Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Family-Centered Music Therapy with Preterm Infants in Perception of their Parents
*Corresponding author: Susann Kobus, Essen University Hospital Clinic for Pediatrics I, Hufelandstr. 5545147, Essen, Germany
Received: October 12, 2021; Published: October 21, 2021
DOI: 10.34297/AJBSR.2021.14.002009
Abstract
Premature birth places considerable demands on preterm infants and their families. Almost all these children must stay in a neonatal intensive care unit immediately after their birth, which means that the parents are exposed to increased psychosocial stress. Building a stable parent-child bond is often difficult due to the special situation. We hypothesized that an accompaniment with live music therapy by a qualified music therapist supports the parents in building relationships with their preterm infant. Forty preterm infants born with a gestational age less than 32 weeks received music therapy twice a week until they were discharged from the hospital. At the time of discharge, the parents completed a questionnaire to evaluate the effectiveness of the music therapy. We saw that 94% of the parents were able to relax during the music therapy session. Many parents also noticed their children in a relaxed behavior during (91%) and after (88%) music therapy. The music therapy care was perceived by the parents as a positive change and enrichment in the hospital stay. All parents were thankful for the music therapy they received.
Keywords: Music Therapy; Preterm Infants; Neonatal Intensive Care Unit; Premature Infants; Parents; Family; Family-Centered; Pregnancy; Brain; Organ; Medical; Retinopathy
Introduction
Premature infants are born before the end the 37th week of pregnancy. Every year about 15 million children around the world are born prematurely and the trend is increasing [1]. Although premature infants are not primarily ill, organ immaturity can lead to various medical problems. This mainly affects the brain, heart, kidneys, lungs, intestines, and immune system, making the children susceptible to complications such as respiratory distress syndrome, chronic lung diseases, intestinal injuries, weakened immune system and cardiovascular diseases [2]. Medical care for premature infants has improved significantly in recent years, so that children who are born immaturely can survive. However, premature infants with a gestational age of less than 28 weeks of gestation still have a high risk of morbidity and mortality [3]. Due to premature birth, they suffer a higher incidence rate of respiratory distress syndrome (IBS), Necrotizing Enterocolitis (NEC), Intraventricular Hemorrhage (IVH), Bronchopulmonary Dysplasia (BPD) and Premature Retinopathy (ROP). As a result, long-term survival rates before 1970 were usually below 10% [4].
And about a quarter of the infants born extremely prematurely in the 1990th had a serious disability in pre-school age, such as impaired intellectual development, cerebral palsy, blindness, or deafness [5]. In recent years, the development of extremely premature infants has greatly improved due to tremendous advances in perinatal care, including prenatal steroids, surfactant replacement therapy, non-invasive ventilation, nutritional therapy, and an increase in active treatment [6]. Premature infants have an increased long-term development risk. After a decrease in serious brain damage such as cerebral haemorrhage and oxygen supply, microscopic abnormalities of the white matter dominate today, which are accompanied by an expansion of the inner and outer liquor spaces and a variable involvement of the cortical and deep gray matter [3]. The cerebellum of babies born prematurely American Journal of Biomedical Science & Research Copy@ Susann Kobus 341 differs significantly from babies born on time, even at the time of the calculated due date. Infections, cerebellar injuries, and supratentorial injuries are important risk factors for impaired cerebellar biochemistry in premature infants [7]. These changes in brain development are therefore multifactorial but can be positively influenced by music therapy [8]. From a gestational age of 26 weeks, the human fetus begins to perceive auditory stimuli [9].
The maturation of the auditory system is influenced by the acoustic environment and is the basis for later language development, learning and memory formation [10]. Before birth, the child is embedded in the intrauterine sound environment. In addition to the noises of the mother’s organism, such as the heartbeat, breathing and digestive noises, the unborn child experiences sound, voices, and noises from the outside world. The womb is the best environment for the mental and physical development of the child, especially about the quality, intensity, and duration of all stimuli [11]. If the child is born too early, the child is withdrawn from this beneficial environment prematurely and transferred to the unpredictable neonatal in- tensive care unit, which is determined by technical noises. Here, the child is offered many stimuli too early [12]. The premature infant is exposed to the low-frequency noises of the incubator and noise such as the highfrequency beeping of the monitor alarm repeatedly penetrates the unprotected ear [13]. On the one hand, intensive care medicine ensures the survival and growth of the child; on the other hand, the unphysiological stimuli can represent immense stressors for the not yet fully developed sensory organs of the unstable child [14]. But not only the premature infant itself, but also its parents are exposed to a special, especially emotional, stress.
