Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
“Update to Pseudobulbar affect (suddenly emotions of crying/laughing without control)”
*Corresponding author: Jorge Garza-Ulloa, Research Consulting Services www.garzaulloa.org / University of Texas El Paso, US.
Received: May 31, 2021; Published: June 09, 2021
DOI: 10.34297/AJBSR.2021.13.001837
Abstract
An “suddenly emotional” is when the simplest things like a simple comment or opinion of someone, a song, a memory, a TV commercial, a harsh word, or even a wayward perception, is all it takes for a person to be drowning in tears, or switch to an exaggerated laughing. These could be an indication of somebody could have “Pseudobulbar affect”, this is a is a disorder that is characterized by episodes of sudden uncontrollable inappropriate laughing and/or crying. “Pseudobulbar affect” typically occurs in people with certain neurological conditions as brain disorders or injuries, which might affect the way the brain controls emotion. The “Pseudobulbar affect (PBA)” are emotions that leaves as fast as they come, making the affected person embarrassed when they spoke publicly, and they start crying or laughing. “PBA” is not really their fault, they have episodes that they cannot control, and they are not alone in this world, where millions of people with affected neurologic conditions have symptoms that may suggest the emotional disorders known as “Pseudobulbar affect”. In this paper the goal is introduce you this disorder, explain the latest updates of how suddenly emotions of crying/laughing without control may suggest “Pseudobulbar affect”, and point out the importance of document this kind of episodes of people that preset this behavior by ones around them, as : caregiver, their loved one, healthcare provider at palliative or hospice health care, all of this with the purpose to facilitate their analysis of the complexity of the symptoms that frequently are combined with neurological condition or brain injuries different by specialized doctors as neuropsychologist, neurologist, and psychiatrist to obtain a valid diagnostic in the less possible time to improve the quality of life of affected persons.
Keywords: Pseudobulbar affect, brain injury, Parkinson’s disease, Parkinsonism, Parkinson’s, Amyotrophic Lateral Sclerosis, Alzheimer dementia, Traumatic Brain Injury, Cerebrovascular disease, Multiple Sclerosis.
Abbreviation: (PBA): Pseudobulbar affect; (PD): Parkinson’s disease; (CNS): central nervous system; (ALS): Amyotrophic Lateral Sclerosis; (ALZ): Alzheimer dementia; (TBI): Traumatic Brain Injury; (MS): Multiple Sclerosis; (CNS): central nervous system.
“suddenly emotions of crying/laughing without control” dedicated to my mom by Jeannie
Introduction based on affected people comments and reports
“Pseudobulbar affect” was first defined as a syndrome based
on several symptoms occurring together and characterizing for
specific disorders, that identifies irregularity or interruption of
normal emotional functions expressed as crying and/or laughing
without control. “Pseudobulbar affect abbreviated as PBA” typically
occurs in people with certain neurological conditions or brain
injuries, which might affect the way the brain controls emotions.
This condition might interfere with abilities to work and do daily
tasks, especially when already the affected one is handling other
symptoms from neurologic conditions or brain injuries. Usually
“PBA” causes embarrassment, social isolation, stress, anxiety, sleepdisorders and even depression for affected patients.
Many millions of affected people around the world report
symptoms that may suggest “Pseudobulbar affect” without being
aware of their current neurologic condition or brain injuries. They
frequently report with comments like the following:
• “My emotions leave me as fast as they come. They are not real
or mine like they used to be.”
• “I cry now a lot; I have never been a crier...all the time.”
• “Sometimes when I have spoken publicly, I will start crying or
laughing. Very embarrassing!! I therefore don’t do any public
speaking anymore”.
• “I cry frequently at TV commercials, and I cannot stop for
minutes.”
• “I wait till everyone is out of the movie, so i can go out without
people seeing my tears. I feel silly.”
• “My eyes used to become tearful on any sad news or situation.
I did not think at all that this may be due to underline
depression.”
And more many similar reports of episodes of sudden
uncontrollable and inappropriate laughing or crying at inconvenient
moments.
“Caregivers and their loved one of people with neurological
condition or brain injuries” also report their experiences as a wide
feeling when receive suddenly changing emotions from the patients
all days long as:
• “Guilty about no knowing how to help them”,
• “Confused and helpless wondering where the crying or
laughing are coming from”,
• “Sadness at seeing their patients struggling with sudden
emotion that impact their quality of life”.
• And many similar reports
“Healthcare provider at palliative or hospice health care
providers” frequently are challenged to make a diagnosis and
treatment plan with lack of education on “pseudobulbar affect
(PBA)”, leading them to ineffective treatments based on wrong
clinicals impressions identifying the causes as: “stress”, “pain”,
“anxiety”, sleep disorders”, “depression”, “bipolar disorder” and
many others. Where:
• “Stress” defined as a physical, mental, or emotional factor that
causes bodily or mental tension. It can be external from the
environment, psychological, or social situations or internal
based on illness, a medical procedure, pain, etc. [1,2].
