing products were purified with BigDye XTerminator™ Purification Kit (Applied Biosystems) and automated sequencing performed by capillary electrophoresis on an ABI3500Dx (Applied Biosystems). Sequences were aligned and examined by using Chromas Pro software (Technelysium Pty Ltd).
Results and Discussion
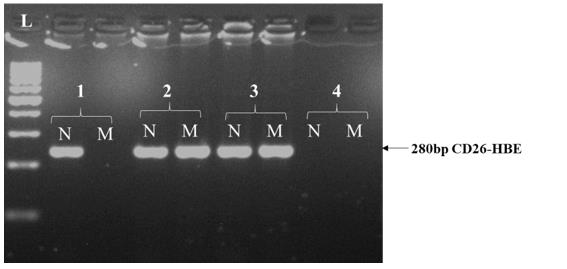
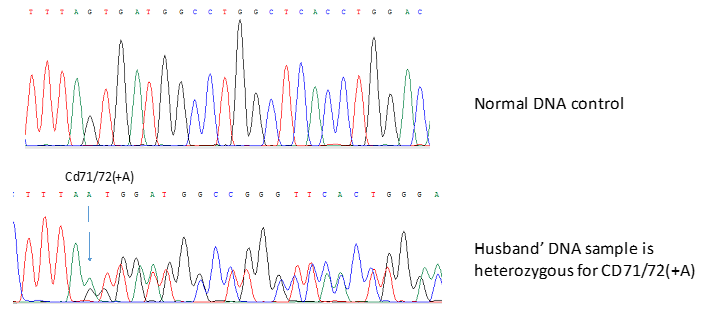
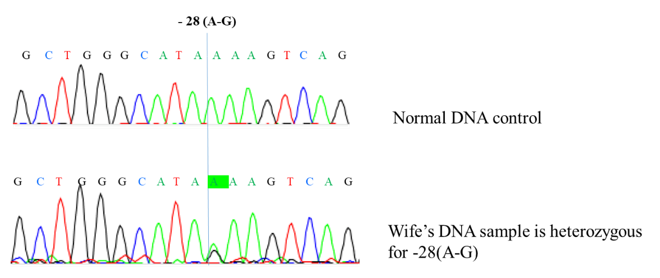
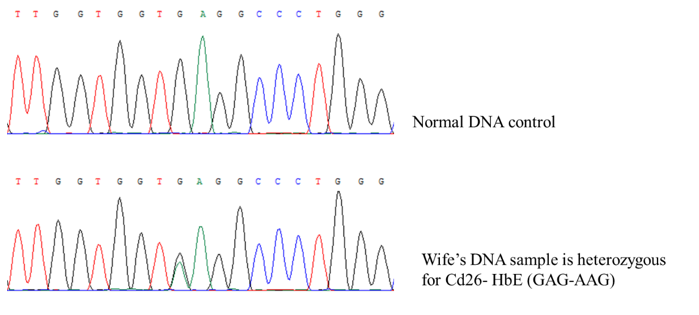
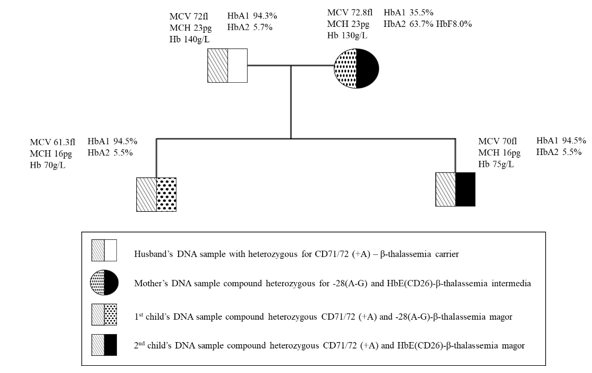
Nine common mutations in the Vietnamese population were screening for both the husband and wife. Multiplex ARMS-PCR result shows that the husband has codon 71/72 [+A] (Figure 1). The wife has never had a blood transfusion up to now. However, the genetic screening results clearly show that she has compound heterozygous for 28 [A>G] and codon 26 [G>A] HbE (Figure 2 & 3). These results were confirmed by Sanger sequencing (Figure 4-6). In general, β-thalassemia intermedia encompasses a broad clinical spectrum with more severe cases presenting between 2 and 6 years of age, including anemia, spleen, and sometimes liver enlargement, as well as delayed growth and development [3]. In other cases, patients are entirely asymptomatic until adult life with only mild anemia [4]. Because the clinical manifestations are not significant, the screening and diagnosis of patients with β-thalassemia intermedia are easy to miss. If only based on the initial screening results of the complete blood count, it is easy to make indecision that this patient is a β-thalassemia carrier. Particularly, if based on the hemoglobin electrophoresis analysis with the high level of HbF (8%), it recommends differential diagnosis. After finding the mutation of the father and the mother, we continued to find the mutant genotype of their children. The β-globin mutation was found in their children (Figure 7). This result shows that two children in this family both have β-thalassemia major. Importantly, they have two different genotypes because the mother is a compound heterozygous of two mutations.