The normal establishment of a parent-child bond is made more difficult by the fact that the child is first given medical care after birth and the parents see it connected to cables at first sight. In addition to the external frame-work conditions of a neonatal intensive care unit, parental fears make it more difficult to build bonds between parents and children and can have a negative impact on the development of the child [15,16]. Nevertheless, parents play a central role in promoting the development of premature infants. Their inclusion in the care is now considered a necessary part of the treatment of premature babies [17]. The care for premature infants has changed significantly in the last few decades, not only due to enormous medical advances, but also to expanded psychosocial care. With the G-BA decision, politicians recognize the need for family-centered care [18]. In the perinatal center of the University Hospital Essen there has been family-centered care since 2007 by the parent advisory service “Frühstart”. The parents of premature infants and ill newborns are cared for from high-risk pregnancy to home. Since 2016, creative, family-centered music therapy has also been offered for premature infants. It serves as a means of interaction, as a non-verbal form of communication and to promote the child’s individual development [19].
In addition, it actively strengthens parents in looking after their children [11]. A qualitative study with premature born before 32 weeks’ gestation showed that creative music therapy can support the parent-child relationship. The musical interaction evoked feelings of joy and relaxation in the parents and encouraged them to interact more deeply with their child. There are also effects on the children. Music therapy has a stabilizing and relaxing effect on the general behavior of premature infants as well as on physiological parameters and sleep patterns [20-23]. Some of these positive effects can already be seen during the intervention [24]. Live music therapy has a stabilizing effect on vital functions and is also effective during sleep [25]. It has recently been shown that live music therapy influences the functional brain activity and even the brain structure in premature infants [8]. Based on the previous findings in the field of family-centered work with premature infants in an inpatient setting and the research results in family-centered music therapy, we examined how parents perceived the in-patient family-centered music therapy care of their premature infants, born before 32 weeks’ gestation.
Materials and Methods
Study Design
The results of the parent survey presented here are part of a prospective, randomized controlled clinical study with music therapy in premature infants less than 32 weeks of gestation. Infants were randomly assigned to either music therapy (intervention group) or no music therapy (control group). There were no differences between the groups in medical care. All parents whose child was randomized into the intervention group received the questionnaires evaluated here before discharge.
Eligibility and Recruitment
Infants born before 32 weeks’ gestation at the University Hospital Essen between October 2018 and May 2021 were eligible for the study. Parental informed consent was obtained during the first week of life, at a minimum age of 72h. Because the study was designed to examine the neurodevelopment outcome later in the course, exclusion criteria were congenital hearing disorders, periventricular haemorrhagic infarction, cerebral malformations, and underlying diseases that impair neurological development. The study was approved by the local ethics committee of the Medical Faculty of the University of Duisburg-Essen (18-8035-BO).
Intervention
In all clinically stable patients in the intervention group, a music therapy session was performed twice a week from the second week of life until discharge. The timing of each therapy session was agreed between the music therapist, the nursing staff, and the parents. During the therapy the child remained in the same position as before therapy, e.g., the incubator, heated cod or parent’s arm or breast during kangaroo care. The parents could be present during the intervention; this was explicitly requested, but not a condition. The sessions consisted of child-directed low humming and the increasing use of the sansula. The sansula, consisting of a wooden ring covered with a drum skin, on which a small kalimba is attached, creates a room-filling, long-lasting and soft sound. This sound and the vibrations are transmitted through the sound membrane. If the sansula is held with the underside in the direction of the child while plucking the sound tongues, a feeling of being enveloped in the sound can arise. Before and after each therapy session, the vital parameters (heart rate, respiratory rate, and oxygen saturation), the wakefulness and the behavior of the children were documented. The music therapy was prepared and carried out for each individual child and did not involve music in the entire intensive care room. The therapy was designed slowly and with many breaks to give time to the premature infants to process their sensory perceptions.