• “Pain” is defined as physical suffering or discomfort caused by
illness or injury [3]
• “Anxiety” as an emotion characterized by physical manifestation
of stress, worried thoughts that lead to excessive nervousness,
fear, apprehension, and inclusive physical symptoms changes as
increased blood pressure and others that may seriously affect
day-to-day living [1], “anxiety” is a common manifestation in
depressive states of the affective disorders [4]
• “Sleep disorders” are frequently initiated with “sleep changes
patterns” due to a big diversity of reasons as: “stress”, “anxiety”,
aging, hormonal levels changes, mood, sleep apnea, snoring,
lifestyles, environment changes, restless leg syndrome [43],
and many other reasons. “Sleep” is defined as the normal
condition of body and mind such as that which typically recurs
for several hours every night, in which the nervous system
is relatively inactive, the eyes closed, the postural muscles
relaxed with consciousness practically suspended and the
normal “Sleep stages”, which is duration is different at various
age [1]. All of this based on changes in sleep patterns in older
men have been linked to an increased risk of cognitive decline
[5]. Until recently, both the purpose of the biological need
for sleep and the mechanism by which the “central nervous
system (CNS)” eliminated metabolic waste products were
unknown. The “glymphatic system” is the recently discovered
macroscopic waste clearance system for the “CNS”, because it
rushes along right next to the brain’s blood vessels, delivering
key supplies while clearing away unwanted debris. It which
predominantly functions during sleep states [6]
• “Depression” as is a constant feeling of sadness and loss
of interest, which stops you doing your normal activities.
Different types of “depression” exist, with symptoms ranging
from relatively minor to severe. Generally, depression does not
result from a single event, but from a mix of events and factors
[7]. For example: “Surviving cardiac arrest” is characterized
by cognitive, psychological, and functional impairments and
apprehension over long-term prognosis. A first estimated the
proportion of clinically significant depression and anxiety in
cardiac arrest survivors and their informal caregivers is bigger
than previous thought [8].
• “Bipolar disorder” formerly called “manic-depressive illness or
manic depression” is defined as a mental disorder that causes
unusual shifts in mood, energy, activity levels, concentration,
and the ability to carry out day-to-day tasks [9]. “Bipolar
disorder” is associated with increased rates of separate
physical diseases likely involving inflammatory components
in the pathogenesis including ischemic heart disease,
diabetes, dementia, hypertension, hypercholesterolemia and
hyperlipidemia, hypothyroidism, and infections [10].
• And others clinicals impressions based of the intense emotions
experienced by “Pseudobulbar affect”, taking them to take
wrong decisions to health care provider at palliative or hospice health care providers, caregivers and their loved one can easily
misjudged when they try to help their patients. Although an
estimated 9% of nursing home residents have symptoms
suggestive of PBA, they are not routinely screened [11].
Pseudobulbar Affect (PBA) Best Definition
Charles Darwin since 1872 described about “involuntary
laughing and crying as pseudobulbar palsy patients” [12], and
Oppenheim in 1911 [13] was the first to use the term “pseudobulbar
affect”, and Wilson in 1924 [14] defined “Pseudobulbar affect
(PSA) as a stereotype emotional display with characteristically
uncontrollable, involuntary outburst of laughing or crying that
mimic an emotional expression that does not reflect the actual
appropriate mood status of the patient”.
Actually, “Pseudobulbar affect” is identified as:
a) “PBA or pathologic laughing/crying is defined as a disorder
based on the disturb of normal function for emotional
expressions, and not only as a syndrome based on collection of
signs and symptoms”.
b) “PBA is distinguishable from mood disorders in which
emotional expressions are associated with actual mood or
feelings” [15].
c) “PBA” is a disorder of emotional expression rather than a
primary disturbance of feeling, that can cause a significant
burden of illness in patients already impacted by a serious
neurologic disease, including impairments in overall health
status” [16]
Because “PBA” symptoms always happen when certain
“neurologic conditions or brain injuries” exist, it is recommended
to be treated only by a specialist doctor who can diagnose
“pseudobulbar affect identified (PBA)” as neuropsychologist,
neurologist, and psychiatrist. It is often detected by theses
expert clinicians in an informal manner, as a part of their routine
neurological evaluations. The most frequently neurological
diseases that could include “PBA” are: “Amyotrophic Lateral
Sclerosis”, “Alzheimer dementia”, “Traumatic Brain Injury (TBI)”,
“Cerebrovascular disease”, “Multiple Sclerosis”, “Parkinsonism”,
“Parkinson’s Disease (PD)”, and others. Where:
a) “Amyotrophic Lateral Sclerosis (ALS)” is a progressive nervous
system disease that affects nerve cells in the brain and spinal
cord, causing loss of muscle control. “ALS” is often called “Lou
Gehrig’s disease”, after the baseball player who was diagnosed
with it. Doctors usually do not know why “ALS occurs” but
some cases are inherited [17].
b) “Alzheimer dementia” is a progressive neurodegenerative
disease that occurs when nerve cells in the brain die, where
dementia symptoms gradually worsen over several years.
In its early stages, memory loss is mild, but with late stage
“Alzheimer’s”, individuals lose the ability to carry on a
conversation and respond to their environment. “Alzheimer’s”
is the most common cause of dementia [18], where “dementia”
is defined as a loss of mental skills, such as memory, cognition,
problem solving, and learning severe enough to interference
with daily life. There are many kinds of dementia and “PBA”
could be present in many of them [19]
c) “Traumatic Brain Injury (TBI)” usually results from a violent
blow or jolt to the head or body. An object that goes through
brain tissue, such as a bullet or shattered piece of skull, often
occurs because of a severe sports injury or car accident. “Mild
traumatic brain injury” may affect your brain cells temporarily.
