Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
9-Month-Old Girl with Thoracic Neuroblastoma Encasing the Subclavian Artery, a Case Report
*Corresponding author: Vlahova A, Department of pediatric surgery, UMHATEM “N. I. Pirogov” - Sofia, Bulgaria
Received: October 14, 2021; Published: October 26, 2021
DOI: 10.34297/AJBSR.2021.14.002017
Abstract
Neuroblastoma is the most frequent extracranial tumor in children having 15% of the cases with thoracic location. The manifestation of such a tumor encasing the subclavian vessels is extremely rare. We present in this paper a 9-month-old girl born by Cesarean delivery from a first nonpathological pregnancy, weighing 3500g. At the age of 8 months parents noticed facial asymmetry and decreased temperature of the left upper extremity. After a pediatric neurologist exam, a head, neck, and thorax magnetic resonance imaging (MRI) was made upon which a tumor located in the front and middle mediastinum encasing the left carotid artery and left subclavian artery was found. The tumor was entirely removed but in the course of operation the left subclavian artery was ligated. Histopathology revealed differentiating neuroblastoma.
We present this case due to the uncommon clinical manifestation of apical neuroblastoma in early childhood age encasing the magistral vessels and the necessity of ligating the left subclavian artery while removing the tumor. The patient follow-up showed good collateral circulation response of the left upper extremity, reduction of the symptoms, and preserved function of the arm.
Keywords: Subclavian artery, Neuroblastoma, Ligation, Children
Abbreviations: NSE: Neuron-Specific Enolase; MRI: Magnetic Resonance Imaging; PET-CT: Positron Emission Tomography - Computed Tomography
Introduction
Neuroblastoma is an embryonic tumor of the sympathetic nervous system in infancy and childhood. The origin of this tumor is the primordial neural crest, which develops into sympathetic ganglia and the adrenal medulla. The migration of the neuroblasts defines the diverse localization of this kind of tumor. The most frequent localization is with abdominal disposition (adrenal gland - 40%, sympathetic ganglia - 25%), followed by thoracic - 15%, pelvic - 5%, cervical - 3% and miscellaneous - 12% [1]. The manifestation of such a tumor encasing the subclavian vessels is extremely rare [2]. Most of the patients have signs and symptoms related to the tumor growth. Diagnosis can be determined by ultrasound imaging (prenatal and after the manifestation of the symptoms), computed tomography scan, or magnetic resonance imaging (MRI). Serum neuron-specific enolase (NSE) level is a marker with diagnostic and prognostic significance. Treatment includes surgery and/or chemotherapy. Surgery could be performed with intent of diagnosis (biopsy) or cure (radical removal of the tumor).
In this paper we present the case of a 9-month-old girl with apical neuroblastoma encasing the left subclavian artery while during the surgical procedure the artery was ligated. The aim of this study is the surveillance of the long-term effects associated with such kind of surgical procedure in early childhood.
Materials and Methods
We present a 9-month-old girl born by Cesarean delivery from a first, non - pathologic pregnancy, weighing 3500g. Neonatal period was uncomplicated, without pathologic conditions. No family health history to be considered. When the child was 8-month-old parents noticed facial asymmetry and decreased temperature of the left upper limb. The patient was admitted to a pediatric neurologic ward for diagnostic work-up. During the clinical examination Horner syndrome [3] was established with miosis and ptosis of the left eyelid, as well as weaker peripheral left arm pulses. A head, neck and thorax MRI was performed which revealed a tumor located in the anterior and middle mediastinum, encasing the left common carotid artery and left subclavian artery (Figure 1). A pediatric cardiologic consult determined reduced Doppler signals of the left upper limb arteries. Echocardiography showed a tumor mass encasing the left brachiocephalic vessels and the aortic arch (without infiltration) and presence of a small pericardial effusion behind the left ventricle. The patient was discussed with a pediatric surgeon to be submitted for surgery.
