Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Ophthalmological Manifestations of SARS-COV-2
*Corresponding author: Nicolás Mauricio Molano Mosquera, General Physician, Universidad Santiago De Cali, Colombia.
Received: November 02, 2021; Published: November 18, 2021
DOI: 10.34297/AJBSR.2021.14.002040
Abstract
The World Health Organization declared on March 11, 2020 a pandemic due to COVID-19, a disease caused by SAR-COV-2. As there are no effective drugs available for this viral infection, many have been the efforts of health policies to achieve adequate control of the source of infection, transmission and protection in susceptible populations, through timely prevention measures.
Until now, the presence of viral conjunctivitis and the risk of contagion through the eye are data mentioned in the international literature in the course of various investigations. It was concluded that it can be transmitted through eye secretions. A search of various published articles was carried out, with the aim of knowing the main ocular manifestations of COVID-19 described in the literature by various authors in the main databases.
Keywords: Ophthalmological manifestations, COVID-19, SARS-COV-2, Conjunctivitis
Introduction
The COVID-19 epidemic began in Wuhan, in Hubei province, China, and in a short time spread to other continents. Italy was the first European country affected by the pandemic, especially in the northern part, in Lombardy. Severe acute respiratory syndrome 2 (SARS-CoV-2) is the cause of the coronavirus disease 2019 or COVID-19, thus typified by the World Health Organization (WHO). The current coronavirus pandemic (COVID-19) is a global health emergency and many countries have currently been affected with thousands of deaths and with great economic repercussions worldwide [1,2].
The clinical picture of COVID-19 ranges from mild, self-limiting respiratory tract symptoms to severe progressive pneumonia, multiple organ failure, and death [3]. The route of transmission occurs through the air, inanimate objects, and the fecal oral route. The virus can pass into the mucosa of the person’s oral cavity, nose, and eyes. It is transmitted primarily through person-to-person contact through respiratory droplets that are produced by coughing and sneezing.
The average incubation period is estimated to be around 5 days, with a range of 2-14 days. The onset of symptoms is characterized by a dry cough, fever and headache, in advanced stages respiratory distress, for which the patient would need mechanical ventilation [4,5].
Lu Cheng acknowledges that transmission through the ocular surface should not be ignored [6]. Although a low percentage of ocular manifestations is registered in patients with COVID-19, it is known that the virus can be isolated in the tear and conjunctiva that its transmissibility through ocular secretions is possible, and that adequate protection of ophthalmology personnel is of vital importance in the care of these patients [5] with the aim of knowing the ophthalmological manifestations reported by different researchers, this review is carried out.
Methodology
A systematic bibliographic search was carried out in databases such as pubmed, sciencedirect, Wiley, Google Scholar, plos one using the following descriptors such as COVID-19, SARS-COV-2, red eye, ophthalmological manifestations, conjunctiva, ocular transmission, conjunctivitis, glaucoma, retina, vasculitis, uveitis, optic nerve. Review articles, such as originals, letters to the editor, clinical cases and clinical studies, were used regardless of their year of publication.
Results
Ophthamological Manifestations
The conjunctiva is a transparent mucous membrane, responsible for maintaining ocular integrity and is the first structure to manifest alterations in the face of any extrinsic aggression. The bulbar conjunctiva presents a non-keratinized stratified squamous epithelium adhered to a thin basement membrane, which is in direct contact with the environment, which interacts with allergens and pathogens. The intercellular junctions of the conjunctival epithelium are the first line of defense against these agents, and below this is the substantia propria that presents different types of innate defense cells. Conjunctivitis is the inflammation of the conjunctival tissue and the most common causes of conjunctivitis are those caused by viruses, bacteria and allergens. Adenovirus is the most common of the viruses. Infection through the eye is possible thanks to receptors in the conjunctival epithelium, to which the virus can bind [7].
Likewise, the mechanism of entry of coronaviruses into cells occurs through the receptor for angiotensin-converting enzyme 2 (ACE-2). This is not only present in the alveolar epithelium, but also in the conjunctiva and the cornea [8-12].
