Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Analysis of the Variation in Corneal Parameters with regard to Refractive Error in Saudi Arabian Adults
*Corresponding author: Saleh A Alkhaldi, Ophthalmology department, King Saud Medical City, Riyadh, Saudi Arabia.
Received: October 05, 2021; Published: November 02, 2021
DOI: 10.34297/AJBSR.2021.14.002025
Abstract
Aim: This study focused on exploring the effects of refractive error and its association with various corneal parameters such as corneal curvature (CC), corneal thickness (CT), endothelial cell density (ECD), and cell volume (CV) among young adults in Saudi Arabia.
Methodology: A total of 70 Saudi Arabian participants were divided into the following three groups: myopia, ametropia, and hyperopia. The corneal parameters and refractive error were investigated through examination with an auto refractometer (KR-8100 A) and specular microscope (SP-2000 P). Corneal parameters including CC, CT, ECD, and CV were comprehensively analyzed for these groups.
Results: The mean age of the participants was 23.2 ± 2.42 years. A statistically significant correlation of mean spherical equivalent (MSE) with CC (r = 0.77, p < 0.05) and ECD (r = 0.34, p < 0.05) was determined, with steep (43.43 ± 1.04) and flat (41.4 ± 0.77) CC among individuals with myopia and hyperopia, respectively. ECD was the highest (3250.1 ± 242.75) in the hyperopic group, including participants with myopia with least but statistically significant correlation (2964.9 ± 307.68). However, CT (r = 0.05, p = 0.66) and CV (r = 0.05, p = 0.65) were not significantly associated with MSE across all groups.
Conclusion: MSE is significantly associated with the changes in CC and ECD. However, central CT and coefficient of variation of CV were in the normal range and were poorly correlated with respect to changes in MSE.
Keywords: Refractive error, Corneal curvature, Corneal thickness, Endothelial cell density, Cell volume, Correlation
Abbreviations: CC: Corneal Curvature; CT: Corneal Thickness; ECD: Endothelial Cell Density; CV: Cell Volume; MSE: Mean Spherical Equivalent; CL: Contact Lens
Introduction
The cornea is an integral part of the eye which is involved in the optical system that enables optimum visual acuity [1]. Visual acuity relies not only on the cornea itself but also on other factors such as pathological state of the eye and refractive error [2]. These anomalies can cause substantial visual impairment if not corrected on time, even among patients with emmetropia [3]. Emmetropia is characterized by an ability of the human eye to focus parallel light rays on the retina when accommodation is relaxed; however, if the optical system fails to focus images sharply on the retina, the eye will be ametropic and exhibit myopia, hyperopia, or astigmatism [4].
Among adults, pathological changes, such as short-term ocular infections involving inflammation, that can significantly alter the refractive error are unusual [5]. The progression of refractive error substantially relies on the overall visual stimulation affecting the corneal parameters and even a minor alteration in the development of refractive error such as myopia, can lead to irreversible steeper cornea and axial expansion compared with patients with emmetropia [6]. A reciprocal effect of flat corneal curvature (CC) is observed among patients with hyperopia; moreover, astigmatism is an additional component where CC varies in different meridians [7].
Numerous publications have reported a strong relationship between refractive error and corneal parameters with myopiaoriented subjects, the literature is scarce among the emmetropes as well as hypermetropic Arabian individuals [1]. The general health of the corneal tissue relies on various parameters, such as its CC, corneal thickness (CT), endothelial cell density (ECD), and cell volume (CV) [8]. Normal human eyes have a CT of approximately 0.5 μm and a radius of curvature of approximately 8 mm. In addition, it contributes to approximately 43D of the total ocular power, which varies in case of a refractive error [9]. Refractive errors are highly prevalent among the adult population in Saudi Arabia, and significant number of urban dwellers present with CCinduced astigmatism (66.3%), followed by myopia (48.7%) and hyperopia (25.2%) [10]. Moreover, contemporary literature has shown that the toricity of posterior CC can also affect the refractive error independently, irrespective of the anterior CC [11]. However, regarding gross refractive error correction and progression, most studies have found a strong correlation of equal contribution toward refractive error by both corneal surfaces [12]. Furthermore, recent literature indicates a sharp increase in the prevalence of axial myopia, instead of CC-induced astigmatism or central CT-induced refractive error, among young Arabian individuals [13]. This is well explained in previously published articles by demonstrating that CT as an independent factor is poorly associated with CC and refractive error development [8]. Even in the presence of a high degree of refractive error, multiple studies have shown an insignificant and poor correlation between CT and refractive error [14]. However, one should remember that a healthy CT represents rigidity, acts as a decisive factor for refractive error surgeries, and significantly affects intraocular pressure evaluation [15,16].
