Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Measurement of Radiation Doses in Computed Tomography (CT) and Estimated Radiological Risk of Cancer
*Corresponding author: Rahman S, Department of Physics, University of Chittagong, Chittagong-4331, Bangladesh.
Received: September 13, 2021; Published: October 20, 2021
DOI: 10.34297/AJBSR.2021.14.002004
Abstract
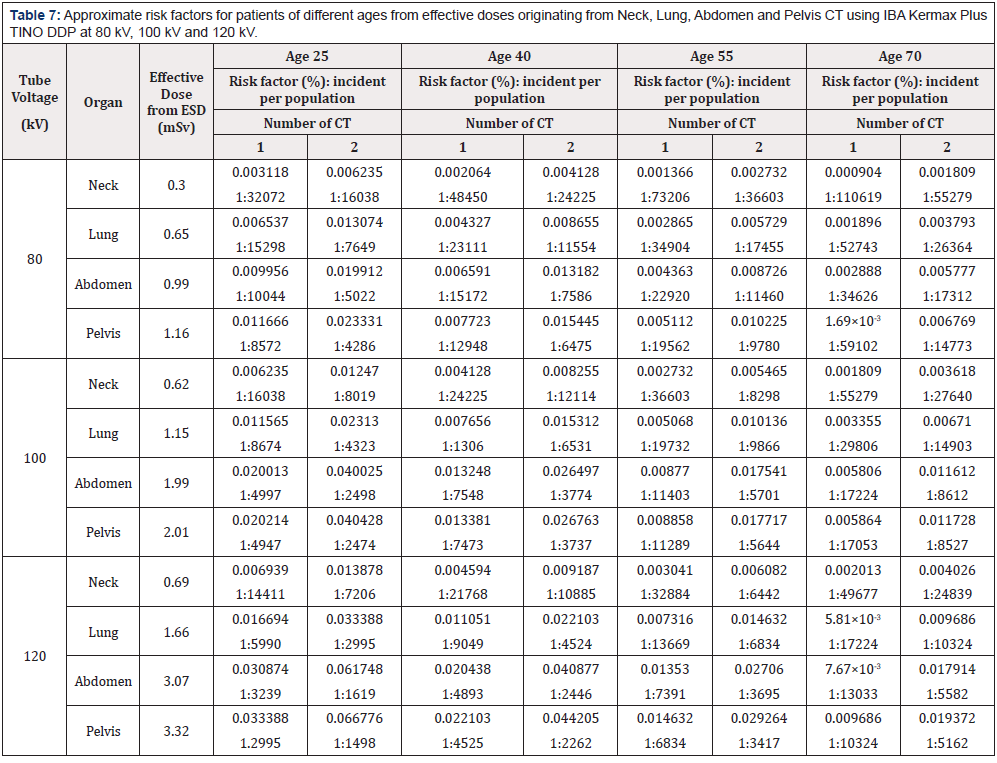
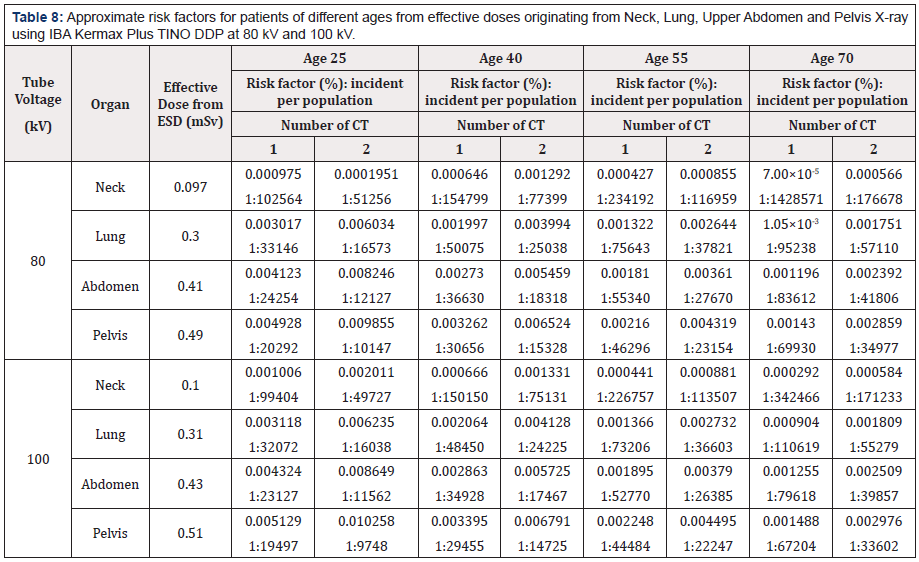
The abundant observance of CT in medical diagnosis delivers higher radiation doses to patients than other radiological imaging systems which is a great concern for the increased radio sensitivity of certain tissue and radiation related cancer. In the present measurement, we have investigated patient effective doses by CT examination to Neck, Lung, Abdomen and Pelvis and a comparison is also made for the contribution of doses with digital radiography (X-ray) using Alderson Rando Phantom at the tube potential 80 kV-120 kV. Effective Dose (ED) measured using Entrance Surface Dose (ESD) for Neck were ranged from 0.30 mSv to 0.69 mSv, for Lung 0.65 mSv to 1.66 mSv, for Abdomen 0.99 mSv to 3.07 mSv and for Pelvis 1.16 mSv to 3.32 mSv, and the corresponding EDDLP measured using dose-length product were ranged from 0.45 mSv to 1.52 mSv for Neck, 1.99mSv to 6.76 mSv for Lung, 2.14 mSv to 7.51 mSv for Abdomen, 1.70 mSv to 5.95 mSv for Pelvis which lie within the reference level established by some other international institutions. From the present study it is found that CT doses is remarkably higher than digital X-rays i.e. for example; CT dose is 6.2 times higher than that of digital radiography at the same tube voltage 120 kV X-rays for neck imaging. The estimated risk factor and incident per population for both X- ray and CT are presented. It is observed that risk factor decreases with the increase of age and risks were increased with the increasing number of exposure.
Keywords: Computed tomography, Ionizing radiation, Effective dose, Radiation risk.
Abbreviations: CT: Computed Tomography; ED: Effective Dose; DLP: Dose length product; ESD: Entrance Surface Dose; NMPI: Nuclear Medical Physics Institute; IPEM: Institute of Physics and Engineering in Medicine
Introduction
The use of computed tomography (CT) techniques in diagnostic radiology imaging procedures has increased rapidly worldwide over the past three decades because of its splendid technological progress and remarkable performance. Now CT is a standard modality in assessing a variety of disorders in patients as well as for cancer detection, surveillance, and evaluation of trauma and CT will continue to provide remarkable advantage to