The presence of the SARS-CoV-2 virus has been described in the tears of patients with COVID19. A nonspecific conjunctivitis has also been described in 0.8 to 1% of cases, considered one of the presentation scenarios of the disease [10,11]. There is little evidence on the role that the ocular pathway may have in the spread of SARS-Cov2. It is not known what the actual viral load an infected person has in the tear or the amount of virus that is necessary on the ocular surface for infection to occur.
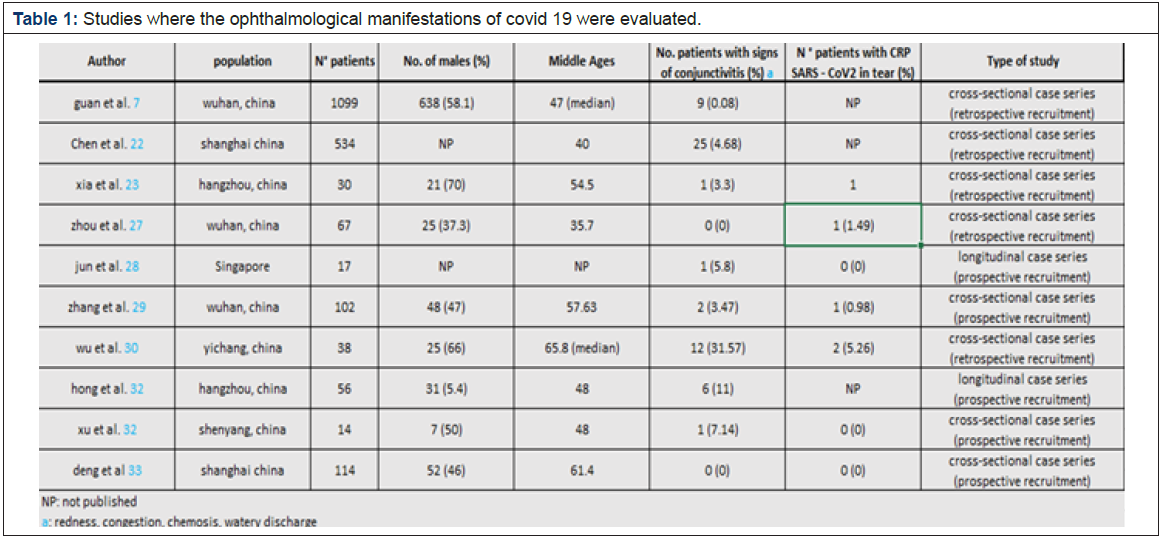
Thus, the first reference to conjunctivitis due to SARS-CoV-2 is in a letter to the editor, published in the journal TheLancet, in which the picture of unilateral eye redness is described in an expert pulmonologist (wearing his protective equipment and an N95 mask, but without protective glasses), days after visiting a hospital in Wuhan. Later he developed pneumonia. Since then, numerous clinical cases and case series have been published, most by Chinese authors, as evidenced in Table 1 [12-18]. (Table 1).
In the same way, Alió, in a press interview, clarifies in his main conclusions that SARS-Cov-2 can cause two types of conjunctivitis: one of them is caused by direct exposure to the pathogen and that is positive in taking sample and performing PCR; However, there are patients with a diagnosis of COVID-19 but the coronavirus does not appear in their tears and they present a picture of conjunctivitis. In this case, it is not a viral conjunctivitis as such, but is part of the general inflammation suffered by severe patients after an exaggerated immune response. Conjunctivitis is part of the clinical picture of COVID-19 and can even be the first symptom in many cases in 20% of patients, according to Alió, although other estimates do not exceed 3%. The patient reports the sensation of a foreign body, red eye and tearing. During the SARS epidemic, ocular exposure to infectious fluids was associated with an increased risk of transmission of SARS-CoV to healthcare workers. Although the SARS-CoV RNA was found Occasionally in ocular samples during the early phase of the disease, its ineffectiveness is unknown [10].
On the other hand, in a recent work published in Spain, it is found that 16.1% of the staff of the ophthalmology departments of the province of Granada (Spain) fell ill with COVID-19, compared to 11.2% of all the staff studied at the Hospital Clinico (Barcelona, Spain), one of the reference centers in Spain for the diagnosis and treatment of COVID-19 [11]. It should be noted that, at that time, Barcelona was one of the epicenters of the pandemic, along with Madrid, and that Granada was not. This provides more arguments in favor of the possible transmission of SARS-CoV-2 through the tear, since, with the personnel supposedly less at risk due to not attending the emergency room or plants destined for COVID patients, they presented a percentage of major infection [12].