Extended use of contact lens (CL) can lead to polymegethism, a condition ideally represented by increased endothelial CV that can cause endothelial degeneration [17]. The association of refractive error with abnormal CV is reportedly stronger in women than in men owing to prolonged CL use among women [18]. Furthermore, refractive error, CL material, gender, and regional status are the major factors influencing the use of CL [7,19]. However, literature exploring the variation among corneal parameters in Saudi Arabian young adults who only used spectacles is limited [1]. Therefore, this study aimed to explore the effects of refractive error and its association with the abovementioned corneal parameters among Saudi Arabian adults who used spectacles only.
Methods
This prospective cross-sectional study included 70 male participants (all of Saudi origin). The age of the participants ranged between 20 and 30 years (mean ± SD, 23.2 ± 2.42). The refractive error of the participants varied from -8.00 to +3.00D; no participants had astigmatism values of more than -1.25DC. All participants had corrected visual acuity of 6/6 or better in both eyes. Participants were divided into three groups based on the refractive status of the eye: emmetropia, myopia, and hyperopia. Those with history of CL use, ocular pathology, and ocular surgery were excluded.
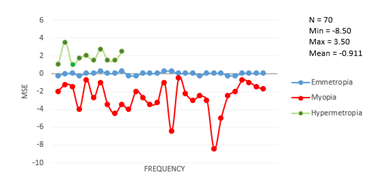
Refractive error and CC were measured using auto keratorefractometer (KR-8100 A, Topcon Inc., Japan). MSE was calculated using the following equations:
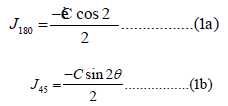
𝐽180 represents from 90° to 180° and 𝐽45 represents from 45° to 135° of astigmatic components [20]. CT, ECD, and coefficient of variation of CV were measured using a specular microscope (SP- 2000 P, Topcon Inc., Japan).
This study was approved by the Research Ethics Committee of King Saud Medical City in Riyadh and was conducted in accordance with the tenets of the Declaration of Helsinki for research involving human participants and current legislation on clinical research. All participants gave their consent for participation before study initiation and were provided verbal explanation followed by information leaflets about the nature of the study.
Statistical Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences version 26.0 (IBM Corp., United States) and Microsoft® Excel® for Microsoft 365. A demographical summary of the data was created using means, standard deviations for frequencies (sample variation), and quantitative variables. A nonparametric approach (Kolmogorov–Smirnov test) was used to assess the distribution of data. Spearman’s correlation coefficient was performed to assess the relationship among quantitative variables, and a two-tailed probability of 0.05 was considered statistically significant. Any data bias was managed using analysis of variance, which aided in determining statistically significant differences among the mean values of the variables.
Results
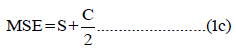
The MSE (mean ± SD) was -2.73 ± 1.77D for participants with myopia and +1.87 ± 0.83 for those with hyperopia. The mean age (mean ± SD) was 23.43 ± 2.41 years for patients with myopia, 23.5 ± 2.31 years for those with emmetropia, and 22.6 ± 2.50 years for those with hyperopia (Table 1).
In the analysis of variables with respect to MSE, there was a
statistical significant difference observed in the CC (r = 0.77, p <
0.05) and ECD (r = 0.34, p < 0.05); however, CV (r = 0.05, p > 0.05)
and CT (r = 0.05, p > 0.05) were not significantly different.
