Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Diagnosis of Recurrent Prostate Cancer at MRI Following Radiation Therapy
*Corresponding author: Jinxing Yu, Department of Radiology, Virginia Commonwealth University, Health System Main Hospital, USA.
Received: November 09, 2021; Published: November 15, 2021
DOI: 10.34297/AJBSR.2021.14.002037
Introduction
Prostate cancer (PCa)recurrence following radiation therapy (RT) is a significant issue. Despite advances in diagnosis and management of PCa, the disease still recurs after definitive treatment in up to 30% of patients [1]. Early diagnosis of local recurrence is strongly associated with improved patient prognosis because of prompt treatment decisions based on the diagnosis. It is approximately 3 years from development of local recurrence to distant metastasis on average if without salvage therapy [2]. According to the Phoenix criterion, after RT, biochemical recurrence (BCR) is defined as an absolute increase in PSA level of 2 ng/ml above nadir (i.e., the lowest post-treatment PSA value) [3,4]. The recurrence may be local, nodal and/or metastatic. A rising serum prostate-specific antigen (PSA) level is typically the first sign of relapse, unfortunately it does not differentiate local recurrence from systemic disease. If PSA doubles in less than 8 months, especially in the first year after treatment, this can be a predictor for metastatic disease [5]. Since there is no reliable way to diagnose local recurrence clinically, imaging is needed to determine if there is a local recurrence. Fortunately, recent advances in multiparametric MRI (mp-MRI) techniques have markedly improved detection of local recurrence following RT [6]. The majority of post-RT recurrences have been shown to be local, with the most common site of recurrence being the prostate. Therefore, in the follow up of BCR in these patients, evaluation with prostate mp-MRI is essential [7]. Most local recurrences exhibit specicifc features at mp-MRI that make them readily detectable [7,8]. The purpose of this mini review is to provide an overview of the MRI features of locally recurrent PCa following RT, emphasizing the key MRI features that will lead to make a definitive diagnosis of local recurrence.
Key Features of Recurrent PCa Following RT at mp-MRI
Up to 40% of patients over 65 years old and 25% of patients under 65 years old would choose RT as the definitive treatment for PCa [9]. RT can be offered as external-beam RT (EBRT) or brachytherapy. Through multiple portals, external-beam RT involves the use of ionizing radiation directed at the prostate and surrounding tissues. Most modern methods in EBRT allow for highly targeted radiation with reduced dose to normal tissue by delivering photons or protons using advanced computer-based planning systems. Photons and protons each have their distinct advantages and disadvantages. Proton therapy with a higher cost delivers a lesser dose. In order to improve survival, 2–3 years of post-radiation adjuvant hormonal therapy is administered for patient with high-risk disease [6]. Either short-course hormonal therapy and standard dose EBRT or dose escalation should be considered standard for patients with intermediate-risk disease. Brachytherapy delivers a high dose of radiation to the tumor while sparing the bladder and the rectum by implanting radioactive sources (seeds or needles) directly into the prostate gland.
Recurrent PCa in Patients After External-BeamRT
The differentiation of the zones of the prostate is effaced in the irradiated prostate which is smaller as a result of gland atrophy [10]. The entire prostate is hypointense on T2W imaging, further complicating differentiation between benign versus malignant tissue [11]. Accurate localization of focal recurrence is essential for possible salvage radiation therapy. The location of the recurrence at the region of the primary tumor occurs more than 90% of time [12,13]. Even though malignant tumors are still most often recognized as lesions of relatively lower T2 signal intensity than that of surrounding noncancerous prostate, unfortunatelyT2W imaging has marked limitations. Since the post-radiation gland fibrosis is less cellular and has diminished vascularity compared to pre-treatment prostate tissue, DWI and DCE appearance of the prostate is impacted as well after RT. However, the functional sequences of mp-MRI still play a more dominant role in detection of post-RT recurrence because changes on DWI and DCE are not as drastic as on T2W. On DWI, signal characteristics of post-RT recurrence are focal hypo intensity on the ADC map, hyperintensity on high b-value DWI and a nodular area on corresponding T2W imaging, very similar to the characteristics of primary PCa. The vascularity of the irradiated prostate decreases with gland atrophy, but recurrent tumors can retain their highly vascular network [14]. Therefore, recurrence will have early hyperenhancement relative to the treated prostate on DCE imaging. If a focal, early enhancement at MRI correlates with abnormalities on T2 and DWI, the finding is particularly suspicious for recurrent PCa [15].
Recurrent PCa in Patients After Brachytherapy
Following brachytherapy, post-treatment changes to the prostate are very similar to those seen after EBRT, with the additional finding of visualization of the radioactive seeds used. Brachytherapy seeds can distort images by introducing MR susceptibility artifacts, particularly on DWI, making interpretation difficult. Since the majority of the patients with brachytherapy have low-risk primary disease, recurrence is less of a concern than it is after EBRT. On T2W imaging, the brachytherapy seeds appear as small, hypointense, ellipsoid structures scattered throughout the prostate. The seeds gradually migrate peripherally within the gland as it shrinks in size. Following brachytherapy, the most common site of recurrence is at the location of the original tumor, which is similar to EBRT. A rapid focus of hyperenhancement on DCE imaging, corresponding a hypointense nodule on T2W imaging with paucity of radiation seeds nearby, with or without associated diffusion restriction are imaging characteristics for suspicion of local recurrence [16]. In recent years, a new form of temporary high dose rate (HDR) brachytherapy has been offered. Since the seeds in HDR brachytherapy are removed, image quality does not suffer from susceptibility artifacts related to the seeds. The data validating the use of mp-MRI post-HDR is limited because HDR is relatively new and BCR post-brachytherapy occurs less frequently. T2WI sensitivity in detecting the recurrence is limited due to the background changes in the gland. In this setting with the removal of seeds, DWI is not compromised, showing high sensitivity for detection of recurrence. At DCE, early hyperenhancement remains very important for the diagnosis of recurrent PCa [17].