In order to better determine the behavior of this virus and its affectation at the ophthalmological level, multiple comparisons have emerged with other coronaviruses, mainly SARS-CoV-1, which produces severe acute respiratory syndrome (SARS), and with the Medium respiratory syndrome virus. East (MERS-CoV). Both have been found in tear secretions, conjunctival and corneal cells11, but conjunctivitis in humans has not been described [13]. Some conjunctival congestion without excessive redness and a slight increase in tear secretion, lasting a few days, was only described in isolated cases [14]. The SARS-CoV-2 genome is 75-80% similar to that of SARS-CoV-1 and 40% similar to that of MER, it would be expected that the behavior at the ocular level would be the same.
However, unlike its predecessors, SARS-CoV-2 can cause more severe conjunctivitis, with marked cilioconjunctival hyperemia, superficial punctate keratitis, tarsal conjunctival follicles and even pseudomembranes as seen in (Figure 1) [15]. There may be edema of the lid margin and mucous discharge. The finding of lymphadenopathy has not been published, but, as it is a viral infection, they may possibly be present. The incubation period of the virus ranges from 5 to 14 days [16]. It can occur in isolation, as a prodrome of respiratory infection and even appear after the onset of systemic symptoms. The time of evolution of the ocular symptoms is also variable, having described remissions between 5 and 20 days [17] (Figure 1).
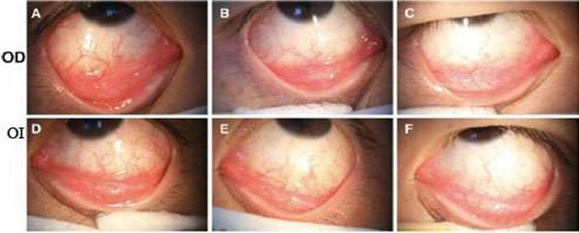
Figure 1: Biomicroscopic examination, showing evidence of bilateral viral conjunctivitis in a SARS-Cov-2 positive patient.
Note*: A and D: Condition with moderate conjunctival injection. Eyelid follicles. B and E: Significant clinical evolution 17 days after infection. C and
F: On day 19, gradual, favorable clinical evolution of treatment with ribavirin.
In addition, Brazilian scientists have described in The Lancet some alterations in the retina of COVID-19 patients using OCT, and have found micro bleeds and lesions at the level of the ganglion cell layer and the internal plexiform, but in a very isolated way. More however, it must be taken into account that it can be presented [17- 21].
Treatment of Conjunctivas by SARS-COV-2
There is no specific treatment. Chen et al. [18] used rivabirin eye drops 4 times a day for 6 days in a 30-year-old man who had already been diagnosed with COVID-19 14 days earlier. They observed a complete remission of eye symptoms on the fifth day of treatment. Shetty, et al. [19-20] comment on the possibility of using topical hydroxychloroquine (0.03%), since it has already been used in dry eye syndrome, with no recorded adverse effects. In relation to the possible harmful effect of its oral administration in patients with pneumonia, a letter to the editor was recently published in the American Journal of Ophthalmology [20].
Conclusion
After our review of the literature, it was possible to conclude that conjunctivitis is the main ophthalmological manifestation caused by SARS-CoV-2, however its prevalence is very low in relation to the magnitude and prevalence of the rest of the manifestations caused by the virus. It could be related to a more serious form of disease. The ophthalmic route of transmission is possible, but not very relevant compared to the airway and by contact with contaminated hands and surfaces. Pneumonia acquired by direct ophthalmic transmission is unlikely. The main repercussion of suffering from isolated conjunctivitis is the epidemiological control of the disease, rather than the ocular repercussions. Given the evidence of SARSCoV- 2 transmission through ocular tissue, even in the absence of conjunctivitis, ophthalmological associations advise eye protection with the use of protective glasses (in addition to protective equipment and a mask).
Conjunctivitis in these patients usually has a good evolution, but in some it can be aggravated even with toxic shock. The factors that determine this worsening are still to be elucidated with future research. Close monitoring of these patients is therefore essential.