More “serious traumatic brain injury” can result in bruising,
torn tissues, bleeding, and other physical damage to the brain.
These injuries can result in long-term complications or death
[20,21].
d) “Cerebrovascular disease” refers to a group of conditions,
diseases, and disorders that affect the blood vessels and
blood supply to the brain. If a blockage, malformation, or
hemorrhage prevents the brain cells from getting enough
oxygen, brain damage can result. “Cerebrovascular diseases”
include “stroke”, “transient ischemic attack (TIA)”, “aneurysm”,
and “vascular malformation” [22].
e) “Multiple Sclerosis (MS)” is a potentially disabling neurological
progressive disease of the “brain and spinal cord (central
nervous system)”. Where, the immune system attacks the
protective sheath (myelin) that covers nerve fibers and causes
communication problems between your brain and the rest of
your body [23,24].
f) “Parkinsonism” is a constellation of signs and symptoms that
are characteristically observed in “Parkinson’s disease (PD)”,
but that are not necessarily due to PD [25,26].
g) “Parkinson’s Disease (PD)” is a progressive neurodegenerative
disease producing neuronal cell death, presenting loss of
dopamine production in the brain area known as “substancia
nigra”, altering the “central nervous system CNS” formed
by brain and spinal cord, and affecting the regulation of the
human movements and emotions [27,28]
And others neurological diseases that could or could not
include “PBA” disorder.
Pseudobulbar Affect Must be Evaluated by Neurological Disorders Specialists
The neurologist Dr. Klaus Poeck in 1969 [29] defined the basic 4 criteria for detection of “PSA” as:
1) When the emotional response is situationally inappropriate, |
|---|
Then, Dr. Jeffrey L. Cummings et al. in 2006 [30] defined 6 criteria for detection of “PBA” as:
|
1) Changes from previous emotional responses, |
|---|
The most frequently PBA diagnostic criteria are from [30,31]: “The Center for Neurologic Study-Liability Scale (CNS-LS) and the Pathologic Laughter and Crying Scale (PLACS)”. Where:
• The Center for Neurologic Study-Liability Scale (CNS-LS) [32] is a short 7-item, self-administered questionnaire designed to be completed by the patient, that provides a quantitative measure of the perceived frequency of PBA episodes. Add the values for each of the 7 items to get the total score evaluating the answer with the following 5 options: Never= 1 point, Rarely=2 points, Occasionally=3 points, Frequently=4 and Most of the time=5 points. “A CNS-LS score of 13 or higher may suggest PBA*”. The CNS-LS can help accurately diagnose PBA. The CNS-LS 7 items used for autoevaluations; these are:
|
I. If there are times when I feel fine one minute, and then I will become tearful the next over something small or for no reason at
all. |
|---|
• “The Center for Neurologic Study-Liability Scale (CNS-LS) and the Pathologic Laughter and Crying Scale (PLACS) [33] have a more precise test than consists of 18 questions and must be carried out by a health professional*. Scores for each question range from zero (normal) to three (excessive emotional lability). It looks at several aspects of “PBA” including duration of, and the extent of distress following, an episode. This scale has not been validated in people with “Multiple Sclerosis (MS)”, but it has been used in “MS studies of PBA”. A score of 13 or more would indicate presence of “PBA”.
Note*: It is important to get a prompt and accurate diagnosis of “pseudobulbar affect” by specialist doctors as neuropsychologist, neurologist, and psychiatrist to enable you to access appropriate treatment, as well as support for you and your family. Counselling may be helpful to reassure the patient and their families that “PBA is not the fault of the patient”.
Pseudobulbar Affect Differences with Depression
Because “PBA” patient’s emotional response is noted as
disproportionate and, therefore, overlooked as “depression”, or
changes are attributed to the patient’s baseline neurocognitive
disease. Often, patients are misdiagnosed as having “depressed
mood”. Based on different research report [31-34,13]:
• In average from 30% to 35% of patients with “PBA” are
“depressed”.
• “The duration and type of symptoms can help delineate
depression from PBA”.
• “Depression tends to have a longer clinical course, whereas
PBA is often of a brief nature with episodic occurrences”.
• “The exaggerated response of patients with PBA, as well as the
discordant response, is also exclusive to PBA”.
• Neurovegetative symptoms such as sleep, and appetite
disturbances are relegated to “depression” and are not
associated with “PBA” It is very import to mention the “PBA”
appears to be related with the “Theory of Stress-Anxietysleep
disorders -Neural Damage Chain in neurological
diseases and brain damage” [1] as explained in this research
article with concepts involved, many reasons to be included
in the theory and their relations to previous conclusions/
suggestions of many researchers’ papers already publish,
and recommendations to develop good habits in neurological
patients to minimize the “PBA” disorder as explain in a real case
in section of this research: “section 8 Testimony to diagnose
pseudobulbar affect”
What Causes Pseudobulbar Affect?
In general, “brain damage” is the cause of Pseudobulbar affect
(PBA)”, it could be from:
• “Stroke” when a blood vessel in the brain is blocked or bursts.
Without blood and the oxygen, it carries, part of the brain
starts to die. Then the part of the body controlled by that area
of the brain cannot work properly.
• “Brain tumor” is a collection, or mass, of abnormal cells in your
brain. The skull, which encloses your brain, is very rigid. Any
growth inside such a restricted space can cause problems.
Brain tumors can be cancerous (malignant) or noncancerous
(benign).
