Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Multidisciplinary Development and Evaluation of Pre-anesthesia Assessment Guidelines for Pediatric Obese Patients
*Corresponding author: Grace Kim, Departments of Pediatrics and Endocrinology University of Washington, Seattle Children’s Hospital, Seattle, WA, USA
Received: November 23, 2021; Published: November 29, 2021
DOI: 10.34297/AJBSR.2021.14.002053
Abstract
Background: Obesity may increase the risk of anesthetic complications. Obesity and related comorbidities may not be recognized until presurgical evaluation.
Aim: We describe a multidisciplinary effort resulting in the evaluation of outcomes post implementation of guidelines for evaluation of obese children in the pre-anesthesia assessment (PASS) clinic and its impact on anesthetic complications.
Methods: Literature review and expert consensus were used to create evidence-based guidelines for pre-operative assessment of obese children in this quality improvement project. Representatives from anesthesia, cardiology, endocrinology, pulmonary and surgery were involved. Outcomes related to guideline implementation were compared pre-post 1year implementation and stratified by presence/absence of PASS evaluation. Subjects included ambulatory surgery patients 2-18 years of age, with a BMI> 95. Outcome measures include: 1) intra-operative desaturation, 2) difficulty during ventilation, and 3) escalation of care.
Results: 1,321 patients were included, 190 in PASS group and 1,131 in non-PASS group. PASS group had higher proportions of severe obesity and higher comorbidities. The frequency of intra-operative hypoxemia decreased from 14.1% to 7.7% among PASS patients and remained constant (6.6-7.7%) for the non-PASS group. There were no changes in difficulty with ventilation in either group. Escalation of care was very rare (0.9-2.0%).
Conclusion: Use of a multidisciplinary guideline for assessment of obese children in the pre-anesthesia clinic is feasible and may help to decrease anesthetic complications. In a pediatric hospital, guidelines did not affect escalation of care. In institutions with lower pediatric volume, its use may have a higher impact.
Six MeSH-compliant keywords
Pediatric obesity; Anesthesia; Obstructive sleep apnea; Practice guidelines; Patient safety; Obesity-hypoventilation. What is already known on the topic. Obese children and adolescents are at increased risk for perioperative complications, due to the compounding effect of comorbidities associated with obesity. What new information this study adds. Comprehensive-multidisciplinary and systematic preanesthesia evaluation for obese children and adolescents may help reduce post anesthetic complications.
Introduction
Childhood obesity is a public health concern, affecting 17% (12.7 million) of US children.[1] Pediatric obesity leads to respiratory and cardiovascular changes that affect anesthetic care and perioperative analgesia. Obese children also have higher need for surgical procedures and increased risk of anesthetic complications. [2,3] Anesthetic concerns when caring for these patients include difficult intubation [4,5] and ventilation due to reduced pulmonary compliance, increased chest wall resistance, and increased upper airway resistance.
Obesity is associated with obstructive sleep apnea (OSA), reactive airway disease, insulin resistance, type 2 diabetes, fatty liver disease, and hypertension, among other conditions. A systematic review identified medication safety and airway management as primary safety concerns in obese children receiving acute care. [6] Prior studies have focused on these areas of concern highlighting the importance of pre-anesthetic evaluation of respiratory risk factors, especially OSA, and medication administration in obese children. [7,8] Comprehensive guidelines to systematically evaluate this group of children for surgical procedures are often lacking.
We describe a multidisciplinary effort to create and implement pre-anesthesia guidelines for comprehensive assessment of obese children. We evaluated at the effect of the use of the guidelines on anesthetic complications and escalation of care in a population of obese pediatric ambulatory patients.
Methods
PASS Clinic was designed to see patients that have one or more medical conditions that could increase their risk for problems with anesthesia. The clinic is to assess whether a patient is healthy enough to receive anesthesia and to ensure a patient does not have any health problems that could delay their procedure. PASS clinic existed before implementation of the guidelines. It is upon clinical discretion of individual surgeons on whether a specific patient needs to attend PASS clinic pre-operatively. Non-PASS patients are evaluated on admission/the day of surgery.