modern medical treatment and the advantage derived by the patient will go far beyond the small risk associated with any properly conducted imaging modality [1]. The X-ray beam based CT typically deliver doses that are substantially greater than those received from conventional radiographic technique and the growing use of CT procedures is a topic of widespread concern. Issues of concern is the increased radio-sensitivity of certain tissues and a longer lifetime for radiation-related cancer [2]. Due to the disproportionately high amount of radiation used, CT accounts for more probable induced cancers than any other medical imaging modality [3]. Most imaging procedures have a relatively low risk but the risk associated with medical imaging procedures refers to possible long-term or short term side effects [4]. Possibility of harm could estimate by quantifying the radiation received by patients who is undergoing radiological examinations. In radiography, the sensitivity of the organs and tissues which being irradiated during the radiographic projections depend on the Entrance Surface Dose (ESD) to patient [5]. As the risk of cancer accumulates with the patient’s lifetime accumulation of radiation exposure the effective dose calculation helps to quantify stochastic risk of carcinogenesis. During diagnosis, in order to lessen extraneous radiation to patients, it is necessary to determine what amount of radiation exposure has occurred [6]. Now a day, Cancer is treated as one of the most dangerous health issues and is a leading cause of death worldwide accounting for an estimated 9.6 million deaths in 2018. Approximately 70% of deaths from cancer occur in low- and middle-income countries [7]. Radiation exposure from medical imaging may be responsible for 1-3% of cancers worldwide [8]. Account for this issue, researchers all over the world observed the radiation dose of patient for computed tomography (CT) scan of different organs of human body using different types of dosimeters and different methods. In this study, Alderson Rando human phantom is used in lieu of actual patients and real time dosimeters are used for dose measurement and cancer risk are calculated by using web based risk calculator. The main examinations focused on this study are the calculation of effective dose from ESD and stochastic risk of cancer. The aim of the present study is to monitor the effective dose of the patients during diagnosis within the recommended value of International Atomic Energy Agency (IAEA) to keep the patient dose as low as possible, and the estimation of the fatal cancer risk and to compare with published literature on patient dosimetry.