• “Neurological disorders” related to neurological disorders”
mainly: “Amyotrophic Lateral Sclerosis”, “Alzheimer dementia”,
“Traumatic Brain Injury (TBI)”, “Cerebrovascular disease”,
“Multiple Sclerosis”, “Parkinsonism”, “Parkinson’s Disease
(PD)”, and others. As explained at “section 3 Pseudobulbar
affect must be evaluated by neurological disorders specialists.
Pathophysiology on Pseudobulbar Affect
The “Pathophysiology” referrers to the study of abnormal
changes in the human body functions that are the causes,
consequences, or concomitants of a disease process. The
“Pathophysiology on Pseudobulbar affect (PBA)” identify a lack of
voluntary control in the “neurons” as specialized cell known as the
basic unit of the “human nervous system”, these “neurons” cells as
shown in figure 1 a make a up a massive network of “specialized
nerve cells” connected with the purpose of transmit messages
very rapidly, from one part of the body to another, creating
complex interconnected circuits known as: “neural pathways”.
They are “clusters of neurons” connections from one part of the
“nervous system” to another using union between them identified
as “synapses” as shown in figure 1 b. The brain under the right
conditions can change hundreds of millions and possibly billions of
the connections between the nerve cells [35] in “neural pathways”
as shown in fig 1 c, every time we learn, react, process and store
new information in the brain or send/receive orders to the nervous
system.
All the neurons transmit signals of mainly two kinds “electrical”
and “chemical”. Where:
“Electrical signals are inside the neurons” and “chemical signals
are between neurons through the synapse space” indicate by blue
circles at figure 1 b and c. The “synapse chemical activity” trigger the
release of “neurotransmitters” which carry the impulse across the
“synapse” to the next “neuron”. Once a nerve impulse has triggered
the release of “neurotransmitter”, these chemical messengers also
known as “hormones” cross the tiny “synaptic space” and taken
up by specialized receptors on the surface of the next cell. “This
process converts the chemical signal back into electrical signal”, if
the signal is strong enough, it will be propagated down to the next
neuron until once again reaches another “synapse” and the process
is repeated once more, and so on until reach the destination as
shown in (Figure 1) c.
The main point to explain the “PBA” disorder is that different
“neurotransmitters” fulfill different functions in the brain as:
“excitatory” and “inhibitory”. Where:
• “Excitatory neurotransmitters” acts stimulating the firing in
the “synapse”, and
• “Inhibitory neurotransmitters” tend to block it in the
responding cell.
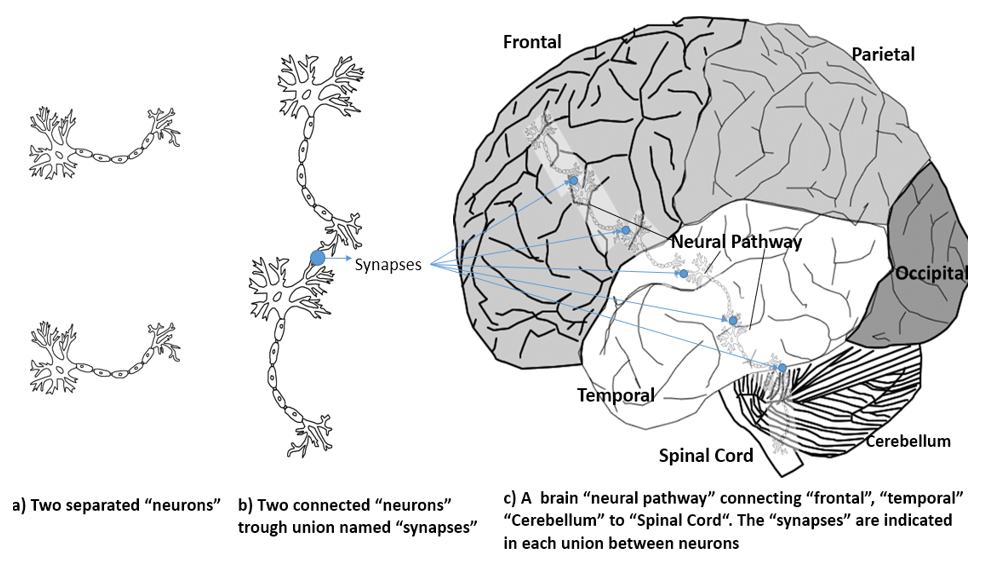
Figure 1: a) Two separated “Neurons”, b) Two Connected “Neurons” Trough “Synapse”, and c) A brain “Pathway””
When the signal reaches its destination is the results of the
combination between “Excitatory and Inhibitory neurotransmitters”
in each “synapse” in the complete “pathway”. There are different
types of small molecules manufactured in different kind of
axons that are in the tail of each neuron, known generally as
“neurotransmitters” [1], some of them are: “acetylcholine”,
“dopamine”, “GABA”, “glutamate”, “glycine”, “norepinephrine”,
“epinephrine or adrenaline”, “serotonin”, and many more. Where:
• “Acetylcholine” has an “excitatory neurotransmitter function”
is used by the “spinal cord” to cause “muscle contraction”, and
many neurons in the brain to regulate memory.
• “Dopamine” has “both inhibitory and excitatory
neurotransmitter functions” depending upon where in the
“brain and which receptor site it binds to”. “Dopamine” plays
a mayor role in regulate movement, attention, learning, and
emotional responses.
