Opinion 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Diagnosis Errors in Oral Surgery: What Should We Learn from This Medical Error?
*Corresponding author: Akram Belmehdi, Regional Center of Oral Care of Rabat, Kingdom of Morocco.
Received: April 17, 2021; Published: May 27, 2021
DOI: 10.34297/AJBSR.2021.13.001826
Keywords: Medical Errors, Wrongly Diagnosed, Omission, Oral Surgery, Dental Practice, Equipment, Lab Reports, Scientific Evidence, Mucosal Disease
Introduction
Medical errors could happen anywhere and anytime in the health care system: In hospitals, clinics, doctors’ offices, pharmacies, and patients’ homes. Scientific literature indicates that such problems widely involve medicines, lack of current scientific evidence regarding treatment, diagnosis, equipment, or lab reports. Medical errors leading to adverse events can occur in dental practice, and especially in oral surgery. The purpose of this paper is to bring out one aspect of errors in oral surgery: diagnostic errors or failures. This subject is rarely discussed in the world of dentistry with lack of references about it in medical literature. The authors report five clinical cases that were wrongly diagnosed either due to omission of careful preoperative examination, or due to a clinical experience’s deficiency.
Clinical Cases
Case 1
Medically compromised patient: A 60-year-old man referred to our department because of postoperative continuous bleeding after dental extraction of two lower incisors in general private practice. The hemorrhage did not stop for 24 hours (Figure 1). Examination of the patient found that he has mechanical valves and under anticoagulants therapy, with a severely advanced periodontitis. The first dentist did not consider these elements in the management of the patient; the latter confirmed to us that the dentist performed the extractions without preoperative medical check-up. We deduce from the case that preoperative examination of patients can avoid practitioners to harm patients by medical errors related to a misdiagnosis of their health and oral conditions, which will respect ethical, legal, and risk-management considerations.
Case 2
Another aspect of diagnosis error concerns mucosal disease. We report a case of a 57-year-old male patient, with a complaint of a non-healing ulcer on the left posterior oral mucosa. The patient had consulted one month ago, a general dentist who considered the lesion as a dental abscess, without any radiographic examination, and prescribed antibiotics to him. The physical examination was difficult due to painful trismus which was <2½ cm. A single well-defined, ulcero-proliferative lesion could be visualized (Figure 2A). He presented also two left submandibular lymph nodes that was palpable. Orthopantomogram showed a maxillary left posterior bone lysis (Figure 2B). Incisional biopsy revealed a welldifferentiated squamous cell carcinoma. In this case, we notice that the wrong first diagnosis had delayed his management. The first dentist had not provided any effort to make a complete diagnosis, which was clearly related to insufficient knowledge about oral pathology.

Figure 2: (A) Intraoral view of the posterior lesion. The patient could not open widely his mouth.
(B) Orthopantomogram showed a bone loss in the left posterior tuberosity.
Case 3
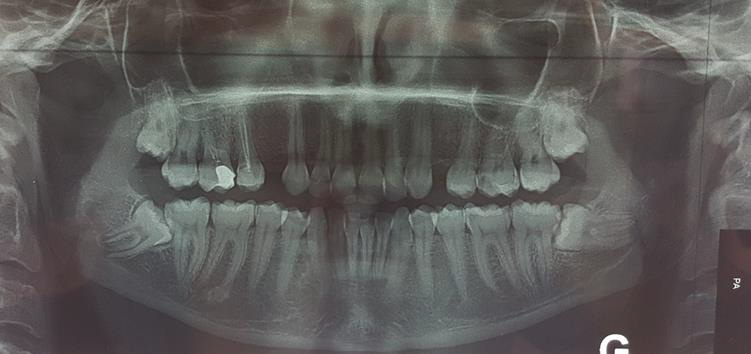
The third case is about a young patient whose reason for consultation was the persistence of a left facial swelling for two months with a severe trismus (Figure 3A). He reported that he visited two different dentists since the first appearance of the swelling. Both considered it as an odontogenic cellulitis and prescribed antibiotics with steroids. Radiographic examination was performed; for the first time in this case, in our hospital, and showed a posterior large mandibular radiolucent lesion in the left side, associated with an impacted third molar (38), in favor of an odontogenic cyst or tumor (Figure 3B). Histologic examination of the lesion revealed an odontogenic keratocyst. This case informs us about two closely related errors: a diagnosis error of an odontogenic cellulitis, without preoperative radiographic examination; following by a useless prescription of medication that complicated clinical symptoms (persistence of the swelling and trismus).