Questionnaires
At the time of discharge, the parents filled out a questionnaire on the parents’ perception of the effectiveness of the music therapy, which was answered anonymously, without naming them. The parents put the completed questionnaire in the mailbox of the parent advisory service on the neonatal station. It took about five minutes to fill out the questionnaire. The first part of the questionnaire contains fourteen questions about music therapy support during the inpatient stay. Sociodemographic characteristics were recorded in further six questions.
Statistical Analysis
The socio-demographic characteristics of the parents of the therapy group were given as absolute frequencies and in percent, and the variables of the written survey in percent. All graphic and tabular representations were created with Microsoft Excel.
Results
Patients
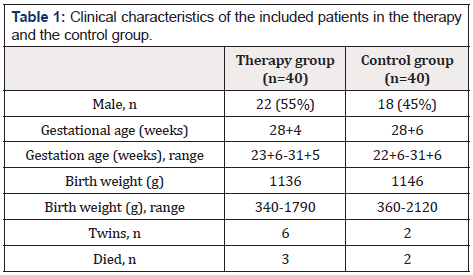
During the study period, 144 premature infants were born before 32 weeks’ gestation at the University Hospital Essen. Eighty premature infants were included in the study, 40 in the therapy group and 40 in the control group. Clinical data of the patients included in the therapy and control groups are shown in Table 1. 64 premature infants were not included. The reasons for not including were birth in another hospital (n=3, 5%), death before recruitment (n=11, 17%), transfer to another hospital (n=4; 6.0%), cerebral haemorrhage °III (n=3; 5%), critical illness or death of the mother (n=2; 3%), insufficient knowledge of German to understand the study objective (n=3; 5%), inpatient stay during the study stop within the corona pandemic (n=6; 9%) and a lack of interest in participating (n=32; 50%).
Questionnaires
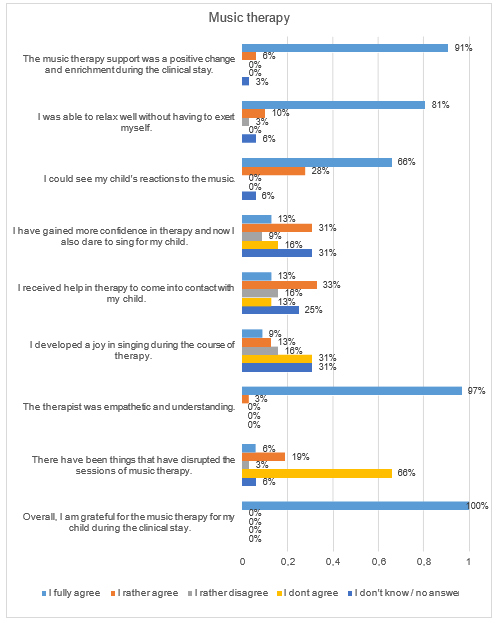
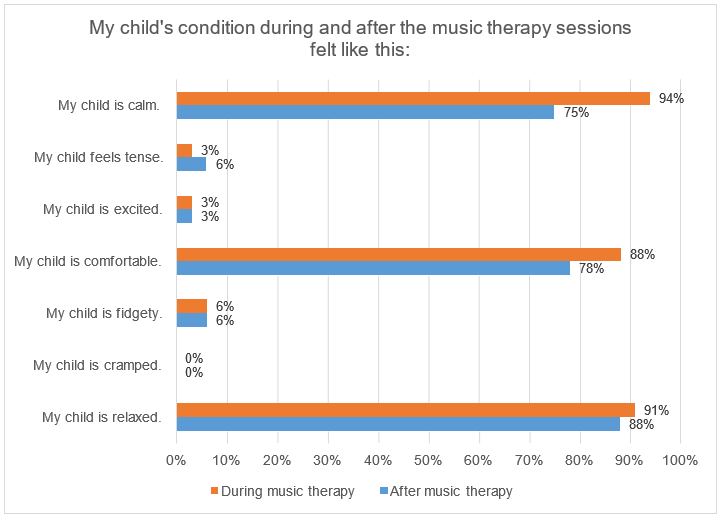
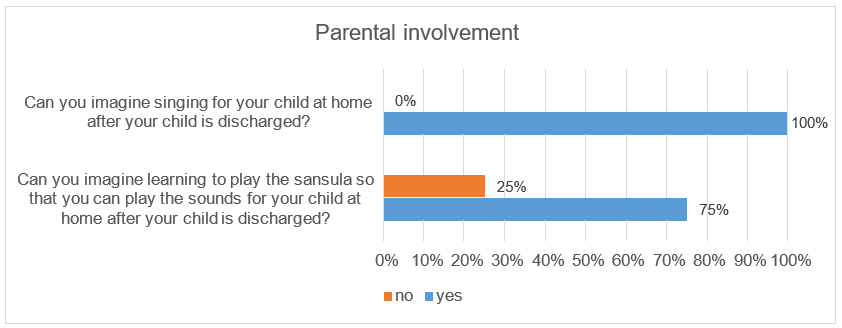
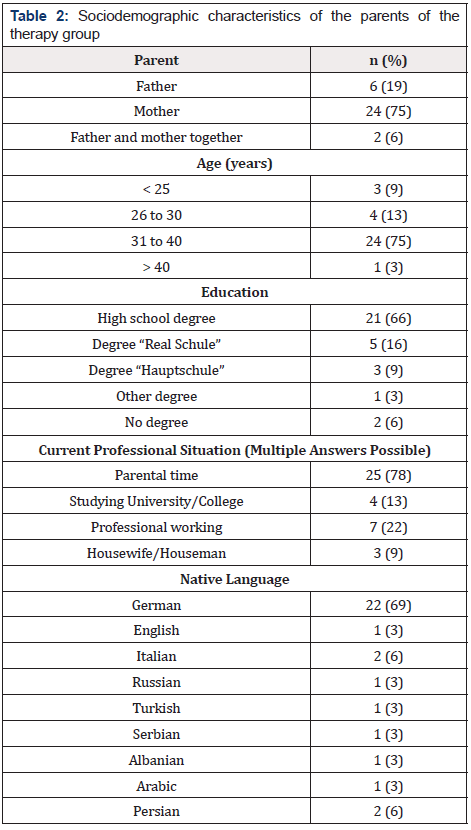
We received 32 completed questionnaires from the parents of the 40 children in the therapy group. Three children died during their inpatient stay and no questionnaire was filled out form parents of five other children. Sociodemographic characteristics of the parents who completed a questionnaire are shown in Table 2. The answers of the questionnaires showed that the parents perceived the music therapy support positively (Figure 1). 