• “GABA” has an “inhibitory neurotransmitter function”. It is
important to produce sleep, reducing anxiety, and forming
memory.
• “Glutamate” has an a powerful “excitatory neurotransmitter
function”. It is important in learning and memory.
• “Glycine” has a “inhibitory neurotransmitter function”. It is
used mainly by the neurons in the “spinal cord”.
• “Norepinephrine” has “inhibitory and excitatory neurotransmitter
functions”. It is used to regulate blood pressure and
calmness.
• “Epinephrine or adrenaline” has “excitatory neurotransmitter
function” in the “peripheral nervous system” and “inhibitory
neurotransmitter function” in a few brain areas. The Key
actions of “adrenaline” include increasing the heart rate,
increasing blood pressure, expanding the air passages of the
lungs, enlarging the pupil in the eye, redistributing blood to the
muscles, and altering the body’s metabolism, with the purpose
of maximize blood glucose levels primarily for the brain.
• “Serotonin” has “inhibitory neurotransmitter function”. It is
a complex and multifaceted, modulating mood, cognition,
reward, learning, memory, and numerous physiological
processes. Low levels of “serotonin” in the brain may cause
depression, anxiety, and sleep trouble.
And many other neurotransmitters types are used in the
synapses in the neural pathways.
There are an estimated of 100 billon “neurons” making an
approximation of 100 trillion “neural connections”. These process
information in the brain, and they can send orders to “body
movements” known as “motor pathways” and receive information
from “humans’ senses” known as “sensory pathways”, “the pathways
are so complex and are not completely understood”. Besides
store memories, update them, new ones from new ideas based
on creativity or reconnection of old information stored. Detailed
reviews of the widespread anatomical and neurophysiological
abnormalities found by Neuroimaging and neurophysiological
studies in patients with “Pseudobulbar affect (PBA) disorder seemsto indicate that the neuronal paths shown unbalanced between
the inhibitory and excitatory neurotransmitter functions in the
synapses involved in the pathways” [46].
The “primary neurotransmitters” believed to be involved
in “PBA” are “serotonin” and “glutamate”. Based on the role of
“serotonin as inhibitory neurotransmitter function in corticolimbic
or cerebellar pathways” may account for its impact on this disorder.
“Glutamate” as an “excitatory neurotransmitter function” that is
present in over 90% of all “brain synapses”, whose receptors are
widely distributed within the brain. Thus, bases on clinical research:
• The areas of the brain that control the expression of emotion,
such as the “prefrontal cortex” are frequently affected on
patients with “PBA” [36].
• The alterations in chemicals in the brain that contribute to
the development of the condition. Disrupting brain signaling,
triggering episodes the person affected cannot control,
the most common are “In the synapses the modulation
of glutamatergic and serotonin transmission” [37]. These
unbalance on different “synapses on brain pathways” can have
widespread effects, and that are affected by “brain damage” as
explained in this paper “section 5 What causes PBA? “ [47 ]
• Other researches had concluded: “In the brain pathways the
cerebellum appears to play a far larger role in PBA”. There are
pathways from the “cortex to pons to cerebellum that appear
to control not only motor, but also cognitive and affective
function” [29]
• It likely results from the compromise of a network of
descending pathways, specifically the “cortico-pontinecerebellar
circuit” as one of the largest pathways associated
with the “cerebellum”. Arising in the cerebral cortex these
fibers first terminate ipsilaterally in the pontine nuclei. Then
the fibers decussate and form the middle cerebellar peduncle,
terminating in the cerebellar cortex as mossy fibers, and/
or dysfunction in certain neurotransmitters, particularly
“serotonin and glutamate” [16].
Pseudobulbar Affect Strategies and Treatments
There is not known cure for “Pseudobulbar affect (PBA)”,
but it has been proving the severe complications related as
embarrassment, social isolation, anxiety, and depression. The
condition might interfere with your ability to work and do daily
tasks, especially when you are already coping with a neurological
condition. Besides, medications can reduce the number of “PBA”
episodes or make them less intensive.
“Lifestyle strategies may help manage PBA” as:
• Keeping a diary to track what triggers the episodes and sharing
it with a doctor.
• Also, when a person feels an episode approaching, he or his/
her caregiver may try to focus on something unrelated and
adjust his posture.
• Taking slow, deep breaths during an episode until they are
in control also may help, and so can relaxing the forehead,
shoulders, and body.
• Build a healthy environment free of worries to the affected
people like avoiding everyday impact news, staying away from
pessimistic people that usually speak about bad news, stop
given to much importance to “PBA episodes”, etc.
“The goal of treatment of PBA is no to cure but focus into
diminish the severity and frequency of the episodes”. This is achieved
targeting the primary “neurotransmitters” that affect cognition and
emotions as “norepinephrine”, “serotonin”, or “glutamate” allows
under specialized medical recommendation and supervision
as “antidepressants”, “Selective serotonin reductase inhibitors
(SSRIs)”, “Cough suppressant dextromethorphan”, “Dopaminergic
medications” and others. Where:
• “Antidepressants” as “Tricyclic antidepressants (TCAs)” [37]
for the treatment of “PBA” are typically prescribed at doses
lower than are those used to treat depression [38].
• “Selective serotonin reductase inhibitors (SSRIs)” [39] these
are a class of drugs that are typically used as antidepressants in
the treatment of major depressive disorder, anxiety disorders,
and other psychological conditions.