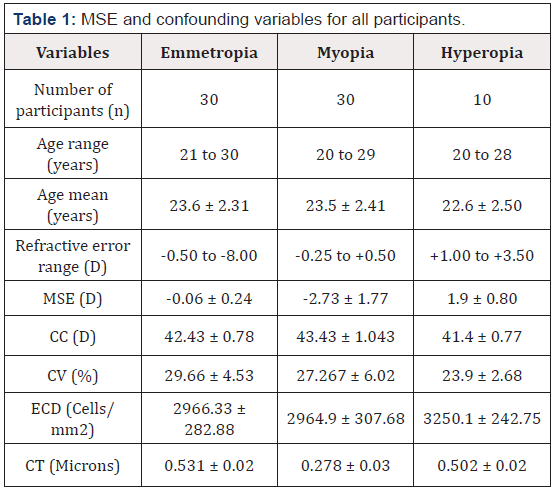
(Figure 1) presents the distribution of MSE and participant
frequency. Normal distribution was observed for the hyperopic
group; however, the values among emmetropic and myopic
participants were poorly distributed.
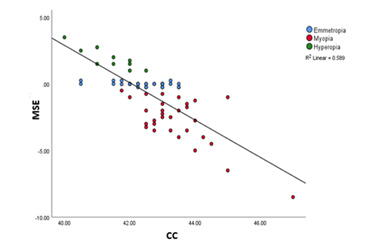
A strong correlation was observed between MSE and CC (r = 0.77, p < 0.05). As expected, myopic participants had a steeper mean CC value (43.43 ± 1.04) than hyperopic (41.4 ± 0.77) and emmetropic (42.43 ± 0.78) participants (Figure 2).
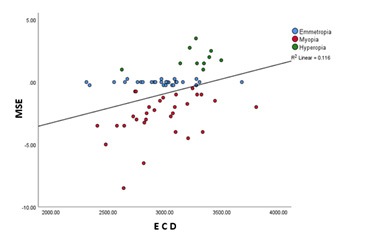
(Figure 3) shows the statistically significant correlation between ECD and MSE (r = 0.34, p < 0.05). Participants with hyperopia had the highest endothelial cell count (3250.1 ± 242.75) compared with those with emmetropia (2966.33 ± 282.88) and myopia (2964.9 ± 307.68).
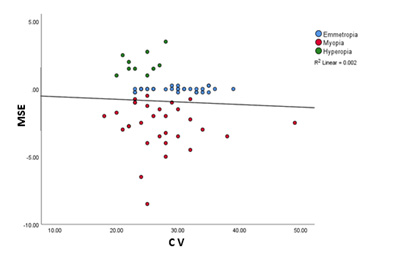
Poorly correlated distribution was observed between CV and MSE (r = 0.05, p = 0.65). Despite having a significant variation in ECD among all groups, the CV values were within the normal range in all participant groups (Figure 4).
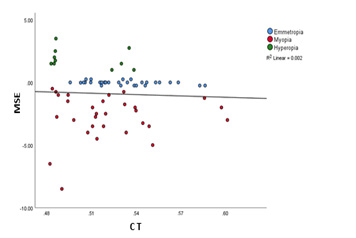
Insignificant distribution of mean CT with respect to MSE was found among all groups (r = 0.054, p = 0.665). The average CT was determined after performing measurements in various quadrants (central, superior, inferior, nasal, and temporal) of the cornea (Figure 5). However, participants in the myopia group had significantly thinner CT (0.278 ± 0.03, p < 0.05), than those in the emmetropia (0.531 ± 0.02) and hyperopia (0.502 ± 0.02) groups.
Discussion
This study explored the association between refractive error and corneal parameters among healthy Saudi Arabian adult men. Variation among CC of the different refractive error groups is one of the most widely studied topics, with numerous publications showing significant correlation values [21]. As mentioned earlier in the text, despite increased steepening in patients with myopia, the anterior corneal surface topography does not vary significantly from its posterior side, with minimal comparative asphericity [12]. The present study shows a similar significant trend with a strong correlation between both parameters (r= 0.77, p < 0.05) (Figure 2). Even though the Although detailed literature explaining such a correlation among Saudi Arabian adults is limited, the usual MSE shift for all groups was significantly correlated with the mean keratometry values. Additionally, the steepening or flattening of CC with the progression of myopia or hyperopia is a known phenomenon, and the shift in refractive error, CC changes, and axial length expansion are always overserved to have a strong correlation in several studies [22,23]. Moreover, a significant number of data points (Figure 2) was concentrated toward low degree refractive error or emmetropia. It can also be postulated that emmetropization is strongly influenced by CC as it tends to keep the progression of refractive error at bay [2,24].