Materials and Methods
This study includes commonly performed medical diagnostic Neck, Lung, Abdomen and Pelvis CT scans examination and digital X-ray examinations. For CT scan examination, Philips Ingenuity TT PET/CT of 128 slices is used which is located at NMPI, AERE. In lieu of actual patients Alderson Rando human phantom, which comprises ingredients similar to human tissue used to investigate the effect of radiation beams on human beings, has been used. The X-ray examination was performed at Ahsania Mission Cancer and General Hospital, Dhaka. Radiographic factors included tube potential (kVp), exposure setting (mAs), and focus to skin distance (FSD) that were used normally in each radiology room by radiographers for average size adult patients (with weights between 60-80 kg according to the European guideline) for only suitable diagnostic quality images as distinct by the radiologist. Dosimetry protocols proposed by IAEA international code of practice TRS 457 and by the report no. 77, Institute of Physics and Engineering in Medicine (IPEM) were used to measure the quality control parameters [4,9]. Electronic personal dosimeters (EPD) of Polimaster (PM1610) series and IBA Kermax-Plus Tino DDP (M: 120-131 Tino) provide measurement of dose equivalent [10,11]. Calibration factors for all the dosimeters are used in this experiment and these were multiplied with the dosimeter values to get the corrected dose. IBA Kermax-Plus Tino DDP dosimeter was placed on the selected target organ to do CT scan and at the same time pocket dosimeters were placed on the other concerned organs to measure the scattered dose. CT was performed for Neck, Lung, Abdomen and Pelvis. While one of them was selected as target organ other three were considered as organs at risk. The whole process was repeated for three different tube voltages 80 kV, 100 kV and 120 kV. Quality control tests such as Computed Tomography Dose Index (CTDI) (volume), mAs (mili ampere second), DLP (Dose Length Product) were also observed from the CT machine for different CT examinations. Entrance dose has been observed through direct measurement. Doses were observed for target organ as well as associated scatter dose for other organs.
The tissue weighting factor is a relative measure of the risk of stochastic effects that might result from irradiation of that specific tissue. It accounts for the variable radio sensitivities of organs and tissues in the body to ionizing radiation. The radiation weighting factor is the value selected for a specified type and energy of the radiation. The probability of stochastic radiation effects depends not only on the absorbed dose, but also on the type and energy of the radiation causing the dose. Determination of Effective Dose (ED) has been defined by the ICRP as the sum of the weighted equivalent doses to specified organs and provides a useful measure of radiation risk (ICRP, 2007) [12].
𝐸 = ΣTWTHT = ΣT𝑊T ΣT𝑊𝑅𝐷T,R ………………. (1)
where, 𝑊𝑇 is the tissue weighting factor, and 𝐻𝑇 is the equivalent dose in that tissue or organ. 𝐷𝑇,R is the mean absorbed dose in tissue T, due to radiation R. WR is the radiation weighting factor [12].
In this study, Conversion Coefficients were used that are derived in National Radiological Protection Board (NRPB), UK to relate measured entrance surface dose (ESD) and ED [13]. The formula given below:
ED (mSυ) = Entrance Surface Dose (mGy) × CC ESD (mSυ/mGy) ………………. (2)
where, the symbol has their usual meaning. CCEntrance dose was used from the table presented in report of NRPB [13]. To determine the Effective dose (EDDLP) from Dose Length Product, DLP and CTDIvol for each CT examination were noted from CT machine. Then EDDLP was calculated from the product of DLP and the body region-appropriate DLP to ED conversion coefficient, k. This are the following method to estimate EDDLP
EDDLP = k × DLP ………………. (3)
Where, k is coefficient factor for the anatomic region scanned [14].