Figure 3: (A) extraoral view of the left posterior swelling.
(B) Orthopantomogram showed a left mandibular radiolucency associated with an impacted third molar.
Case 4
Another misdiagnosed case related to a wrong approach of clinical examination: the patient consulted a dentist because of appearance of an ulcerative cutaneous sinus tract in her left submandibular area (Figure 4A). Ignoring to make a correct diagnosis of her condition, he sent her to a dermatologist since the lesion was in her skin. The dermatologist prescribed only topic medication without any good improvement. The patient was referred to our department. Orthopantomogram showed a presence of radiopaque lesion in the left molar mandibular region (Figure 4B). Biopsy of the lesion had concluded a suppurative osteomyelitis, which was the principal etiology of the cutaneous sinus tract.
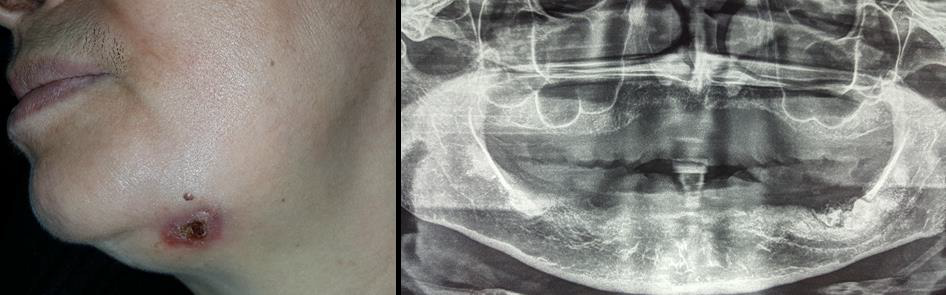
Figure 4: (A) extraoral view submandibular cutaneous sinus tract.
(B) Orthopantomogram showed a left mandibular radiopaque lesion.
Case 5
Sometimes, even with radiological examination, occurrence of failures is inevitable. The last case of our clinical series describes a young female patient who underwent a third molar surgery. She presented Inferior Alveolar Nerve (IAN) paresthesia of a transient nature (two months). Evaluation of her preoperative orthopantomogram showed that roots of mesioangular impacted third molar (48) are in close relation to mandibular canal (Figure 5), which was misdiagnosed and not taken into consideration by her dentist. This paresthesia could be prevented by indicating CBCT-SCAN to confirm real contact between roots and IAN, to avoid the neurological risks, and alternative strategy might be used like coronectomy to reduce postoperative patient’s discomfort.
Discussion and Conclusion
Diagnosis forms the key to treatment planning, which is
important to initiate the appropriate management at the right time.
A diagnosis could be erroneous when the practitioner has lacked
vigilance. Habit, routine, lack of involvement on the part of the
practitioner; or on the contrary; a strong pressure from the patient,
are a common factor that conduct the therapist to make the wrong
diagnosis. In oral surgery and pathology, the conditions most often
related to diagnostic failure are oral infections, cancers, benign
tumors, and other mucosal diseases. Misdiagnosis, another form of
diagnosis error, can also occur in relation to adverse consequences
(e.g., infections, nerve injuries, etc.) resulting from third molar
surgery and implant procedures. Dentists and oral surgeons play
an important role in the early diagnosis and treatment of oral
lesions. Oral care includes not only a complete preoperative clinical
examination associated with radiology to identify the condition,
but also determination of a pathology by biopsy and histologic
evaluation. Nevertheless, treatment based only on a clinical
impression of the diagnosis, without using a scientific approach
of preoperative assessment, can result in serious consequences.
Theoretical knowledge and clinical experience too matter in preventing a mistaken diagnosis. Careful patient management,
teamwork and use of technology can reduce the diagnosis errors.
Learning from mistakes is also important to minimize errors in
future.
In conclusion, avoiding and stopping diagnosis errors could be
Achieved by:
A. Developing collaborations between various specialties of
dentistry.
B. Continuous education and training to update practitioners
with current knowledge and technologies.
C. The need to establish a complete preoperative assessment
including radiographic evaluation and biologic examination.
Acknowledgement
Special acknowledgements and dedication to my brother Mohammad Belmehdi, and to the most worshipful GLNM sovereign community.
Conflicts of Interest
None.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.