Description of Guidelines
The setting for this quality improvement work was a tertiary care, freestanding children’s hospital. It involved a multidisciplinary working group of stakeholders from the departments of anesthesia, cardiology, endocrinology, pulmonary, and surgery. Literature review and expert consensus was used by this working group to create recommendations to guide pre-anesthesia assessment and perioperative planning for obese children scheduled for surgery and diagnostic procedures under anesthesia. Based on prior literature on safety events on this population, we focused our work on recommendations for recognition, severity assessment and perioperative management of obstructive sleep apnea, cardiovascular symptoms, hyperglycemia, and hypertension. We used an iterative approach and approved the final guidelines by consensus prior to implementation. Guidelines were created for children age 2yrs-18yrs with BMI ≥95th percentile and distributed to medical staff in PASS clinic. Development of guidelines took 18 months and implementation took place in the PASS clinic through educational session aimed at the clinic’s medical providers. Providers provided feedback leading to revisions. Final guidelines were adopted into practice via consensus from the multidisciplinary panel and PASS providers.
To evaluate the guidelines, we compared the rates of anesthetic complications and escalation of care between obese patients referred to the PASS clinic (referred to as PASS) and those not referred to PASS (non-PASS) clinic. Referral groups were further divided into 1year before (pre) and after implementation (post) of the guidelines. We only included patients scheduled for ambulatory procedures. With this design, we had four comparison groups: PASS-pre, PASS-post, non-PASS-pre, and non-PASS-post.
Primary outcome measures were 1) intra-operative desaturation (Saturation measured with Pulse-oximetry (SpO2) <90% longer than 5 minutes); 2) difficulty during ventilation, and 3) escalation of care (change in post-operative disposition: planned day surgery requiring hospitalization, emergency department visit within 72 hours after day surgery discharge, or re-admission within 36 hours of discharge from the index visit). We identified anesthetic complications using quality improvement data, generated by anesthesiologist self-report at the end of every anesthetic encounter and before discharge from the post-anesthesia recovery area. In addition, we reviewed data from all electronic anesthetic records to determine intra-operative hypoxemia defined by intra-operative desaturation (SpO2<90%) longer than 5 minutes, as well as report of difficult intubation or ventilation.
Using our electronic medical records, we identified all patients scheduled for ambulatory surgical procedures between June 2016- May 2018. We included patients 2-18 years of age who at the time of surgery had a BMI≥95%. We excluded patients who underwent emergent procedures or patients that were had planned hospitalizations.
Statistical Analysis
To assess whether any changes in complication rates were occurring among the larger surgical population independent of the pathway introduction, we compared complication rates within and between groups before and after implementation of the guidelines.
Clinical and demographic characteristics as well as frequency of complications are summarized descriptively by time (pre vs. post) for PASS and non-PASS patients separately and are compared using a t-test (age) and chi-square tests. An alpha of 0.05 was used for statistical significance testing. We used a linear regression model with interaction to conduct a difference in differences analysis comparing the difference in complication frequency among PASS vs. non-PASS patients before and after the guideline’s introduction. Data on complications rates were plotted monthly over time by PASS clinic status using statistical process control (SPC) charts and proportions with standard errors. Descriptive sub-analyses of complication rates were conducted among higher risks groups, assessing only patients with extreme obesity (≥99 percentile BMI) and assessing by ASA status (ASA 1 and 2 vs. ASA 3 and 4). Data on frequency of escalation of care and presence of hypoxemia during surgery were available reliably for these two populations and were used as the primary outcome measures. IRB approval was obtained for all aspects of this study.
