Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Uncommon Presentation of Hydradenitis Suppuritiva with Unique Surgical Considerations
*Corresponding author: Zuhair Irfan, Henry Ford Health System, 2333 Biddle Avenue, Wyandotte, Michigan, 48192, USA
Dedication to Professor. Forrest Smith, Harrison School of Pharmacy, Auburn University, Alabama, USA.
Received: June 11, 2021; Published: July 15, 2021
DOI: 10.34297/AJBSR.2021.13.001889
Abstract
Hydradenitis suppurtiva [HS] is an inflammatory skin condition often presenting in the intertrigenous areas of the body, with chronic and recurrent lesions typically treated by wide margin surgical excision. We discuss an uncommon presentation of HS in the popliteal fossa, with unique surgical considerations due to a previous traumatic below knee amputation of the affected side and potential for skin contractures affecting mobility.
Introduction
Hydradenitis suppuritiva is a common inflammatory skin disorder typically presenting with recurrent chronic lesions in apocrine gland-containing skin regions. These pruritic, painful, and suppurative lesions are predominantly present in intertrigenous regions of the body.
There is no cure for HS. Treatment of HS depends on severity of the process. In patients with mild disease processes, lifestyle modifications are encouraged, including warm baths and improved hygiene, decreased weight, and reduction of smoking. Further treatment modalities may focus on combination antibiotic treatment up to 6 months [1]. Anti-inflammatory medications may be employed as well, with usage of both NSAIDs and corticosteroids via topical, oral, or intra-lesional injections [1]. Additionally, further anti-inflammatory, biological, or immunosuppressive therapy may be used [1]. In chronic or uncontrolled HS, wide margin excision is the preferred method of surgical intervention, as implicated in the presented case.
Methods
A 46-year-old man [JT] with a past medical history of hyperlipidemia, coronary artery disease with LAD stenting, as well as a surgical history of right sided traumatic below knee amputation [BKA], was evaluated in the plastic surgery clinic with complaints of skin irritation and thick, creamy drainage from behind the right knee that was inhibiting the patient’s ability to effectively wear his prosthesis. Patient endorsed a 1 PPD history of smoking for 25 years.
Physical exam revealed a right-sided BKA without significant contracture. The popliteal fossa demonstrated multiple areas of transversely oriented skin pitting with fibrotic non-draining clefts as well as dermal and superficial subcutaneous tissue induration consistent with HS (Figure 1). No active infection was appreciated.
Conservative and surgical treatment modalities were discussed in detail with patient. The patient elected for surgical intervention, as explained by the surgeon to attempt complete excision and combining this with primary closure in multiple directional vectors incorporating skin plasties to limit the chance for profound hypertrophic scarring given the location and lifelong trauma from his below knee prosthetic. Patient provided informed written consent and was boarded for surgery.
Procedure
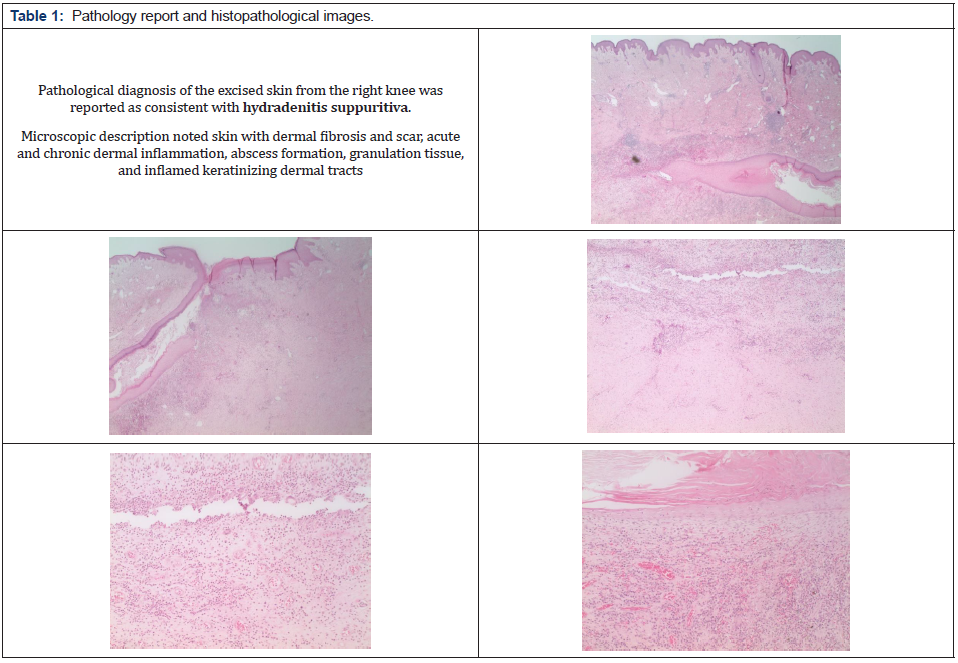
There was no fluctuance or erythema at the time of surgery. Resection was performed utilizing cutting current electrocautery into the superficial subcutaneous tissues. There was mild induration in the very superficial subcutaneous tissue plane and mild to moderate induration within the skin. There were no pockets of fluid and no gross evidence of infection. Resection size in the central portion of the popliteal fossa was 7x7 cm. Two additional sites were excised, one 3x1.5 cm and the other approximately 4x2 cm. All were sent to Pathology for permanent section analysis and findings were confirmed as below (Table 1). Meticulous hemostasis was obtained throughout the procedure using directed electrocautery. A 1cm to 1.5cm circumferential subcutaneous tissue undermining was performed of the smaller resection areas to allow for a 4cm and 5cm complex wound closure, respectively. This was accomplished after the wounds were irrigated with sterile saline, utilizing interrupted buried 2-0 and 3-0 PDS sutures for the deep dermis and 2-0 and 3-0 nylon sutures for the epidermis. Given the size of the central resection and the patient’s baseline of approximately 5 degrees of knee contracture, decision was made not to attempt closure with a linear popliteal fossa crossing scar in order to avoid any further augmentation of his knee contracture. Rather, a distally-based V-Y fasciocutaneous advancement flap was designed measuring a total of 20 sq. cm. This was advanced on the underlying attached fascia and adipose tissue mobilizing it approximately 3 cm into the defect (Figure 2, 3). The proximal portion of the defect was minimally undermined as well. Wound closure was performed with inset of the V-Y advancement flap using interrupted 2-0 and 3-0 PDS sutures for the deep dermis as well as closure of the Y component, and 2-0 nylon sutures for the epidermis (Figure 4). There was minimal tension on the tissues and healthy bright red bleeding from all dermal edges was noted during inset. There was no evidence of venous congestion. All wounds were closed and dressed with a sterile dressing.
