Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Phlegmasia Cerulea Dolens as A Complication of Severe Pneumonia Because Of SARS Cov-2
*Corresponding author: Irena Jimenez Velasco, Department of Emergency, Hospital Virgen de la Salud, Toledo, Spain.
Received: October 04, 2021; Published: October 14, 2021
DOI: 10.34297/AJBSR.2021.14.002000
Abstract
Novel Coronavirus Disease 2019 (COVID-19) is a global pandemic with more than 4 million positive cases across the globe. Recent retrospective studies suggest an increased risk for venous thromboembolism in patients with COVID-19. We report a case of a woman with a phlegmasia cerulean dolens as a complication of severe pneumonia because of SARS-CoV-2, probably related to diagnosis delay. Phlegmasia cerulea dolens is a manifestation of massive venous thrombosis associated with a high amputation rate, pulmonary embolism, and a mortality rate of over 40%. Emergency physicians should be aware of these complications when evaluating a patient with COVID-19.
Keywords: COVID-19; Coronavirus; Venous Thromboembolism; Phlegmasia Cerulean Dolens; Respiratory WHO; Hospitalized; Physicians; Diagnosis; Hypertension; Humerus
Introduction
In late December 2019, an epidemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) began in Wuhan and spread rapidly throughout the world [1]. The World Health Organization (WHO) declared the 2019 Coronavirus Disease (Covid-19) pandemic on March 11, 2020 [2]. Patients affected by Covid-19, both hospitalized and outpatient, are at high risk of venous and arterial thromboembolic disease due to hyperinflammation, hypoxia, immobilization, and Disseminated Intravascular Coagulation (DIC) [3-7] We present a clinical case in which an unfavorable evolution of a thromboembolic complication appears, probably related to the delay in its diagnosis. The relationship between covid-19 and thromboembolic disease has been increasingly described. Our case emphasizes the need to keep a high suspicion for COVID 19 when compatible symptoms of thrombosis appear and show the severity of associated complications, which can help emergency physicians in their rapid identification.
Case Report
83-year-old woman with a personal history of hypertension (AHT), Chronic Obstructive Pulmonary Disease (COPD), a pacemaker carrier for complete AV block, stage 3 chronic kidney disease (Kidney Disease Outcome Quality Initiative guidelines) secondary to nephroangiosclerosis in follow-up by Nephrology and prosthesis in the left shoulder after fracture of proximal humerus 8 years ago. She went to the ER for severe pain in her lower left limb, which has been worsening progressively for 5 days. The patient contacted with primary care, who prescribed analgesia with acetaminophen and metamizole without improvement in symptoms. She also reports that she had moderate effort dyspnea and a low-grade fever for 15 days. She denied the presence of cough, expectoration, and gastrointestinal symptoms. As epidemiological background, her husband was being followed for respiratory symptoms like the one presented by the patient.
On examination her blood pressure was 145/81 mmHg, pulse rate was 93/min, temperature was 36.4°C and blood Oxygen Saturation (SpO2) was 85% in room air, which was corrected with oxygen supplement. Pulmonary auscultation detected the presence of generalized bilateral snoring. Normal abdominal examination. She presents edema, coldness, cyanosis, and the appearance of skin blisters in the lower left limb (Figure 1). She maintains motility and the arterial pulses are palpable in the 4 extremities. Figure 1. Lower left limb with edema, coldness, and cyanosis. Laboratory tests showed elevated white-cell count (14.000 cells per cubic millimeter), lymphocites was 1.500 cells per cubic millimeter, anemia (hemoglobin level 10 g per deciliter) and normal platelet count (282.000 per cubic millimeter). The C-reactive protein level was elevated at 263mg per liter, procalcitonin level was elevated at 2.45ng per mililiter. Lactatedeshydrogenase was elevated at 618U per liter. D-dimer was elevated at 38.965 nanogram per liter with normal prothrombin and activated partial thromboplastin times. Liver-function tests were normal.