• “Cough suppressant dextromethorphan” [38]. This time,
the only treatment currently approved by the U.S. Food
and Drug Administration (FDA) for the treatment of “PBA”
is an oral medicine that contains “dextromethorphan
hydrobromide and quinidine sulfate”. The active ingredients
are dextromethorphan hydrobromide monohydrate USP and
quinidine sulfate dihydrate USP [39][40][48]
• “Dopaminergic medications” such as “levodopa and
amantadine” have been used as well, but with lower response
rates [41]
Testimony to Diagnose Pseudobulbar Affect
I am a caregiver of a family member with “Parkinsonism:
Atypical Parkinson” neurological disease as a both a chronic
and progressive movement. After 5 years her Parkinsonism:
Atypical Parkinson” was identified as: “Progressive Supranuclear
Palsy (PSP)” is the most common degenerative type of atypical
parkinsonism. Symptoms tend to progress more rapidly than “PD”.
People with “PSP” may fall frequently early in the course of disease.Later symptoms include limitations in eye movements, particularly
looking up and down, which also contributes to falls. Those with
“PSP” also often have problems with swallowing (dysphagia),
difficulty in producing speech (dysarthria), sleep problems,
memory and thinking problems (dementia). Its average age of
onset is in the mid-60’s.
Where was notorious the frequently crying since the
beginning of her Parkinson’s, usually without any apparent
reason, unfortunately the specialized doctors took 10 years from
the beginning of her disease to correctly identified the additional
disorder as “pseudobulbar affect (PBA)”, probing that is extremely
hard to detect correctly besides her neurological progressive disease
even for specialized doctors. Consulting different specialized
doctors that were following the way of diagnoses her suddenly
crying as different conclusions: “Stress-Anxiety”, “Neuropathic
Pain”, “sleep disorders”, and “Depression”. Where the treatments
and results were:
“Stress” as a response to a threat in a situation and “anxiety” is
a physical reaction to the “stress” [1].
• They recommended treatment based on: A comfortable family
environment was built, free of worries and problems of any
kind to reduce her “anxiety” and by consequence her “stress”,
with a lot of personal care, love, and comprehension.
• Result: It helped to reduce it, but the “crying” episodes
continued.
“Neuropathic Pain” is often described as a burning or shooting
pulses, she suffered of numbness and tingling, and frequently
feel pain from a touch that would not normally be painful. In her
specific case was diagnosed to mainly “stiff muscles” complaint.
• Recommended treatment: “Frequently rest” was implemented
because the persons with neurologic disease uses more energy
to do anything that a normal people, and they frequently feel
very tired. Periodic “muscles massage” to increase relaxation,
reduce pain improve blood circulation and alertness, and
“applications of heat or cold” base in the fact that “heat work”
is better for muscle tightness and “cold” may work better for
swelling and inflammation. The options were to apply hot and
cold packs, heating pads, heat therapy patches and diclofenac
sodium topic gel.
• Result: It helped to reduce it a little more, but the “crying”
episodes continued.
“Sleep disorders” in neurological disorders is frequently suspect
the accumulated actions from years to of “stress” and “anxiety”
plus others factors as: aging, hormonal levels changes, mood,
sleep apnea, snoring poor lifestyle environment changes, etc.
• Recommended treatment: In her case the sleep cycles in quality
and duration presented a “Rapid Eye Movement behavior
disorder” characterized by “dream enactment (acting while
dreaming)” where the muscle paralysis that normally occurs
during “REM Sleep stages” was incomplete or absent [40]. She
also presented “Rest less syndrome” as a condition that causes
an uncontrollable urge to move your legs during resting [43].
• Recommended treatment: “Ramelteon as hypnotics -
melatonin M1/M2 Receptor agonists”, but it did not work, then
a prescription of an antidepressant that belongs to a group
of drugs called “serotonin receptor antagonists and reuptake
inhibitors (SARIs)”. She only achieved to sleep 2 o 4 hours
every night, the final prescription was a “Sedative-Hypnotic –
Benzodiazepines”, and finally it works achieving 7-8 hours of
sleep.
• Result was that the suddenly crying diminish about 33% in
total.
“Depression” as a continuous symptom as: feelings of sadness,
feelings of hopelessness, loss of interest/lack of pleasure, short
temper, irritation, tiredness, memory loss, sleep disorders,
crying uncontrollably, reduced appetite and weight Loss, etc.
• Recommended treatment: Antidepressants to relax the mind
and Psychotherapy ·.
• Result: was that the suddenly crying diminish a little more
about 40% in total.
After 10 years of visiting different specialized neurologists,
one detected her disproportionate Patient’s emotional response
in an episode as “Pseudobulbar affect (PSA)” as described in this
research under a normal evaluation appointment.
• Recommended treatment contains “dextromethorphan
hydrobromide and quinidine sulfate”.
• Result: was that the suddenly crying diminish a little
more about 70%-80% in total.
Pseudobulbar Affect Conclusions
“Pseudobulbar affect (PBA)” is a nervous system disorder
that is reflect with suddenly emotions of crying/laughing without
control and it is related with: brain injuries including stroke, and
neurological disorders based in the following conclusions:
• “Pseudobulbar affect (PBA)” affects the areas of the brain
that control the expression of emotion, such as “prefrontal
cortex”, there also maybe alterations in the “chemical
neurotransmitters” that contribute the development of this
condition. These alterations may disrupt brain signaling,
triggering episodes that the person affected cannot control.