Measurement of the Entrance dose for X-ray contained diagnostic x-ray examinations namely; Neck X-ray, Lung X-ray, Abdomen X-ray and Pelvis X-ray. In this study, Alderson Rando human phantom (male) is also used in all cases instead of real patients. Same dosimeters and same procedures were followed in X-ray examination like CT examination. In all cases tube voltages are taken as 80 kV and 100 kV.
To find the estimated radiological risk of cancer a website X-RayRisk.com was used. This is an educational website that focuses on estimating this risk (https://www.xrayrisk.com/about.php) [15]. One of the site’s main features is a web based calculator that allows users to track their imaging history and estimate their personal risk, while providing answers to frequently asked questions. There are no published studies that prove the direct causality between medical imaging and increased cancer risk. Most of the evidence on radiation-induced cancer risk comes from 4 groups: Japanese atomic bomb survivors, medically exposed populations, occupationally exposed groups, environmentally exposed groups. Present data on radiation exposure and cancer risk are coming from the above mentioned sources. The assumed increased risk of cancer from low dose medical exposure (CT scans and X-rays) is based on individuals exposed to high doses (atomic bombs and nuclear accidents). The linear no threshold model is the theory that the increased risk holds true at these lower doses and is the currently adopted model for calculating radiation risk.
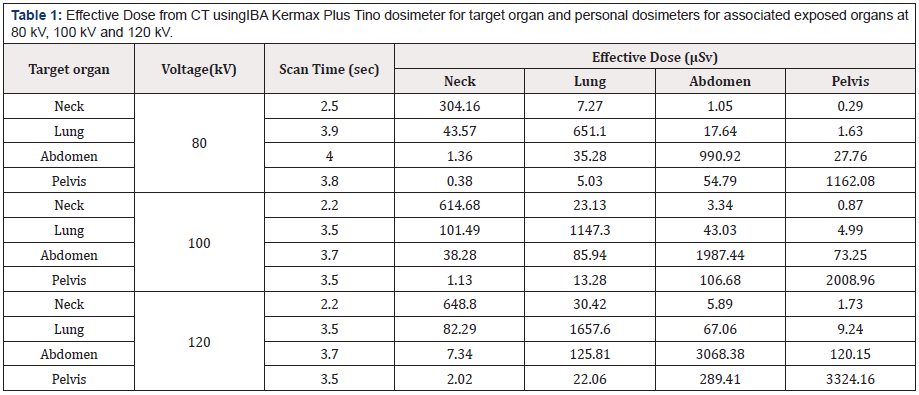
Table 1: Effective Dose from CT usingIBA Kermax Plus Tino dosimeter for target organ and personal dosimeters for associated exposed organs at 80 kV, 100 kV and 120 kV.
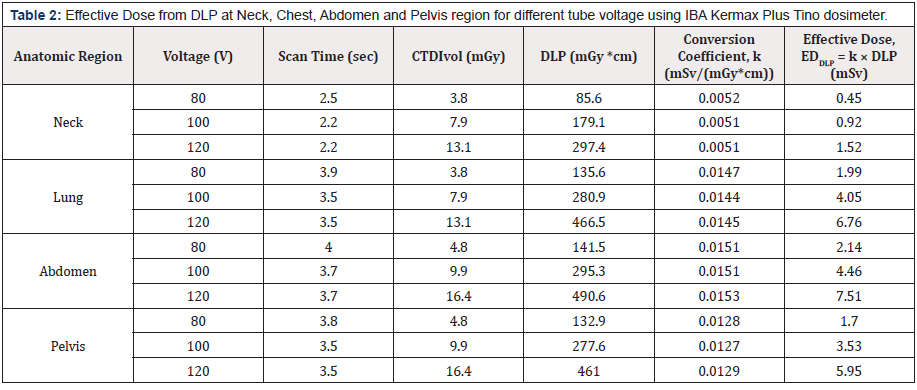
Table 2: Effective Dose from DLP at Neck, Chest, Abdomen and Pelvis region for different tube voltage using IBA Kermax Plus Tino dosimeter.