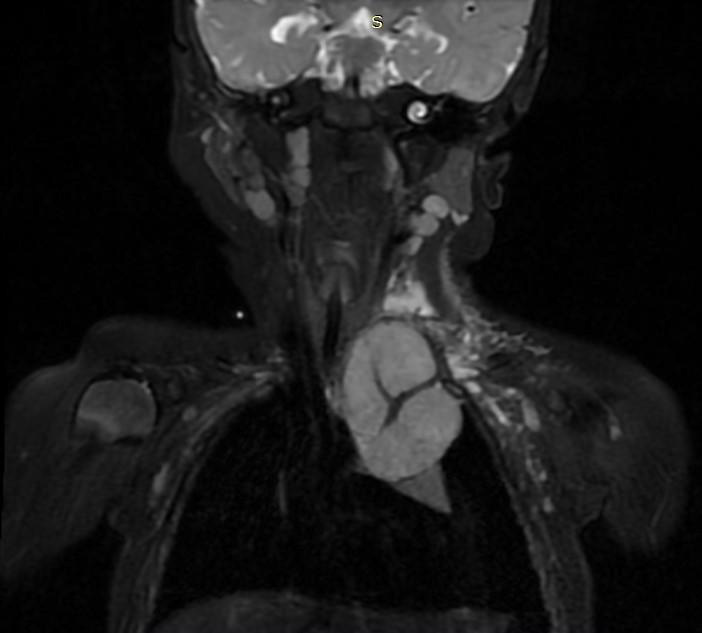
Figure 1. Magnetic resonance imaging (MRI) before the surgery. The tumor formation encasing the subclavian artery is presented.
At admission to the Pediatric thoracic surgery department, the child was in a slightly poor general condition with swollen venous network of upper third of the left thoracic half, miosis of left pupil, and ptosis of left eyelid non-covering the pupil. Low grade decreased temperature of the left upper extremity with preserved peripheral pulses during the exam. Breathing was bilateral vesicular without wheeze. Laboratory tests before the surgical intervention establish leukocytosis, anemia, thrombocytosis and NSE - 163 ng/ml (reference level <17 ng/ml). Chest X-ray showed a tumor in the upper mediastinum on the left side, 4,7cm/3,2cm in size, dislocating the trachea to the right and the left main bronchus to caudal direction (Figure 2).
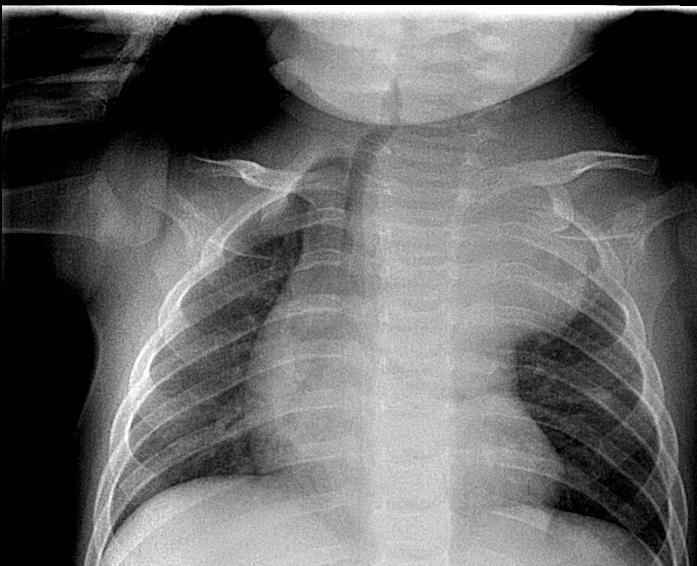
Figure 2. Chest X-ray showing a tumor in upper mediastinum, dislocating the trachea to the right and left main bronchus in caudal direction.