Results
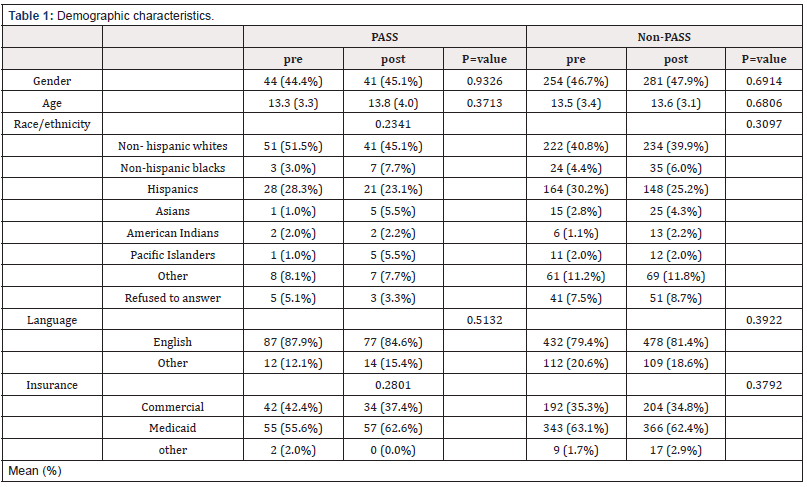
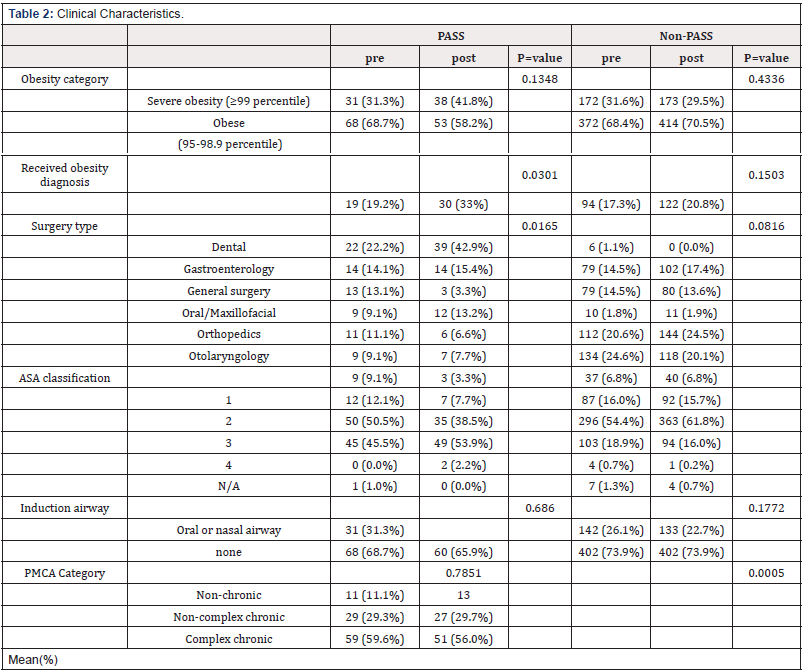
A total of 1,321 patients were included in the study: 190 PASS, 1131 non-PASS. Baseline demographic and clinical characteristics differed between groups (Table 1). Patients seen in PASS clinic were more likely to be non-Hispanic White (NHW), have severe obesity (BMI≥ 99%), and higher comorbidity measured by ASA and the Pediatric Medical Complexity Algorithm (PMCA) classification. PMCA is a classification system to code level of medical complexity in a child with chronic disease. (8b) Referrals to PASS clinic by surgical specialty also varied at baseline (Table 2).
Patient characteristics did not change significantly postguideline implementation, but more patients in the PASS group had received a diagnosis of obesity post-guidelines. In the PASS group, the proportion of patients that received obesity diagnosis increased. In the non-PASS group, the proportion of severely obese patients remain stable, however the referral patterns form some surgical services changed. Specifically, general surgery and orthopedic surgery patients were less likely to be referred to the PASS clinic.