• “Pseudobulbar affect (PBA)” is often unrecognized and
misdiagnosed. Patients with “PBA” experience episodes of
spontaneous or exaggerated laughter and/or crying that are
disproportionate to or inappropriate for the current situation.
It is often mistaken for mental health conditions such as
depression and hidden by the symptoms of the commonly
associated neurologic diseases mainly: “Amyotrophic Lateral
Sclerosis”, “Alzheimer dementia (AD)”, “Traumatic Brain
Injury (TBI)”, “Cerebrovascular disease”, “Multiple Sclerosis”,
“Parkinsonism”, “Parkinson’s Disease (PD)”, and others
• “Caregivers has a substantial burden when caring for patients
with PBA” compared with caregivers of patients with the same
underlying neurological condition but without “PBA” that
affects patients [44].
• “PBA can be managed with pharmacologic intervention”
including Antidepressant medicine, usually in a lower dose
than for depression or Dextromethorphan and quinidine as
the first line drug of choice for PBA [45, 31].
• “PBA” in nursing home residents was associated with chart
documentation of uncontrollable crying, presence of a
neurologic disorder, or by the documented presence of at least
2 of the following: stroke, severe cognitive impairment, and
schizophrenia [11]
• “At this time has been find that several brain pathways
contribute to laughter and crying in PBA”, each with different
brain areas and component to achieve the emotion that
control our behavior to be “inhibited or excited” to facilitate
the correct balance by “neurotransmitter” on the connection
between neurons identified as “synapses.”
This research paper main objective is to diminish the time to
obtain the correct diagnose of “Pseudobulbar affect (PBA)” making
a general observations to document the typical symptoms from
the patients by caregiver, their loved one, healthcare provider at
palliative or hospice health care providers to facilitate different
specialized doctors as neuropsychologist, neurologist, and
psychiatrist to obtain a valid diagnostic beside the complexity of
symptoms combined neurological condition or brain injuries in the
less possible time to improve the quality of life of “PBA” patients.
“You bring me smiles at the moments of tears, you demonstrate strength in moments”
References
- Jorge Garza Ulloa (2019) Theory of Stress-Anxiety-Sleep Disorders-Neural Damage Cyclic Chain and the Progression of Parkinson’s Disease. Am J Biomed Sci & Res 6(3).
- Cordelia Gray, Alex Calderbank , Joy Adewusi , Rhiannon Hughes, Markus Reuber (2020) Symptoms of posttraumatic stress disorder in patients with functional neurological symptom disorder. J Psychosomatic Res 129: 109907.
- Victor C Wang, William J Mullally (2020) Pain Neurology. Am J Med 133(3): 273-280.
- Malcolm Lader, Issac Marks (1971) Chapter Three - CLINICAL ANXIETY, Editor(s): MALCOLM LADER, ISSAC MARKS, Clinical Anxiety, Butterworth-Heinemann 22-49.
- Jesse L Parker, Sarah L Appleton, Yohannes A Melaku, David Stevens, Gary A Wittert, et al. “Sleep macroarchitecture but not obstructive sleep apnea is independently associated with cognitive function in only older men of a population-based cohort”. J Sleep Res 13370.
- Jennaya Christensen, Glenn R Yamakawa, Sandy R Shultz, Richelle Mychasiuk (2021) Is the glymphatic system the missing link between sleep impairments and neurological disorders? Examining the implications and uncertainties. Prog Neurobio 198: 10191.
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/depression], 05/04/2021.
- Alex Presciutti, Mary M Newman, Ana Maria Vranceanu, Jonathan A Shaffer, Sarah M Perman (2020) Associations between depression and anxiety symptoms with quality of life in cardiac arrest survivors with good neurologic recovery and informal caregivers of cardiac arrest survivors,Journal of Affective Disorders Reports, 100046.
- https://www.mayoclinic.org/diseases-conditions/bipolar-disorder/symptoms-causes/syc-20355955 , 05/06/2021
- Lars Vedel Kessing, Simon Christoffer Ziersen, Per Kragh Andersen, Maj Vinberg (2021) A nation-wide population-based longitudinal study mapping physical diseases in patients with bipolar disorder and their siblings. J Affect Disord 282: 18-25.
- Carrie Allen, Barbara Zarowitz, Terrence O Shea, Edward Peterson, Charles Yonan, et al. (2018) Identification of pseudobulbar affect symptoms in the nursing home setting: Development and assessment of a screening tool. Geriatr Nurs 39(1): 54-59.
- Hess U, Thibault P (2009) Darwin and emotion expression. Am Psychol 64(2): 120-128.
- Parvizi J (2009) Pathological laughter and crying. In: Savitz SI, Ronthal M, eds. Neurology review for psychiatrists. Philadelphia: Lippincott Williams and Wilkins, 68-72.
- Wilson SAK (1924) Some problems in neurology. II: pathological laughing and crying. J Neurol Psychopathol 4: 299-333.
- Parvizi J, Coburn KL, Shillcutt SD (2009) Neuroanatomy of pathological laughing and crying: a report of the American Neuropsychiatric Association Committee on Research. J Neuropsychiatry Clin Neurosci 21(1):75-87.