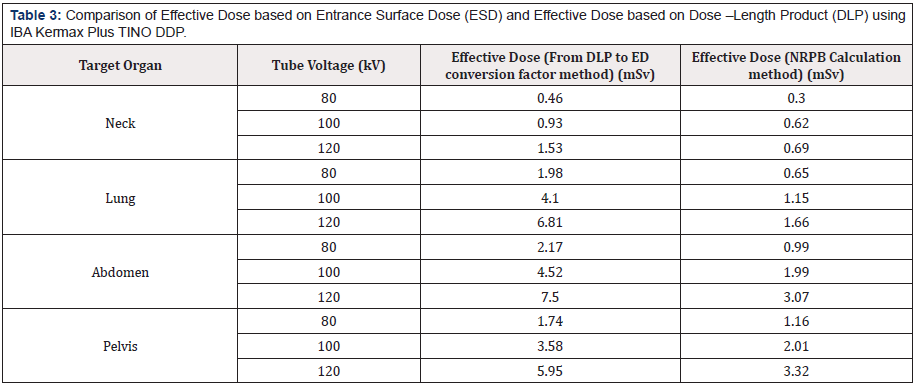
Table 3: Comparison of Effective Dose based on Entrance Surface Dose (ESD) and Effective Dose based on Dose –Length Product (DLP) using IBA Kermax Plus TINO DDP.
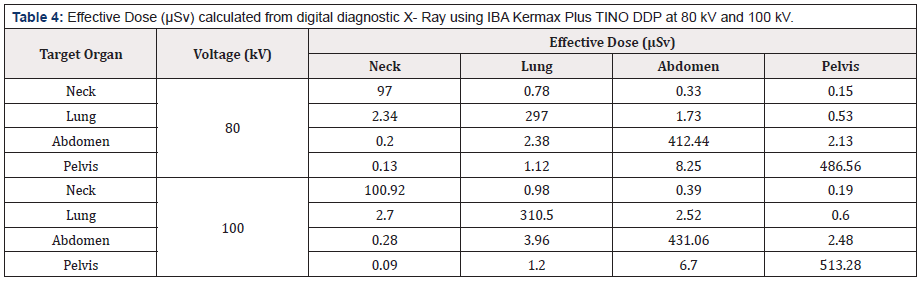
Table 4: Effective Dose (μSv) calculated from digital diagnostic X- Ray using IBA Kermax Plus TINO DDP at 80 kV and 100 kV.
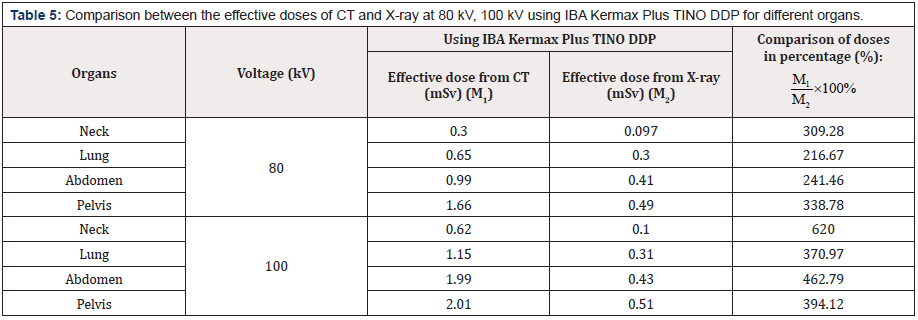
Table 5: Comparison between the effective doses of CT and X-ray at 80 kV, 100 kV using IBA Kermax Plus TINO DDP for different organs.
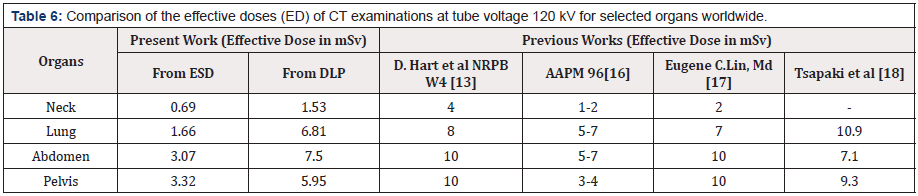
Table 6: Comparison of the effective doses (ED) of CT examinations at tube voltage 120 kV for selected organs worldwide.
