Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Bacilliferous Tuberculosis in Children
*Corresponding author: Dr. Shujaat Ali Khan, Department of Pharmacy, COMSATS University Islamabad-Abbottabad Campus, Khyber Pakhtunkhwa, Pakistan.
Received: November 11, 2021; Published: November 29, 2021
DOI: 10.34297/AJBSR.2021.14.002051
Abstract
Tuberculosis poses a real public health problem in the world and particularly in Africa where there is a high burden of morbidity and mortality. We here report a case of sensitive tuberculosis in a 2-year-old child hospitalized at the Medical Center of the company RVA. Thus, the screening of children exposed to an adult with smear-positive tuberculosis is an important element in allowing early management.
Keywords: Child; Tuberculosis; Bacilliferous
Introduction
Tuberculosis is a real public health problem in the world and particularly in the Democratic Republic of Congo (DRC) which is among the countries with an incidence ≥ 30 cases / 100,000 inhabitants / year. It is ranked second in Africa in terms of the burden of tuberculosis and ninth globally [1]. The World Health Organization estimates that globally 10 million people contracted tuberculosis in 2019, 5.6 million men, 3.2 million women and 1.2 million children [1].
Tuberculosis is passed from person to person through the air, and a patient with pulmonary tuberculosis, coughing, sneezing or spitting, projects tuberculosis bacilli into the air. However, it only takes another person inhaling a few of these bacilli for them to become infected [1-10]. Among people infected with the tuberculosis bacillus, the risk of developing the disease at any time in life is between 5 to 15% and a person with active untreated tuberculosis can infect up to 15 others in a year. [1-3].
The disease is often not recognized by caregivers in children and adolescents and it can be difficult to diagnose and treat with consequences for the health of the child [1-2]. Fortunately, since 2006, the specific challenges of tuberculosis in children have received increasing attention and the importance of the phenomenon as a public health problem has been increasingly recognized worldwide. Although most children with tuberculosis are not necessarily the cause of significant spread of the disease in the population, tuberculosis remains a significant contributor to infant morbidity and mortality [1-6].
This is why its early detection is necessary to stop the spread of the germ in the population and ensure better case management. Thus, the management of children with tuberculosis must comply with the Stop TB strategy, taking into account the peculiarities of the epidemiology and clinical forms of tuberculosis in children.
Patient and Observation
The 2-year-old male child had consulted at the Medical Center of the company RVA for a prolonged cough and fever that had progressed for 4 weeks, night sweats and weight loss. His background reveals that he was born quietly, weighing 2,800kg. The child was breast fed and with cow’s milk. He is 3rd in the family and the vaccination schedule is well respected. Her father is employed in a state company and her mother is a housewife. The history of her illness dates back to 4 weeks of the consultation for the general signs mentioned above. He was treated successively with Clamoxyl, Bactrim, Cefuroclav and Palucur without improvement.
Paraclinical Examinations
Paraclinical examinations showed the following elements: A sedimentation rate at 65 mm / h, CRP at 48 mg, Intradermal reaction to tuberculin (IDRT) at 10 mm, leukocytosis at 22 350 / mm3, the predominantly neutrophilic leukocyte formula (80% ) and lymphocytes at 20%, platelets at 200,000 / mm3, Hemoglobin at 9 mg%, SGOT at 25 US and SGPT at 18 US, urea at 24 mg / dl and Creatinine at 0.6 mg / dl, HIV serology orientation (To determines and Double Cheick) negative, Ziehl on sputum and gastric tubing fluid positive with two crosses in the different samples taken. The Gen-Xpert MTB / RIF sample came back positive with sensitivity to Rifampicin. Culture on Lowenstein Jensens’ medium came back positive and Mycobacterium tuberculosis was isolated by the third week of incubation. The strain was sensitive to Rifampicin, Isoniazid, Ethambutol and Streptomycin.
Diagnostic
The diagnosis was smear-positive tuberculosis Treatment The child was given anti-tuberculosis drugs according to the recommendation of the National Tuberculosis Control Program, namely: Rifampicin, Isoniazid and Pyrazinamide during the intensive phase (2 months) and Rifampicin and Isoniazid for four months in the treatment phase continuation (4 months).