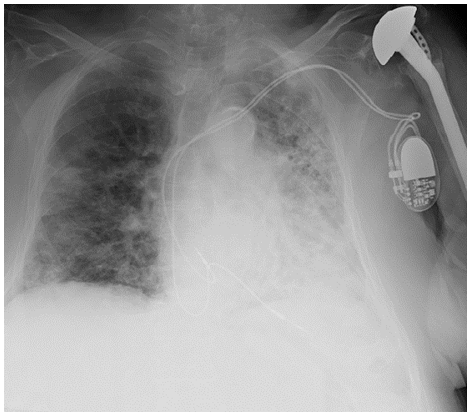
Portable chest radiograph shows predominantly left bilateral parenchymal lung involvement, with extensive diffuse consolidation in the left parenchyma and ground-patched ground opaque patches with right patches (Figure 2). A serological test was performed to detect SARS CoV-2 where it presented positive IgM and IgG. Doppler ultrasound of the lower limbs was performed, showing the absence of compressibility in the popliteal vein suggestive of deep vein thrombosis with arterial permeability. Based on the observed findings, the diagnosis of severe bilateral pneumonia due to SARS CoV-2 and phlegmasia cerulean dolens in the lower left limb is established. The patient was admitted and it was decided to start treatment for covid-19 with hydroxychloroquine 400mg and opting for conservative treatment for phlegmasia cerulean dolens with unfractionated heparin 15.000U and intravenous amoxiclineclavulanate 1g. The patient presented poor evolution, dying 5 days after admission.
Discussion
Patients with Covid-19 involvement usually present symptoms of acute respiratory infection. Venous Thromboembolic Disease (VTE) in hospitalized patients with Covid-19 is an emerging problem, affecting between 15% and 31% in the first 14 days of infection [6,7] Immobilization caused by the disease, dehydration, acute inflammatory status, and the presence of other cardiovascular risk factors are common in patients with Covid-19. This, along with possible endothelial cell damage due to virus binding to the ACE2 receptor, may increase the risk of VTE. Clotting disorders occur relatively frequently among Covid-19 patients, especially those with severe disease. Elevated D-dimer levels may reflect the severity of infection and are associated with complications in patients with community-acquired pneumonia [4]. Phlegmasia cerulea dolens is a rare and serious manifestation of massive venous thrombosis. Its classic presentation is based on intense pain, significant edema, and cyanosis [8]. It is associated with a high amputation rate (50%), pulmonary embolism (22%) and a mortality rate of over 40% [9].
Conclusion
Thromboembolic disease has been highly described in relation with covid-19. This case illustrates the importance of being vigilant of symptoms of thrombosis to prevent severe associated complications.
Conflict of Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Conflict of Interests
None
References
- Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, et al. (2020) Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 191: 145-147.
- World Health Organization. Director-general's remarks at the media briefing on 2019-nCoV on 11 May 2020.
- Anastasios K, Konstantinos GK, Evangelos D, Garyphallia P, George S (2020) Thromboembolic risk and anticoagulant therapy in COVID-19 patients: Emerging evidence and call for action. Br J Haematol 189(5): 846-847.
- Terpos E, Ntanasis Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, et al. (2020) Hematological findings and complications of COVID‐19. Am J Hematol 95(7): 834-847.
- K Casey, A Iteen, R Nicolini (2020) COVID-19 pneumonia with hemoptysis: Acute segmental pulmonary embolism associated with novel coronavirus infection. Am J Emerg Med 38(7): 1544.e1-1544.e3.
- Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, et al. (2020) Incidence of Venous Thromboembolism in Hospitalized Patients with COVID-19. J Thromb Haemost 18(8): 1995-2002.
- Chen T, Wu D, Chen H, Yan W, Yang D, et al. (2020) Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ.
- Hsin Ti, Shu Hung H (2018) Phlegmasia Cerulea Dolens with Compartment Syndrome. N Engl J Med 378: 658
- Ayman S, Abdullah Saleh, Ehab Elashaal, Humood, Ibrahim, et al. (2019) The ugly face of deep vein thrombosis: Phlegmasia Cerulea Dolens-Case report. Int J Surg Case Rep 59: 107-110.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.