The patient progressed well in the post-operative period with stitches being removed approximately 2 weeks after the procedure. Physical exam revealed continued and complete viability of the flap on follow ups, and the patient did not report any significant complications. He was cleared to progress with adjustment of his prosthesis and was discharged with follow up as necessary.
Discussion
Hydradenitis suppuritiva is a chronic inflammatory and suppurative condition most commonly observed within the axillae, inframammary regions, groin, genital, and gluteal areas [2]. Patients with this disease may experience recurrent abscesses, draining sinuses, and scarring, affecting principally areas of body friction [3]. While the etiology of this disabling disease is not completely understood, it involves follicular occlusion of the apocrine glands as a primary event followed by secondary bacterial infection [4]. Current literature supports that this disease may be defined as a systemic inflammatory condition with several associated metabolic conditions including obesity; additionally, autoimmune diseases such as inflammatory bowel diseases, autoinflammatory diseases, spondyloarthritis, some genetic keratin disorders, occur more frequently in these patients [5]. HS is more common in women than men [75% vs 25%] [4]. Data also demonstrates a link between BMI and disease severity, as 76% of HS patients were obese [4]. Prevalence of HS is approximately 1% and incidence peaks in the second and third decades and declines by the fifth decade [5].
Grading of HS is based on the Hurley classification system. In this system, Stage 1 includes abscess formation, whether single or multiple, with no sinus tracts or scarring [5]. Stage 2 involves recurrent single or multiple abscesses with sinus tracts and scarring [5]. Stage 3 is classified as diffuse or almost diffuse involvement of multiple interconnected tracts and abscesses [5]. There is unfortunately no cure for HS. However, treatments are available and are largely based on the stage of disease. Treatment options for mild to moderate disease include oral antibiotics, topical antibiotics, intralesional steroid injections, laser treatments, minor surgery, and hormonal therapy [6,7]. Disease of greater severity may also be treated with these modalities, however they are more likely to be refractory, requiring additional treatments such as biologic agents, immunosuppression, and larger surgical procedures [6,7]. Additionally, patients are encouraged to quit smoking, maintain a healthy body weight, and wear looser-fitting clothing [6].
Patients with HS often suffer from the negative social and emotional effects secondary to this disease. Because of the associated anxiety and stigma, patients may experience social isolation, anxiety, and depression [5]. With respect to our patient, review of the literature revealed limited discussion on presentation of HS within the popliteal fossa. However, the clinical presentation was consistent with HS, likely secondary to obesity, mechanical irritation, and occlusion. With surgical intervention, we encourage practitioners to weigh the risks/benefits of wide margin surgical excision while determining the best technique for each patient, particularly those at risk for hypertrophic scar formation, at risk individuals for keloid development, and in our case, excessive scarring leading to potential contractures in sensitive areas such as a below knee amputation and prosthetic site. Adding the negative social and emotional stigmata of HS to our patient’s existing challenges associated with reliance on a prosthetic limb emphasized the importance of careful surgical planning, so as not to reduce function and mobility. Patient reports no issues with contracture or his ability to use his prosthetic, which we attribute to proper surgical decision making and patient compliance [8].
Acknowledgements
The authors would like to thank Dr. Jason Pimentel in the Department of Pathology and Laboratory Medicine at Henry Ford West Bloomfield Hospital for the histopathological visuals and comprehensive pathology report.
Disclosures
None of the authors has a financial interest in any
References
- Saunte DML, Jemec GBE (2017) Hidradenitis Suppurativa: Advances in Diagnosis and Treatment. JAMA 318(20): 2019–2032.
- Patil S, Apurwa A, Nadkarni N, Agarwal S, Chaudhari P, et al. (2018) Hidradenitis Suppurativa: Inside and Out. Indian J Dermatol 63(2): 91-98.
- Pescitelli L, Ricceri F, Prignano F (2018) Hidradenitis suppurativa and associated diseases. G Ital Dermatol Venereol 153(3 Suppl 2): 8-17.
- Kurayev A, Ashkar H, Saraiya A, Gottlieb AB (2016) Hidradenitis Suppurativa: Review of the Pathogenesis and Treatment. J Drugs Dermatol 15(8): 1017-1022.
- Vekic DA, Cains GD (2017) Hidradenitis suppurativa - Management, comorbidities and monitoring. Aust Fam Physician 46(8): 584-588.
- Alikhan A (2016) Hidradenitis Suppurativa. JAMA Dermatol 152(6): 736.
- Lee EY, Alhusayen R, Lansang P, Shear N, Yeung J (2017) What is hidradenitis suppurativa? Can Fam Physician 63(2): 114-120.
- World Union of Wound Healing Societies (2016) Understanding Hidradenitis Suppurativa.







 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.