Although there was a poor correlation between the distribution of CV and refractive error, (r = 0.05, p = 0.65) (Figure 4), the correlation between ECD and distribution of CV was significant (r = 0.34, p < 0.05) (Figure 2). Previous article presented a mixed response ECD and CV among different refractive error groups, with some demonstrating reduced ECD ratio in individuals with myopia [25]. The findings of this study were consistent with those of some other studies, who reported low corneal ECD among high myopes with an average age of 22.2 years [26]. However, the variation in ECD among individuals with hyperopia and emmetropia has always been observed to be within the normal range.
The corneal endothelium was studied using the SP-2000 P specular microscope, a highly efficient tool that can determine the ECD and cell morphology with precision, to rule out any abnormalities such as polymegethism [27]. The confounding variables were limited in the present study because the recruited participants were young adults and had no history of CL use or refractive surgery. These variables play a substantial role in ECD variation because the extended use of CL can decrease ECD values and the incidence of polymegethism; moreover, ECD tends to decrease with an increase in age by approximately 0.5% per year among healthy individuals [28].
The recruited sample size can act as a potential risk factor. In the current study, the sample size was small, particularly in the hyperopic group. Previous publications have reported similar variable analyses involving a sample size of ≥100 individuals; this can affect the output values if considered in the future for Arabian individuals [29,30]. Corneal ECD and cell morphology act as decisive factors when considering patients for LASIK eye surgery or CL prescription; these treatment types were reported to significantly alter ECD and CV [16].
Conclusion
MSE is significantly associated with changes in CC and ECD. However, CT and CV were observed to be in the normal range and with a poor correlation with respect to changes in MSE. The current study excluded the extended use of CL, endothelial cell hexagonality, and laser-vision correction-associated parameters; the study considers these confounding variables that significantly affect ECD and CT, irrespective of the magnitude of MSE. Furthermore, this study was limited to male participants, which leaves scope for a comparative analysis in the future involving female participants of the same age group. Inclusion of these parameters would require long-term data collection of Riyadh’s dwellers wearing CLs; this can be explored in future studies.
Acknowledgement
We would like to thank the research center at King Saud Medical City for their valuable support.
Conflict of interest
The authors have declared no conflict of interest.
References
- Wagoner MD, Gonnah E, Towerki AA (2009) Outcome of Primary Adult Penetrating Keratoplasty in a Saudi Arabian Population. Cornea 28(8): 882-890.
- Wildsoet CF (1997) Active emmetropization--evidence for its existence and ramifications for clinical practice. Ophthalmic Physiol Opt 17(4): 279-290.
- Iribarren R, Morgan IG, Chan YH, Lin X, Saw S (2012) Changes in lens power in Singapore Chinese children during refractive development. Invest Ophthalmol Vis Sci 53(9): 5124-5130.
- Karunakar B, Rajlingam, Reddy L, Murthy S, Srikanth (2016) Axial length, corneal curvature and their association with the refractive status of the eye. Journal of Evolution of Medical and Dental Sciences 5(10): 422-426.
- Lin H, Wei C, Chang C, Chen T, Hsu Y, et al. (2016) Role of Chronic Inflammation in Myopia Progression: Clinical Evidence and Experimental Validation. E BioMedicine 10: 269-281.
- Rabin J, Van SRC, Malach R (1981) Emmetropization: a vision-dependent phenomenon. Invest Ophthalmol Vis Sci 20(4): 561-564.
- Mallen EAH, Gammoh Y, Bdour AM, Sayegh FN (2005) Refractive error and ocular biometry in Jordanian adults. Ophthalmic Physiol Opt 25(4): 302-309.
- Kotb M, Eissa SA (2021) Correlation Between Myopic Refractive Error, Corneal Power and Central Corneal Thickness in the Egyptian Population. Clin Ophthalmol 15: 1557-1566.
- Sanders DR, Koch DD (1993) An Atlas of corneal topography. Thorofare NJ, Slack.