100% of the responding parents said that they were grateful for the music therapy they received. 94% of the parents at the University Medicine Essen stated that they could observe their child’s reactions to the music during the music therapy interventions. These included smiling, grimacing, blinking, making little voices, pacifying, lounging and deep breaths. During music therapy, 94% (n=30) of the parents found their child calm, in 75% (n=24) this continued even after music therapy. Likewise, 91% (n=29) of the children looked relaxed for their parents during music therapy and 88% (n=28) of the children also after music therapy (Figure 2). In our study, 88% (n=28) of the parents stated that their child felt comfortable during the music therapy and 78% (n=25) of the parents were able to observe this even after the music therapy. Overall, 94% (n=30) of the parents said that the music therapy was good for their child and 78% (n=25) for them too. All parents said that they can imagine singing for their child after they have been discharged and 75% of parents can also imagine learning to play the sansula Figure 3.
Discussion
This study shows that parents of premature infants perceive family-centered music therapy positively in terms of their own well-being and that of their child. The relaxing effect during the music therapy intervention played the most important role for the parents. The music therapy support was perceived by all parents as a positive change and enrichment during their hospital stay, so that everyone was grateful for the additional therapeutic offer. Relaxation is also necessary to promote bonding [14,26], because the parents’ access to their child can be made more difficult by increased stress. This prevents parents from correctly interpreting their child’s signals and from reacting to them accordingly. Due to the concern for their own child, parents do not always succeed in relaxing, especially in the early days [27,28]. Music therapy can (re) establish well-being and lead to relaxation [29]. By listening to the sansula during music therapy, the ambient noise is perceived to be reduced, which causes calming and relaxation. Most of the parents in our study (94%) said that they could relax easily during music therapy. Many parents also perceived their children to be relaxed during and after therapy.