Harmful Light Metals
Recently, however, bioresonance therapists have noticed that titanium is less and less tolerated after several months. This runs parallel to the exposure to chemtrails, which contain titanium as an important component, and to the titanium oxide admixtures in many medicines. Whereas heavy metals used to be the main problem, light metals have now been added, most clearly visible in the aluminium poisoning of the brain and especially our pineal glands. Elements that are far apart in the periodic table of the elements produce a battery together with the electrolyte of the saliva. Dentogenic-galvanic current production takes place, the intensity of which can be far higher than the endogenous currents of the central nervous system. This concerns especially the combination of mercury amalgam or gold on the one hand and titanium on the other hand [2].
RANTES and NICO
Now to the RANTES = CCL5 (CC-chemokine ligand 5). It is a
cytokine out of the family of the CC-chemokines
1. It is thanks to colleagues Lechner and von Baehr
2. That they have uncovered the relationship between chronic
NICO-type jaw osteitis (non-infectious chronic osteitis) and
serious diseases in the body. This concerns mainly cancer, in
women preferentially breast cancer.
With regard to NICO, there are several problems:
a) It hardly causes any pain or other subjective discomfort
b) It is not known/recognised by most dentists
c) It is difficult to detect in normal X-rays
Problems with the Focus Examination
For decades, the author sent patients who showed dental focus findings in bioresonance to the dentist with the request for a focus clarification. Most of them came back with the result “everything is fine, there is nothing there”. Then, when computer tomography came along with the possibility of being able to assess the jaw bones more precisely, patients surprisingly came back after the Newtom- CT [3] with the result of a tooth root or jawbone focus. The time of objectifying suspicious findings began. Unfortunately, this has still not caught on. In the last years a further instrument was developed, it is the CaviTAU [4] ultrasound examination. It goes beyond the wellknown osteonecrosis of the jaw (ONJ, [5].
Now one could object that this is, so to speak, dental esotericism. However, this objection is no longer valid since the objective blood value of the RANTES became analysable in such cases. RANTES is a chemokine that can be detected in elevated levels in chronic noninfectious inflammations like NICO and represents, among other things, the oxidative stress.
Quote from a publication (by Lechner and von Baehr) [6]
“For decades, phenomena such as “jaw osteitis” and “NICO” have been causally associated with general diseases as so-called “foci”. Energy pathways of Chinese acupuncture have also served as holistic functional and explanatory models. The authors’ research shows with modern laboratory methods that over-activated signal transduction cascades, especially of the chemokine RANTES in osteolytic changes of the jaw bone, can be linked to RANTES effects in complex chronic diseases. We thus present an extended explanatory model of the so-called “interference field effect” from the tooth-jaw area and thus promote complementary and integrative thinking in medicine and dentistry.”
A Typical Case
A woman with breast cancer came for a TimeWaver® [7] examination every 2 months. She rejected orthodox medicine. Each time, among other things, a NICO suspicion came out, concerning the area 37/38. She went to the family dentist, who found nothing in the normal panoramic X-ray. Then she chose a complementary dentist who was able to confirm the findings on CT. He sent blood for RANTES determination to a special laboratory, with the result of an increase. Additionally, she still had three amalgam fillings. She wrote in her email from July 07th, 2021: “I will visit the dentist Dr. J.L. in Munich, who can do a CaviTAU ultrasound examination to determine possible diseases of the jaw. The RANTES value is 58.2 and should be less than 30. Meanwhile I know that RANTES is responsible for many diseases, including breast cancer. During the bioresonance therapy you had always seen that I had a noninfectious inflammation in my jaw. Now it is for sure. This case is exemplary for the topics of NICO and RANTES. May this knowledge spread as soon and generally as possible? The so frequent separation of dentistry and holistic medicine must not be maintained.