- Almudhaiyan T, Alhamzah A, AlShareef M, Alrasheed A, Jaffar R, et al. (2020) The prevalence of refractive errors among Saudi adults in Riyadh, Saudi Arabia. Saudi J Ophthalmol 34(1): 30-34.
- Vergara C, Bomotti SM, Valencia C, Klein BEK, Lee KE, et al. (2018) Association analysis of exome variants and refraction, axial length, and corneal curvature in a European-American population. Hum Mutat 39(12): 1973-1979.
- Hashemi H, Khabazkhoob M, Miraftab M, Emamian MH, Shariati M, et al. (2013) Axial length to corneal radius of curvature ratio and refractive errors. J Ophthalmic Vis Res 8(3): 220-226.
- Ore L, Garozli HJ, Schwartz N, Cohen DM (2014) Factors influencing prevalence of vision and ocular abnormalities among Jewish and Arab Israeli schoolchildren. Isr Med Assoc J 16(9): 553-558.
- Hashmani N, Hashmani S, Hanfi AN, Ayub M, Saad CM, et al. (2017) Effect of age, sex, and refractive errors on central corneal thickness measured by Oculus Pentacam. Clin Ophthalmol 11: 1233-1238.
- Damji KF, Muni RH, Munger RM (2003) Influence of Corneal Variables on Accuracy of Intraocular Pressure Measurement. J Glaucoma 12(1): 69-80.
- Tang M, Li Y, Avila M, Huang D (2006) Measuring total corneal power before and after laser in situ keratomileusis with high-speed optical coherence tomography. J Cataract Refract Surg 32(11): 1843-1850.
- Mirna ŠŠ (2016) RISK FACTORS FOR CONTACT LENS COMPLICATIONS. Zdravniški vestnik 85(2).
- Sheng H, Bullimore MA (2007) Factors Affecting Corneal Endothelial Morphology. Cornea 26(5): 520-525.
- Zeried FM, Alnehmi DA, Osuagwu UL (2020) A survey on knowledge and attitude of Saudi female students toward refractive correction. Clin Exp Optom 103(2): 184-191.
- Thibos NL, Wheeler NW, Horner ND (1997) Power Vectors: An Application of Fourier Analysis to the Description and Statistical Analysis of Refractive Error. Optom Vis Sci 74(6): 367-375.
- Llorente L, Barbero S, Cano D, Dorronsoro C, Marcos S (2004) Myopic versus hyperopic eyes: axial length, corneal shape and optical aberrations. J Vis 4(4): 288-298.
- Ip JM, Huynh SC, Kifley A, Rose KA, Morgan IG, Varma R, et al. Variation of the Contribution from Axial Length and Other Oculometric Parameters to Refraction by Age and Ethnicity. Invest Ophthalmol Vis Sci 48(10): 4846-4853.
- Almahmoud T, Priest D, Munger R, Jackson WB (2011) Correlation between refractive error, corneal power, and thickness in a large population with a wide range of ametropia. Invest Ophthalmol Vis Sci 52(3): 1235-1242.
- Grosvenor T, Scott R (1991) Comparison of refractive components in youth-onset and early adult-onset myopia. Optom Vis Sci 68(3): 204-209.
- Müller A, Craig JP, Grupcheva CN, McGhee CNJ (2004) The effects of corneal parameters on the assessment of endothelial cell density in the elderly eye. Br J Ophthalmol 88(3): 325-330.
- Chang S, Tsai I, Hu F, Lin LL, Shih Y (2001) The cornea in young myopic adults. Br J Ophthalmol 85(8): 916-920.
- Cheung SW, Cho P (2000) Endothelial cells analysis with the TOPCON specular microscope SP-2000P and IMAGEnet system. Curr Eye Res 21(4): 788-798.
- Racz A, Toth GZ, Tarnoki AD, Tarnoki DL, Littvay L, et al. (2016) The inheritance of corneal endothelial cell density. Ophthalmic Genet 37(3): 281-284.
- MacRae SM, Matsuda M, Yee R (1985) The effect of long-term hard contact lens wear on the corneal endothelium. CLAO J 11(4): 322-326.
- Setälä K, Vasara K, Vesti E, Ruusuvaara P (1998) Effects of long-term contact lens wear on the corneal endothelium. Acta Ophthalmol Scand 76(3): 299-303.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.