Although manifestations such as retinal microbleeds and lesions at the level of the ganglion cell layer and the internal plexiform were also found in a very isolated case, but the documented information is scarce on this issue, other researchers are motivated to continue studying these future manifestations.
References
- Zhou W (2020) The coronavirus prevention Handbook. 101 Science-based tips that could save your life.
- Mejia CR, Rodríguez Alarcon JF, Garay Ríos L, Enríquez Anco Md, Moreno A, Huaytan Rojas K, et al. (2020) Perception of fear or exaggeration transmitted by the media in the Peruvian population during the COVID-19 pandemic. Rev Cubana Invest Bioméd 39(2).
- Aquino Canchari CR, Medina Quispe CI (2020) COVID-19 and education in medical students. Rev Cubana Invest Bioméd 39(2): e758.
- Kamps BS, Hoffman CH (2020) COVID Reference. Steinhauser Verlag.
- (2020) Spanish Society of Ophthalmology. Recommendations for the care of ophthalmological patients in relation to the COVID-19 emergency.
- Lu CW, Liu XF, Jia ZF (2020) 2019-nCoV transmission through the ocular surface must not be ignored. Lancet 395(10224): e39.
- Wang W, Xu Y, Gao R, Roujian Lu, Kai Hane, et al. (2020) Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 323(18): 1843-1844.
- Olivares JP, Garza M, García G, Azcárate T, Penniecook J, et al. (2020) Recommendations for the management of patients requiring ophthalmological care during the SARS-CoV-2 pandemic. Rev Mex Oftalmol 94(3): 103-112.
- Peng Y, Zhou YH (2020) Is novel corona1virus disease (COVID-19) transmitted through conjunctiva? J Med Virol 92(9): 1408-1409.
- Amesty MA, Alió del Barrio JL, Alió JL (2020) COVID-19 disease and ophthalmology: An update. Ophthalmol Ther 9(3): 1-12.
- Garcia Basteiro AL, Moncunill G, Tortajada M, Vidal M, Guinovart C, Jiménez A et al. (2020) Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. Nat Commun 11(1): 3500.
- Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA (2012) Isolation of a novel coronavirus from a manwith pneumonia in Saudi Arabia. N Engl J Med 367(19): 1814-1820.
- Yuen KSC, Chan WM, Fan DSP, Chong K, Sung J, et al. (2004) Ocular screening in severe acute respiratory syndrome. Am JOphthalmol 137(4): 773-774.
- Seah I, Agrawal R (2020) Can the coronavirus disease 2019(COVID-19) affect the eyes? A Review of coronaviruses andocular implications in humans and animals. Ocul ImmunolInflamm 28(3): 391-395.
- Cheema M, Aghazadeh H, Nazarali S, Ting A, Hodges J, et al. (2020) Keratoconjunctivitis as the initial medicalpresentation of the novel coronavirus disease 2019(COVID-19). Can J Ophthalmol 55(4): e125-e129.
- Daruich A, Martin D, Bremond Gignac D (2020) Unilateralconjunctivitis as first presentation of coronavirus disease2019 (COVID-19): A telemedicine diagnosis. J Fr Ophtalmol 43(5): e167-e168.
- Chen L, Liu M, Zhang Z, Qiao K, Huang T, et al. (2020) Ocularmanifestations of a hospitalised patient with confirmed 2019novel coronavirus disease. Br J Ophthalmol 104(6): 748-751.
- Lu C, Liu X, Jia Z (2020) 2019-nCoV transmission through the ocularsurface must not be ignored. Lancet 395(10224): E39.
- Chen L, Liu M, Zhang Z, Qiao K, Huang T, et al. (2020) Ocularmanifestations of a hospitalised patient with confirmed 2019novel coronavirus disease. Br J Ophthalmol 104(6): 748-751.
- Shetty R, D’Souza S, Ganesan Lalgudi V (2020) What ophthalmologists should know about conjunctivitis in theCOVID-19 pandemic? Indian J Ophthalmol 68(5): 683-687.
- Marinho PM, Marcos A, Romano AC, Nascimento H, Belfort R (2020) Retinal findings in patients with COVID-19. The Lancet 395(10237): 1610.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.