A willingness to interact with the child has great importance for building a bonding between the parents and the child. This can be very different from child to child. The more immature the premature infant, the lower his attention span or his ability to process stimuli [30]. Even in the early phase of the parent-child relationship, which is often highly stressed after a premature birth, music therapy can be an effective mean of communication to initiate the first dialogues and facilitate mutual relaxation, joy, and playful exchange [31]. Feedback from parents in our study shows that music therapy helps about half of parents to meet their child, which helps to promote parent-child bonding [32]. Involving the parents in the therapy encourages them to make music for their child. Studies have shown that family-centered music therapy has positive effects on parents and helps them to deal better with their worries and fears [8]. Parental stability, self-confidence and well-being are strengthened [32]. About half of the parents whose children received music therapy care at the University Hospital Essen during the study period stated that they had gained more self-confidence through music therapy.
Some parents also increasingly dare to sing for their child. In music therapy, parents can do something for the premature infant by leaving their voice as something irreplaceable and personal [12]. Only 22% of the parents felt encouraged to sing for their child outside of the therapy session. It is possible that the proportion of singing parents is significantly higher after discharge, as privacy is very limited in the inpatient environment, which increases inhibitions to sing. In the protected environment at home, the parents dare to sing for their child significantly more, which is also reflected in the answers to our questionnaire: All parents stated that they can imagine singing for their child even after they have been discharged. Three quarters of the parents can also imagine learning to play the sansula. A major limitation of our study is that the parent survey was limited to the perceptions of the music therapy interventions, the reactions of the children and the sociodemo- graphic characteristics of the parents in the therapy group. There was no questioning of the control group.
Conclusion
The family-centered music therapy is perceived by parents as a positive, supportive offer for themselves and for their children. The therapy promotes relaxation in parents and children as well as the parent-child interaction, which is necessary for the development of a stable bonding. Music therapy helps to relieve the families of prematurely born children in the difficult early days.
Funding
The study received funding from the Stiftung Universitaetsmedizin Essen.
Conflicts of Interest
The authors have no conflict of interests to declare.
References
- Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, et al. (2019) Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health 7(1): 37-46.
- Muhe LM, McClure EM, Nigussie AK, Mekasha A, Worku B, et al. (2019) Major causes of death in preterm infants in selected hospitals in Ethiopia (SIP): a prospective, cross-sectional, observational study. Observational study 7(8): 1130-1138.
- Huening B, Jaekel, J (2021) Prematurity and long-term consequences into school age. Implications for aftercare and school. Childhood and development 30 (1): 37-50.
- Doyle LW, Victorian Infant Collaborative Study Group (2004) Evaluation of neonatal intensive care for extremely low birth weight infants in Victoria over two decades: I. effectiveness. Pediatrics 113(3 Pt 1): 505-509.
- Serenius F, Kallen K, Blennow M, Ewald U, Fellman V, et al. (2013) Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA 309(17): 1810-1820.
- Wu F, Liu G, Feng Z, Tan X, Yang C, et al. (2019) Short-term outcomes of extremely preterm infants at discharge: a multicenter study from Guangdong province during 2008-2017. BMC Pediatr 19(1): 405.
- Brossard R, Murnick J, Bouyssi M, Coulombe J, Chang T, et al. (2017) Altered Cerebellar Biochemical Profiles in Infants Born Prematurely. Sci Rep 7(1): 8143.
- Haslbeck FB, Jakab A, Held U, Bassler D, Buchera H, et al. (2020) Creative music therapy to promote brain function and brain structure in preterm infants: A randomized controlled pilot study. Neuroimage Clinical 25: 102171.
- Parikh NA (2016) Advanced neuroimaging and its role in predicting neurodevelopmental outcomes in very preterm infants. Semin. Perinatol 40(8): 530-541.
- Moon CM, Fifer WP (2000) Evidence of Transnatal Auditory Learning. J Perinatol 20(8 Pt 2): 37-44.