Conclusion
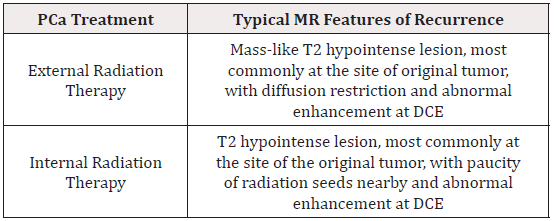
MR imaging plays an important role not only in initial staging of PCa but also in evaluation for suspected recurrent disease following RT. Radiologists should be comfortable with interpretation of mp- MRI for both indications. Recognizing the typical appearance of post treatment changes and distinguishing them from the MR features of recurrent cancer are very important in making a correct diagnosis, which plays an uttermost role in clinical management and potential prompt treatment of PCa Recurrence (Table 1).
Conflict of Interest
Authors declare that no conflict of interest exist in this paper.
Acknowledgement
None
References
- Babaian RJ, Troncoso P, Bhadkamkar VA, Johnston DA (2001) Analysis of clinicopathologic factors predicting outcome after radical prostatectomy. Cancer 91(8): 1414-1422.
- FJ Bianco, PT Scardino, AJ Stephenson, CJ DiBlasio, PA Fearn, et al. (2005) Long term oncologic results of salvage radical prostatectomy for locally recurrent prostate cancer after radiotherapy. International Journal of Radiation Oncology, Biology, Physics 62(2): 448-453.
- Kuban DA, Levy LB, Potters L, David C Beyer, John C Blasko, et al. (2006) Comparison of biochemical failure definitions for permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys 65(5): 1487-1493.
- Cheung R, Tucker SL, Lee AL, Lei Dong, Ashish Kamat, et al. (2005) Assessing the impact of an alternative biochemical failure definition on radiation dose response for high-risk prostate cancer treated with external beam radiotherapy. Int J Radiat Oncol Biol Phys 61(1): 14-19.
- Zagars GK, Pollack A (1997) Kinetics of serum prostate-specific antigen after external beam radiation for clinically localized prostate cancer. Radiother Oncol 44(3): 213-221.
- Mertan FV, Greer MD, Borofsky S, Ismail M Kabakus, Maria J Merino, et al. (2016) Multiparametric Magnetic Resonance Imaging of Recurrent Prostate Cancer. Top MagnReson Imaging 25(3): 139-147.
- Vargas H, Wassberg C, Akin O, Hricak H (2012) MR Imaging of Treated Prostate Cancer. Radiology 262(1): 26-42.
- Stephenson AJ, Kattan MW, Eastham JA, Zohar A Dotan, Fernando J Bianco, et al. (2006) Defining biochemical recurrence of prostate cancer after radical prostatectomy: a proposal for a standardized definition. J Clin Oncol 24(24): 3973-3978.
- Siegel R, DeSantis C, Virgo K, Kevin Stein, Angela Mariotto, et al. (2012) Cancer treatment and survivorship statistics,2012. CA Cancer J Clin 62(4): 220-241.
- Sugimura K, Carrington BM, Quivey JM, Hricak H (1990) Postirradiation changes in the pelvis: assessment with MR imaging. Radiology 175(3): 805-813.
- Chan TW, Kressel HY (1991) Prostate and seminal vesicles after irradiation: MR appearance. J MagnReson Imaging 1(5): 503-511.
- Arrayeh E, Westphalen AC, Kurhanewicz J, Mack Roach , Adam J Jung, et al. (2012) Does local recurrence of prostate cancer after radiation therapy occur at the site of primary tumor? Results of a longitudinal MRI and MRSI study. Int J Radiat Oncol Biol Phys 82(5): 787-793.
- Jalloh M, Leapman MS, Cowan JE, Katsuto Shinohara, Kirsten L Greene, et al. (2015) Patterns of Local Failure following Radiation Therapy for Prostate Cancer. J Urol 194(4): 977-982.
- Franiel T, Ludemann L, Taupitz M, Bohmer D, Beyersdorff D (2009) MRI before and after external beam intensity-modulated radiotherapy of patients with prostate cancer: the feasibility of monitoring of radiation-induced tissue changes using a dynamic contrast-enhanced inversion-prepared dual-contrast gradient echo sequence. Radiother Oncol 93(2): 241-245.
- Barchetti F, Panebianco V (2014) Multiparametric MRI for recurrent prostate cancer post radical prostatectomy and postradiation therapy. Biomed Res Int 2014: 316272.
- Rouviere O, Vitry T, Lyonnet D (2010) Imaging of prostate cancer local recurrences: why and how? Eur Radiol 20(5): 1254-1266.
- Tamada T, Sone T, Jo Y, Atsushi Higaki, Hiroki Higashi, et al. (2011) Locally recurrent prostate cancer after high-dose-rate brachytherapy: the value of diffusion-weighted imaging, dynamic contrast-enhanced MRI, and T2-weighted imaging in localizing tumors. AJR Am J Roentgenol 197(2): 408-414.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.