Evolution
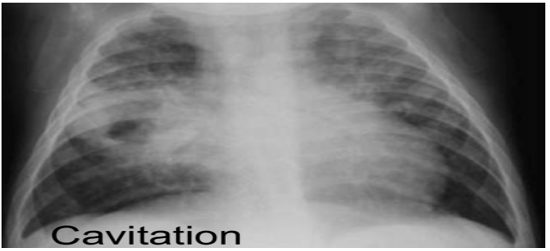
Contact case tracing was carried out with all the people who lived in the same house with a view to locating other cases. However, analyzes performed on contacts was negative so far. Regarding the evolution in the child, a drop in fever and cough were noticed at the second week of treatment, as well as the negativation of the Ziehl examination on gastric tubing fluid only because the child no longer coughed. The sedimentation rate and CBC returned to normal at the 2nd, 3rd and 5th month of monitoring. We also noticed a weight gain (2Kg). In contrast, the X-ray image could be superimposed on the first to the second month of treatment and normalized at the end of anti-tuberculosis treatment.
Discussion
The urgency of the problem posed by childhood tuberculosis must be given special attention to allow better case management. The disease being contagious requires rapid and early diagnosis to reduce the risk of contamination to those around it. The source of contamination in a child is above all an adult who is often bacilliferous [1-6]. This was the case for this child infected by his mother who also had smear-positive tuberculosis. This observation agrees with that reported by Aketi
Chemlal
Thus, the intensity of the exposure depends on the proximity and repetition of contact, in particular sharing the same home (intra-family contact) [4-14]. Another important factor is the patient’s age which is the factor in the immediate progression to the disease. The World Health Organization (WHO) shows that this risk is greatly increased in children under 2 years of age with a risk of developing the severe form of tuberculosis and this can persist until the age of 5 [1-2]. Thus, the child is a subject at risk by his relative fragility and its permanent contact with adults, which is a predilection for tuberculosis [1-5].
Tuberculosis is therefore a major cause of morbidity and mortality throughout the world and it is a global public health problem. The WHO reports that every day, nearly 400 children die from tuberculosis, which is nevertheless a preventable and curable disease if and only if all the means are available for its detection and correct management [1-2].
Unfortunately, it often happens that tuberculosis goes unnoticed because of the unspecific symptoms of the disease in children and the difficulties of diagnosis which lead to treatment, which is often inadequate. However, the adoption of the Stop TB Strategy in 2006 made it easier to prioritize actions in favor of the most vulnerable populations, especially children, and by strengthening case-based care [1-3].
Investigation shows that despite the vaccination, the child developed tuberculosis. This is not a new fact; several surveys have already shown that being vaccinated does not prevent an individual from developing tuberculosis [4-8]. However, we know that it would reduce the occurrence of severe and / or disseminated forms of tuberculosis (meningitis, miliary and pericarditis) in children [2-16]. WHO and certain authors such as Monia Khcmiri and [12]. Tidjani
The general signs encountered in our investigation, (Long-term fever, cough for more than 4 weeks, anorexia, night sweats and weight loss) including the concept of T-counting, made it possible to suspect tuberculosis in the child. This observation is in line with those of Yousra LANDA
In addition, the bacteriological examinations showed a positive bacilloscopy, a positive culture on the medium of Lowenstein Jensens and the identification made it possible to determine the strain of Mycobacterium tuberculosis, sensitive to all the anti-tuberculosis drugs tested. Gen-Xpert MTB / RIF revealed tuberculosis sensitive to Rifampicin. These results were made possible by the analysis of spontaneous sputum and gastric tubing fluid obtained from the child. Aketi L.
Conclusion
Tuberculosis is a real public health problem in the country and contact tracing of tuberculosis cases is very important in children who are often in close contact with adults as the disease continues to contribute to infant morbidity and mortality.
Conflicts of Interest
The authors declare no conflict of interest.
Contributions from the Authors
All the authors contributed to the conduct of this work. All authors also declare that they have read and approved the final version of the manuscript.
References
- (2019) Who Rapport global sur le contrôle de la tuberculose.