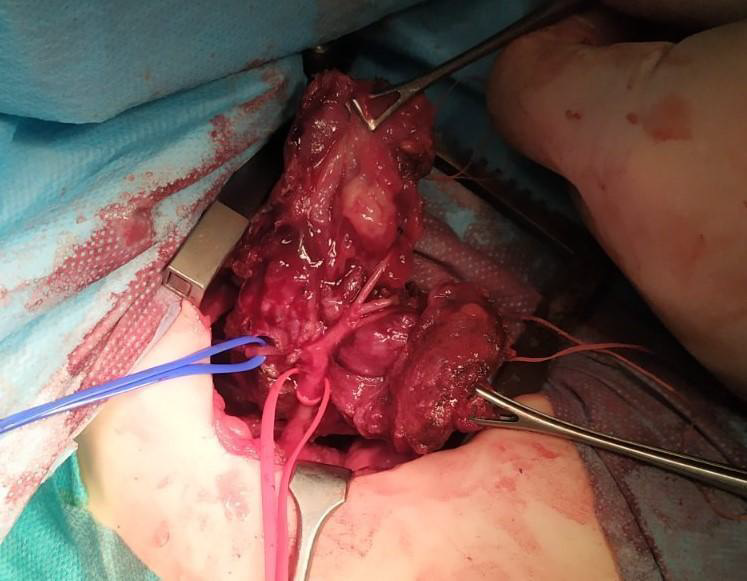
The operation was performed by a team of pediatric surgeon and pediatric cardiothoracic surgeon. Thoracoscopically a capsulated, highly vascularized, ovaly shaped tumor with diameter 4cm/5cm in size was found. The lesion had necrosis zones, easily raw in contact, originating from posterior mediastinum, expanding in anterior superior and middle mediastinum, and located in front of the aortic arch encasing the magistral vessels - left common carotid artery and left subclavian artery. Infiltration in the adjacent organs of the mediastinum and pleural cavity was not determined. The team made the decision that the tumor is curable and left lateral thoracotomy in 3th intercostal space was performed (Figure 3). During the operation, the left common carotid artery and recurrent laryngeal nerve were identified. Pericardiacophrenic vessels and nerve, left vagus nerve, left mammary artery, and intercostal vessels and nerves were ligated. Left subclavian artery was entering into the center of the lesion which led to ligation. The ligature was made after the separation of the left vertebral artery. It was estimated that it is not possible to perform End-to-End anastomosis between the proximal and distal end of the artery due to greater space between the segments. Left subclavian vein was dissected proximally. The tumor formation was removed radically (Figure 4). A 14Ch drain tube was inserted into the pleural cavity.
Immediately following the procedure the left upper extremity was with decreased temperature, with marmorated skin and barely perceptible peripheral pulses. During the first postoperative day the left hand was of pink color and with palpable pulses. The drain tube was removed on the fourth postoperative day. The surgical wound healed primarily. The postoperative period was uneventfully without complications. Histopathology revealed differentiating neuroblastoma. The child was discharged from the hospital in good condition - permanently afebrile, without manifestation of pulmonary insufficiency, persisting miosis and ptosis of left eyelid, with hoarse voice. She mildly spared her left upper extremity, had good active and passive movements, and palpable peripheral pulses.
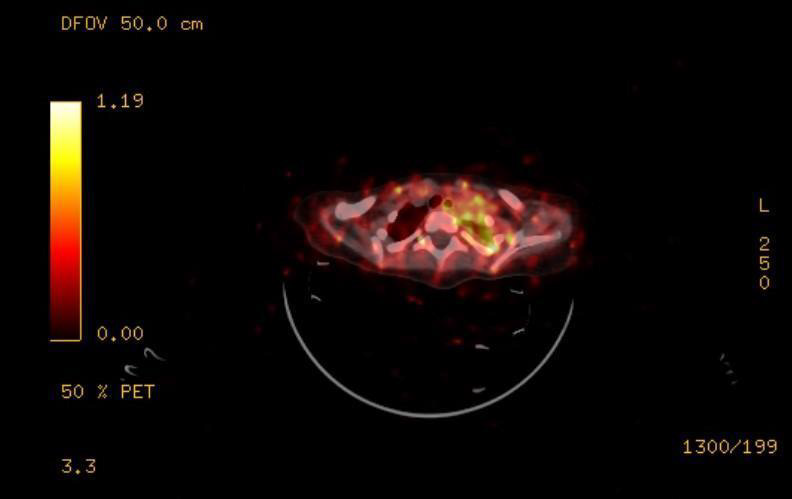
Figure 5: PET-CT showing residual soft tissue in the left superior thoracic aperture above the first rib.