Summary
The largely unknown but pathogenetically important subject of foci in the area of the tooth roots and jaw bones is listed. The terms NICO (non-infectious chronic osteitis) and RANTES (an important chemokine) are explained. Their importance is largely underestimated. An integral, cause-related medical science must take this into account, as a toxin-free mouth is of great importance and should be achieved in all of us.
References
- Thierry Chef I, Dabin J, Friberg EG, Hermen J, Istad TS, et al (2013) Assessing Organ Doses from Pediatric CT scans-A Novel Approach for an Epidemiology Study (the EPI-CT Study). Int J Environ Res Public Health 10(2): 717-728.
- Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet 380(9840): 499-505.
- (2019) Radiological Society of North America, Inc. (RASNA) Radiation Dose in X-Ray and CT Exams, Reviewed 1-5.
- (2007) International Atomic Energy Agency (IAEA); Dosimetry in Diagnostic Radiology: An International Code of Practice, Technical Reports Series 457.
- Fujibuchi T, Kato H, Hashimoto M, Abe Y, Kikawa T (2006) Characteristic evaluation of a real-time silicon dosimeter and measurement of entrance surface dose at radiography. Nihon Hoshasen Gijutsu Gakkai Zasshi 62(7): 997-1004.
- Sorop I, Dadulescu E (2011) Assessment of entrance surface doses for newborn babies with an intensive care unit. Roma Rep Phys 63(2): 401-410.
- World Health Organization (WHO) Cancer (March 2021).
- González ABD, Darby S (2004) Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries, The Lancet 363(9406): 345-351.
- Ranallo FN (1998) Recommended standards for the routine performance testing of diagnostic x-ray imaging systems, IPEM Report No 25(8): 1556-1557.
- User manual Step Sensortechnik und Elektronik Pockau GmbH, X-ray and gamma ray dosimeter: Polimaster.
- (2021) User manual Kermax plus Tino, IBA Dosimetry GmbH.
- (2007) International Commission on Radiological Protection (ICRP), The 2007 Recommendations of the International Commission on Radiological Protection; ICRP publication no 103, Ann ICRP 37 (2-4): 1-332.
- Hart D and Wall BF (2002) Radiation Exposure of the UK population from Medical and Dental X-ray Examinations, National Radiological Board (NRPB-W-4) Report :1-41.
- Deak PD, Smal Y, Kalender WA (2010) Multi-section CT Protocols: Sex and age-specific conversion factors used to determine effective dose from Dose Length Product. Radiology 257(1): 158-166.
- American Society of Radiologic Technologist (ASRT); X-ray Risk, Radiation and Medical Imaging.
- (2008) American Association of Physicists in Medicine (AAPM); The measurement, reporting, and management of radiation dose in CT, Report of AAPM Task Group 23 of the diagnostic imaging council CT committee, Report No 96.
- Eugune C and Lin MD (2010) Radiation Risk from Medical Imaging, Mayo Clin Proc 85(12): 1142-1146.
- Tsapaki V, Kottou S and Papadimitriou P (2001) Application of European Commission reference dose levels in CT examinations in Crete, Greece, Brits Jour of Radio 74: 836-840.
- Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, et al (2003) Cancer risks attributable to low doses of ionizing radiation: assessing what we really know, Proc Natl Acad Sci USA 100(24): 13761-13766.
- Dauer LT, Brooks AL, Hoel DG, Morgan WF, Stram D et al Review and evaluation of updated research on the health effects associated with low dose ionizing radiation, Radi Prot Dosi 140(2): 103-136.
- (2005) The International Commission on Radiological Protection (ICRP); Low-dose extrapolation of radiation-related cancer risk, Annals of ICRP, ICRP Publication 99, Elsevier, 35(4).
- Colang JE, Killion JB, Vano E (2007) Patient dose from CT: A literature review, Radiologic Technology 79(1): 17-26.
- Vafaei A, Khosravi N, Barjouei NS, Gholizadeh N, Sadeghi AO, et al. (2019) Radiation organ dose measurement and cancer risk estimation in CT examination on trauma patients, Mid East Jour Canc 10(3): 206-213.
- Hussain SA, Sullivan R (2013) Cancer control in Bangladesh. Japan J Clin Oncol 43(12):1159-1169.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.