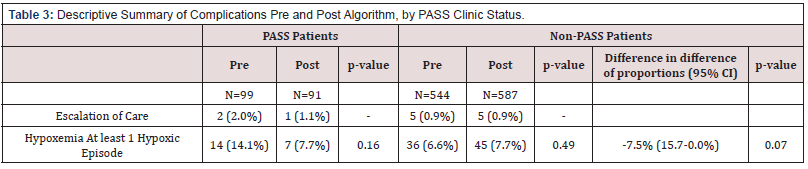
Escalation of care was very low in both the PASS and non- PASS populations (Table 3). Of the 1327 patients selected for this study, only 13 (0.9%) required escalation of care. In the PASS group 2 (2.0%), and 1 (1.1%) patient required escalation of care pre and post implementation of the guidelines, and in the non- PASS group 5 (0.9%) and 5 (0.9%) patients respectively. Of these 13 patients, escalation included: post-operative evaluations for bleeding, respiratory distress, non-bleeding surgical complications, insufficient analgesia, and anxiety. Four required hospitalizations for analgesia. Two returned to the emergency department for mild post-operatively bleeding after discharge (requiring dressing change and discharged immediately after). Two patients had respiratory symptoms after procedure (esophagogastroduodenoscopy (EGD) and tonsillectomy and adenoidectomy). The EGD patient was at a local ambulatory center and had to be transferred to emergency department. The tonsillectomy and adenoidectomy patient were seen preoperatively at the PASS clinic with a recommendation for direct admission, but the recommendation was not followed through. Two patients had non-bleeding surgical complications and two patients had anxiety episodes. Four patients required hospitalization due to inadequate analgesia after surgery. Of the 12 patients, four of them (18%) were scheduled in our ambulatory center; requiring transportation to the main hospital to manage their post-operative course.
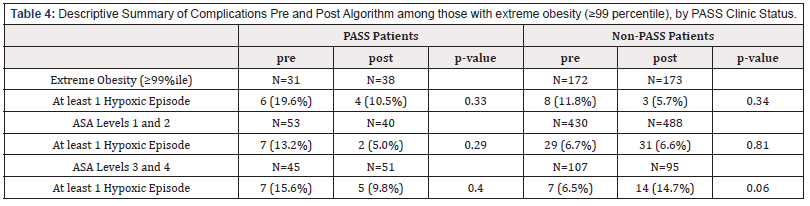
Frequency of intra-operative hypoxemia decreased from 14.1% to 7.7% among PASS- patients after implementation of guidelines while it remained constant for the non-PASS group (6.6 vs 7.7%) (Table 3). The difference between PASS and non-PASS groups was 7.5%’ however, it did not reach statistical significance. When evaluating monthly changes in hypoxemic events, before and after implementation of the guidelines, there were no differences among the non-PASS cohort. Among the PASS cohort, there were zero episodes of desaturation in 8 of the 12 months after implementation of the guidelines. This trend however did not reach statistical significance due to the small sample size. The subanalyses of complication rates among higher risks groups [patients with extreme obesity (≥99 percentile BMI) and assessing by ASA status (ASA 1 and 2 vs. ASA 3 and 4)] showed not statistically significant after implementation of guidelines in both PASS and Non-Pass patients (Table 4).
Discussion
This multidisciplinary effort, using evidence-based guidelines, shows that a systematic approach for pre-anesthesia evaluation of obese pediatric patients can be implemented despite the complexity and heterogeneity of this population. In the evaluation of the effect of the guidelines on respiratory complications and escalation of care, we were underpowered to detect statistically significant changes, particularly as overall complication rates were quite low. However, there was a trend of decreasing frequency of intra-operative hypoxemia.
Currently, there are no formal pediatric obesity guidelines for preoperative evaluation, resulting in variable approaches that rely on individual anesthesiologists’ criteria. Several studies have assessed the need for hospital preparation when caring for obese pediatric patients. [6] Our study addresses this need, our approach around the pre-anesthesia visit, focus on optimization of pre-anesthesia assessment and planning of anesthesia and post-anesthesia care. Prior pediatric studies have highlighted the increased anesthetic risk for obese children, especially related to respiratory events. [9] Our study adds in the creation of a tool to systematically assess this population, emphasizing identification of other risk factors to reduce peri-operative complications. Another strength is the multidisciplinary effort and iterative process used during the creation of the guidelines. This process emphasized a thorough examination of the patient, without increasing resource utilization and avoiding as possible delaying or canceling procedures without compromising safety. Risk assessment prior to referral to consulting services, using lab tests and systematic physical evaluation of patients, aims for optimization of endocrine, cardiology and respiratory obesity comorbidities prior to surgery while balancing timing of surgery.