The 20 days after the intervention follow-up of the patient examined levels of Neuron-specific enolase 55,27μg/L (reference level 16,3μg/L) and revealed normal hematology results. The DNA analysis of the tumor material does not show any amplification of MYCN gene. PET-CT conducted one month after the surgery revealed evidence of residual soft tissue in the left superior thoracic aperture above the first rib, probably encasing the sympathetic nerves (Figure 5). This imposed the implementation of chemotherapy courses.
During the clinical examination the child was in good condition, with persisting ptosis and miosis but mild improvement, without hoarse voice, the thorax was symmetrical, the operative wound healed primarily, auscultation showed bilateral vesicular breathing without crepitation. The left upper extremity was of pink color with palpable peripheral pulses, without any difference in the temperature of the two arms and preserved active and passive movements with mild sparing of the left hand and third, fourth, and fifth fingers. The control chest X-ray does not show any tumor. The ultrasound scan 45 days after the surgery revealed normal size of the left brachial artery with reduction of the blood flow. Direct Doppler sounds of the brachial artery and radial artery were detected.
Discussion
In literature, most cases with ligation of the left subclavian artery in children under one year are described in cardiothoracic patients with repair of coarctation of the aorta. Subclavian flap angioplasty (SFA) is an operative technique in which the left subclavian artery is ligated and transected distally at its thoracic outlet and subsequently is used to reconstruct the aorta. This procedure results in reduction of blood supply to the left arm. In these cases, the upper extremity is supplied by blood from the formed collateral arterial branches [4].
The late results of ligating the subclavian artery present in decrease in length of the upper extremity thoroughly for the account of the long bones and muscle thickness. Bone age and the circumferential bone growth are not affected. The affected extremity compensates by subcutaneous fat increase in part for the loss of muscle mass. In some patients a difference in the temperature of the two arms is found. The occurrence, type, and severity of the changes cannot be predicted in an individual due to the different responses of the collateral circulation and other various limb components to the decreased blood supply. Despite the shortening of the affected arm, these changes seem to have little clinical significance in the long-term concern. Patients inform of having mild weakness of the affected limb, however, easily using both arms [5].
The possible types of reconstruction of the ligated subclavian artery are to construct an End-to-End anastomosis or to implant a synthetic graft in case of greater space between the segments. These methods are used in adult patients in which the subclavian artery was ligated while removing an apical tumor. Ligation of the subclavian artery without revascularization in these cases would result in upper limb ischemia [6]. In contrast to adults, children have much higher potential for developing collateral arterial circulation. In children the decreased extremity blood flow can be compensated by a decrease in the peripheral vascular resistance.
Conclusion
Our study shows that the ligation of the subclavian artery encased by a tumor in children under one year is possible and not related with severe long-term results. In children the formation of arterial collaterals can almost completely compensate the limb blood flow and the function of the affected arm is preserved.
References
- Lacayo NJ, Davis KL (2021) Pediatric Neuroblastoma, Medscape.
- Pelton JJ, Ratner IA (1990) Neuroblastoma of the thoracic inlet. Journal of Pediatric Surgery 25(5): 547-549.
- Barrea C, Vigouroux T, Karam J, Milet A, Vaessen S, (2016) Horner Syndrome in Children: A Clinical Condition with Serious Underlying Disease. Neuropediatrics 47(4): 268-272.
- Van Son JA, Van Asten WN, Van Lier H, Daniëls O, Vincent JG et al. (1990) Detrimental Sequelae on the Hemodynamics of the Upper Left Limb After Subclavian Flap Angioplasty in Infancy. Circulation 81(3): 996-1004.
- Currarino G, Engle MA (1965) The effects of ligation of the subclavian artery on the bones and soft tissues of the arms. J Pediatr 67(5): 808-811.
- Lahon B, Mercier O, Fadel E, Mussot S, Fabre D, et al. (2013) Subclavian Artery Resection and Reconstruction for Thoracic Inlet Cancer: 25 Years of Experience, Presented at the Forty-ninth Annual Meeting of The Society of Thoracic Surgeons. Los Angeles CA 96(3): 988-989.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.