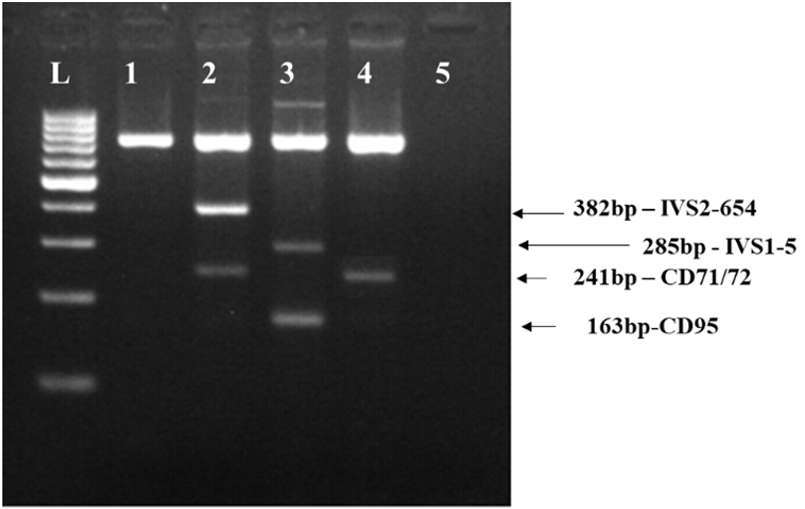
Figure 1: Gel electrophoresis analysis of CD71/72 (+A) mutation in the patient’s husband by multiplex ARMS PCR.
Lane L: Ladder 100bp.
lane 1: Negative control.
lane 2: Internal control with IVS2-654(C-T) and CD71/72 (+A) mutant
lane 3: Internal control with IVS1-5 (G-C) and CD95 (+A);
lane 4: Husband’s DNA sample.
lane 5: Blank control.
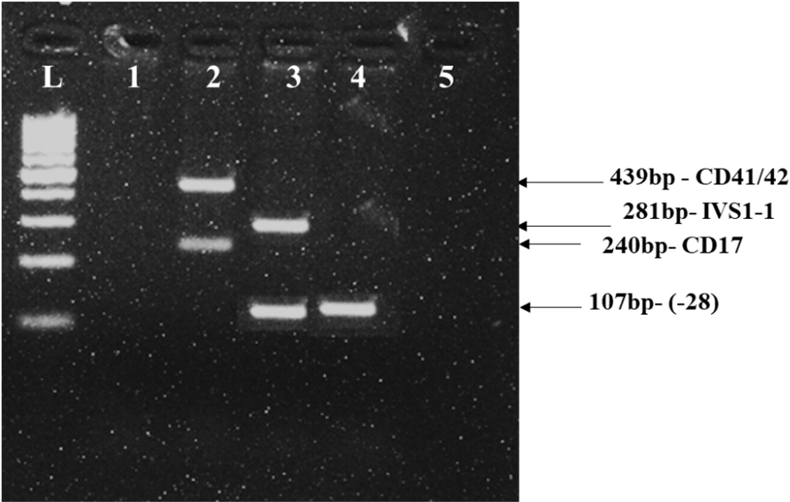
Figure 2: Gel electrophoresis analysis of -28 (A-G) mutation in the patient’s wife by multiplex ARMS PCR. Lane L: Ladder 100bp
lane 1: Negative control.
lane 2: Internal control with CD41/42 (-TCTT) and CD17 (A-T) mutant.
lane 3: Internal control with IVS1-1 (G-T) and -28 (A-G).
lane 4: Wife’s DNA sample.
lane 5: Blank control.
Conclusion
Our data highlight the necessity of deep molecular characterization of intermedia thalassemia subjects. This study plays a significant role in genetic counseling, diagnosis, and treatment, especially in prenatal diagnosis for risk families.
Acknowledgments
The authors express our sincere to all staff of the Human Genetics Department - Vietnam National Children’s Hospital, Medical Genetic Department - Vinmec Health Care System, Vietnam, and Vinmec Tissue Bank.
Conflict of Interest
The authors declare no conflicts of interest.
References
- B Modell and M Darlison (2008) Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ 86(6): 480-487.
- V Viprakasit and S Ekwattanakit (2018) Clinical Classification, Screening and Diagnosis for Thalassemia,” Hematol Oncol Clin North Am 32(2): 193-211.
- RM Shawky and TM Kamal (2012) Thalassemia intermedia: An overview Egypt. Egyptian Journal of Medical Human Genetics 13(3): 245-255.
- K Tari, P Valizadeh Ardalan, M Abbaszadehdibavar, A Atashi, A Jalili, et al. (2018) Thalassemia an update: molecular basis, clinical features and treatment. International Journal Biomedicine and Public Health 1(1): 48-58.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.