Additionally, low-income children and adolescents are more likely to be obese than their higher income peers.11 Thresholds for re-scheduling a procedure because an obesity related co-morbidity was undiagnosed or not managed optimally, were carefully consider avoiding unnecessary burden for families who plan for surgeries.
Another benefit of the pre-operative obesity assessment is the referral to a weight management clinic or letter to primary care physician suggesting follow up for obesity management. This aims to initiate a continued conversation about weight management.
Our study has some limitations. We utilized a convenient sample size that was not powered to detect differences between groups. However, this is a quality improvement project, and the focus was on rapid evaluation post-implementation. Additionally, referral to pre-anesthesia clinic was prompted by the surgery team, and is tightly linked with the type of surgery, therefore potentially introducing selection bias. Nonetheless, patients who received a referral to PASS clinic had more comorbid conditions, and therefore detected differences may be potentially larger. Another limitation is lack of medication administration data, especially considering that 2 patients who had escalation of care required hospitalization for pain management. Inadequate dosing has been previously documented in overweight and obese children [9].
Conclusions
The multidisciplinary creation and implementation of guidelines to systematically evaluate pediatric obese patients is feasible. Guidelines may facilitate anticipation of complications in this population, particularly in centers not staffed by dedicated pediatric anesthesiologists.
Acknowledgments
Dr. Kim and co-authors thanks surgical patients of Seattle Children’s Hospital.
Disclosures
1. There was no need for ethical approval.
2. The source of funding for the study came from Fulbright
Scholarship for Dr. Vera Sergeeva.
3. Any conflict of interest. My Coauthors and I have no conflicts
of interests.
References
- Prevalence of Childhood Obesity in the United States.
- Subramanyam R, Yeramaneni S, Hossain MM, Anneken AM, Varughese AM (2016) Perioperative Respiratory Adverse Events in Pediatric Ambulatory Anesthesia: Development and Validation of a Risk Prediction Tool. Anesth Analg 122(5): 1578-85.
- Mortensen A, Lenz K, Abildstrøm H, Lauritsen TL (2011) Anesthetizing the obese child. Paediatr Anaesth 21(6): 623-629.
- Porter RM, Thrasher J, Krebs N (2012) Implementing a Pediatric obesity care guidelines in a freestanding children’s hospital to improve child safety and hospital preparedness. J Pediatr Nursing 27(6): 707-714.
- Brodsky JB, Lemmens HJM, Brock Utne JG, Saidman LJ (2003) Anesthetic considerations for bariatric surgery: proper positioning is important for laryngoscopy 96: 1841-1842.
- Halvorson E, Irby M, Skelton J (2014) Pediatric Obesity and Safety in Inpatient Settings: A Systematic Literature review. Clinical pediatrics 53(10): 975-987.
- Coté, Charles J (2015) Anesthesiological Considerations for Children with Obstructive Sleep Apnea. Current Opinion in Anaesthesiology 28 (3): 327-32.
- Chidambaran V, Tewari A, Mahmoud M (2018) Anesthetic and Pharmacologic Considerations in Perioperative Care of Obese Children. Journal of Clinical Anesthesia 45: 39-50.
- Tamara D Simon, Wren Haaland, Katherine Hawley, Karen Lambka, Rita M Smith (2018) Development and Validation of the Pediatric Medical Complexity Algorithm (PMCA) Version 3.0. Academic pediatrics 18(5): 577-580.
- Tait A, Voepel LT, Burke C, Kostrzewa A, Lewis I (2008) Incidence and risk factors for perioperative adverse respiratory evenst in children who are obese. Anesthesiology 108(3): 375-380.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.