- (2016) Who Lignes directrices concernant la prise en charge de la tuberculose chez l’enfant dans le cadre des programmes nationaux. Disponible sur internet à.
- Rapport AE (2019) HCSCP Infections tuberculeuses latentes: détection, prise en charge et surveillance. Disponible sur inssternet à v 1-88.
- Getahun H, Matteelli A, Chaisson RE, Raviglione M (2015) Latent Mycobacterium tuberculosis infection. N Engl J Med 372(22): 2127-2135.
- Perez Velez CM, Marais BJ (2012) Tuberculosis in children. New England Journal of Medicine, 367(4): 348-361.
- Graham SM (2011) The use of diagnostic systems for tuberculosis in children. Indian Journal of Pediatrics78(3): 334-339.
- Bates M, O'Grady J, Maeurer M, Tembo J, Chilukutu L,
- et al.
(2013) Assessment of the Xpert MTB/RIF assay for diagnosis of tuberculosis with gastric lavage aspirates in children in sub-Saharan Africa: a prospective descriptive study. Lancet Infectious Diseases 13(1): 36-42. - Nicol MP, Workman L, Isaacs W, Munro J, Black F,
- et al.
(2011) Accuracy of the Xpert MTB/RIF test for the diagnosis of pulmonary tuberculosis in children admitted to hospital in Cape Town, South Africa: a descriptive study. Lancet Infectious Diseases 11(11): 819-824. - (2016) Programme national de lutte contre la Tuberculose. Programme antituberculeux intégré aux soins de santé de base, 5ème é
- Aketi L, Engo A, Lumbala P, Kasongo S, Lulute E, (2008) Tuberculose pulmonaire bacillifère chez un petit nourrisson. Archives de Pédiatrie 15: 1611-1613.
- Elfihri S, Amor JB, Zahraoui R, Marc K, Soualhi M, et al (2014) Chemlal Mouna. Aspect diagnostic de la tuberculose de l'enfant expérience del'hôpital Molay Youssef. Thèse doctorat Médecine, Rabat; 34, N°
- Khemiri M, Labessi A, Zouari S, Borgi A, Ben Mansour F,
- et al.
(2009) Tuberculosis in childhood: clinical features and problems in diagnosis. Report of 30cases. Tunis Med 87(1): 61-67. - OuédraogoNugbaré SO, Ouali, Diabouga S, Moyenga I, Bouda C, et al (2015) Morbidité et tàcteurs de risque de décès de la tuberculose de l'enfant à Ouagadougou (Burkina Faso). Médecine d'Afrique Noire 6204 - Avri120l5. 215-225.
- Lewinsohn DM, Leonard MK, LoBue PA, Cohn DL, Daley CL, et al (2017) Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention clinical practice guidelines: Diagnosis of tuberculosis in adults and children. Clin Infect Dis 64(2): 111-115.
- Laurenti P, Raponi M, Waure CD, Marino M, Ricciardi W,
- et al.
(2016) Performance of interferon-ƴ release assays in the diagnosis of confirmed active tuberculosis in immunocompetent children: A new systematic review and meta-analysis. BMC Infect Dis 16:131. - Tidjani O, Grunttlky B, Tatagan K, Kassan Kognon Y, Fillastre C, (1988) Efficacité du B.C.G. dans la prévention de la tuberculose de l'enfant. Communication Rencontre Franco-Africaine de Pédiatrie JP P 19: 224.
- Landa Y (2015) Épidémiologie de la tuberculose de l'enfant à l'hôpital d'enfant entre2008 et 2013. Université CADI AYYAD Faculté de médecine et de pha11l1acie deMARRAKECH Thèse doctorat Médecine, MalTakech 114: 34-35.
- Kouéta F, Ouédraogo G, Dao L, Néboua D, Yé D (2011) La tuberculose chez les enfants infectés par le VIH suivi à Charles de Gaulle l'hôpital universitaire de pédiatrie de Ouagadougou (BF). Mali Med 26(4): 44-49.
- Aketi L, Kashongwe Z, Kinsiona C, Fueza SB, Kokolomami J, et al : Tuberculose de l'enfance dans une facilité tertiaire sous saharienne: épidémiologie et facteurs associés avec le résultat de traitement.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.