- Haslbeck F (2013) Advanced training in music as therapy in the premature baby ward. Introduction and orientation. Munich.
- Nöcker R (2007) Lecture at the anniversary conference of the Music Therapy course of the Westphalian Wilhelms University of Münster on 23-25.
- Fischer, Als (2003) What do you want to tell me? Individual relationship-based care in the neonatal intensive care unit to promote the development of the premature child. In: Nöcker-Ribaupierre, M. Hören-Bridge into Life. Music therapy with premature and newborn children. Göttingen Vandenhoeck Ruprecht Verlag 17-43.
- Sarimski K, Porz F (2004) Premature babies after discharge. Information brochure of the Federal Association "The Premature Child" e.V. Frankfurt am Main.
- Dudek L (2004) Parent stress in the neonatal intensive care unit and the influence of parent and infant characteristics. Am J Occu Ther 58(5): 509-520.
- Howe TH, Sheu CF, Wang TN, Hsu YW (2014) Parenting stress in families with very low birth weight preterm infants in early infancy. Res Dev Disabil 35(7): 1748-1756.
- Baley J, COMMITTEE ON FETUS AND NEWBORN (2015) Skin-to-Skin Care for Term and Preterm Infants in the Neonatal ICU. Pediatrics September 136(3): 596-599.
- Huening BM, Reimann M, Sahlmen S, Leibold S, Nabring, et al. (2016) Concept analysis of inpatient and outpatient psychosocial family-centered care in neonatology in the time of the G-BA resolution. Clin Padiatr 228: 195-201.
- Kobus S (2018) Musical accompaniment for premature babies and their families. Row point of time music. Wiesbaden Dr. Ludwig Reichert Publishing House.
- Bieleninik L, Ghetti C, Gold C (2016) Music Therapy for Preterm Infants and Their Parents: A Meta-analysis. Pediatrics 138(3): e20160971.
- Haslbeck F (2012) Music therapy for premature infants and their parents: an integrative review. Nordic J Music Therapy 21: 203-226.
- Standley J (2012) Music therapy research in the NICU: an updated meta-analysis. Neonatal Network 31(5): 311-316.
- Hartling L, Shaik M, Tjosvold L, Leicht R, Liang Y, et al. (2009) Music for medical indications in the neonatal period: a systematic review of randomised controlled trials. Arch Dis Child Fetal Neonatal Ed 94(5): 349-354.
- Loewy J, Stewart K, Dassler A, Telsey A, Homel P (2013) The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics 131(5): 902-918.
- Kobus S, Diezel M, Dewan MV, Huening B, Dathe AK, et al. (2021) Music Therapy Is Effective during Sleep in Preterm Infants. Int J Environ Res Pub Heal 18(16): 8245.
- Lüdin C (2014) Passion for fatherhood. About the importance of attachment-promoting elements of Emotional First Aid (EEH) for fathers, as the basis of the parent-child bond. Final thesis of the training to become a specialist advisor for emotional first aid (EEH). Basel.
- Treyvaud K, Lee KJ, Doyle LW, Anderson PJ (2014) Very preterm birth influences parental mental health and family outcomes seven years after birth. J Pediatr 164(3): 515-521.
- Yaari M, Treyvaud K, Lee KJ, Doyle LW, Anderson (2019) Preterm Birth and Maternal Mental Health: Longitudinal Trajectories and Predictors. J Pediatr Psychol 44(6): 736-747.
- Janus L (2011) How the soul arises-our psychic life before, during and after birth. Heidelberg Mattes Verlag.
- Rose SA, Feldman, JF, Jankowski, J, Van Rossem R (2005) Pathways from prematurity and infant abilities to later cognition. Child Development 76(6): 1172-1184.
- Papoušek M (2012) Preface. In: Nöcker-Ribaupierre, M. Hören-Brücke into life. Music therapy with premature and newborn children. Göttingen: Vandenhoek Ruprecht Verlag 7-11.
- Nöcker RM (2015) International music therapy approaches for premature children. In: Musiktherapeutische Umschau. Research and practice of music therapy. Göttingen Vandenhoeck Ruprecht GmbH Co KG 36: 2.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.