- Reus and D. Lindqvist (2019) Handbook of Clinical Neurology,Vol. 165 (3rd series)Psychopharmacology of Neurologic Disease V.I. Editorshttps://doi.org/10.1016/B978-0-444-64012-3.00014-9Copyright © 2019 Elsevier B.V
- https://www.mayoclinic.org/diseases-conditions/amyotrophic-lateral-sclerosis/symptoms-causes/syc-20354022
- https://www.alz.org/alzheimers-dementia/what-is-alzheimers, 05/04/2021
- https://www.alz.org/alzheimers-dementia/what-is-dementia/types-of-dementia, 05/06/2021
- https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557, 05/04/2021
- A Obenaus, Loma Linda (2016) Encyclopedia of Mental Health (Second Edition), Traumatic Brain Injury Elsevier Inc.
- https://www.medicalnewstoday.com/articles/184601
- https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269, 05/042021.
- Maria K. Houtchens, Samia J. Khoury (2013) in Women and Health (Second Edition).
- Jorge Garza-Ulloa (2019) A Parkinson’s Disease Journey from Patient side view. Am J Biomed Sci & Res 5(1).
- Alice Hosking, Adrianus A L J Hommel, Stefan Lorenzl, Miguel Coelho, Joaquim J Ferreira, et al. (2021) Characteristics of Patients with Late-Stage Parkinsonism Who are Nursing Home Residents Compared with those Living at Home. Journal of the American Medical Directors Association 22(2): 440-445.
- Jorge Garza-Ulloa (2019) Update on Parkinson's Disease. Am J Biomed Sci & Res 2(6): AJBSR.MS.ID.000614
- Nutan Sharma (2008) in Essentials of Physical Medicine and Rehabilitation (Second Edition), 2008
- Poeck K (1969) Pathophysiology of emotional disorders associated with brain damage. In: Vinken P, Bruyn G, eds. Handbook of clinical neurology 3: 343-367.
- Jeffrey L Cummings, David B Arciniegas, Benjamin R Brooks, Robert M Herndon, Edward C Lauterbach, rt al. (2006) Defining and diagnosing involuntary emotional expression disorder. CNS Spectr 11(6):1-7.
- Young D Chang, Mellar P Davis, Joshua Smith, Terrence Gutgsell (2016) Pseudobulbar Affect or Depression in Dementia?. J Pain Symptom Manage 51(5): 954-958.
- https://www.psychcongress.com/saundras-corner/scales-screeners/pseudobulbar-affect-pba/center-neurologic-study-liability-scale-cns, 05/05/2021
- https://mstrust.org.uk/a-z/pseudobulbar-affect-pathological-laughing-and-crying
- Roy E Strowd, Michael S Cartwright, Michael S Okun, Ihtsham Haq, Mustafa S Siddiqui (2010) Pseudobulbar affect: prevalence and quality of life impact in movement disorders. J Neurol, 257(8): 1382-1387.
- Suzuki K, Miyamoto M, Miyamoto T, Hirata K (2015) Parkinson's disease and sleep/wake disturbances, Curr Neurol Neurosci Rep15(3): 8.
- https://www.mayoclinic.org/diseases-conditions/pseudobulbar-affect/symptoms-causes/syc-20353737,05/08/2021
- https://www.ajmc.com/view/pharmacotherapeutic-management-of-pseudobulbar-affect, 05/08/2021
- https://www.mayoclinic.org/diseases-conditions/pseudobulbar-affect/diagnosis-treatment/drc-20353741#:~:text=Antidepressants%20for%20the%20treatment%20of,designed%20to%20specifically%20treat%20PBA., 05/05/2021
- Ahmed A, Simmons Z (2013) Pseudobulbar affect: prevalence and management. Ther Clin Risk Manag 9:483-489.
- Miller A, Pratt H, Schiffer R. Pseudobulbar (2011) affect: the spectrum of clinical presentations, etiologies, and treatments Expert Rev Neurother 11:1077-1088.
- Villeneuve Y, Cruz Santiago D, Masson H, Clerc D (2020) Treatment of pseudobulbar affect in a mixed neurodegenerative disorder with compounded quinidine capsules and dextromethorphan cough syrup. SAGE Open Med Case Rep 8:2050313X20921076.
- https://www.mayoclinic.org/diseases-conditions/rem-sleep-behavior-disorder/symptoms-causes/syc-20352920, 05/14/2021.
- https://www.mayoclinic.org/diseases-conditions/restless-legs-syndrome/symptoms-causes/syc-20377168, 05/14/2021
- Tammie Lee Demler (2017) Introduction to Pseudobulbar Affect: Setting the Stage for Recognition and Familiarity with This Challenging Disorder. Am J Manag Care (18): 339-344.
- Healthwise Staff Medical Review:E. Gregory Thompson MD - Internal Medicine & Colin Chalk MD, CM, FRCPC – Neurology August 4, 2020.
- Jorge Garza-Ulloa (2018) Chapter 7 - Case studies of applied Biomechatronics solutions based on mathematical models,Applied Biomechatronics using Mathematical Models, Academic Press 525-626.
- Jorge Garza Ulloa (2018) Chapter 2 - Introduction to human neuromusculoskeletal systems, Editor(s): Jorge Garza-Ulloa, Applied Biomechatronics using Mathematical Models, Academic Press 53-118.
- Pioro EP (2011) Current concepts in the pharmacotherapy of pseudobulbar affect. Drugs 71(9):1193-1207.





 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.