Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Importance of Early Treatment for COVID-19
*Corresponding author: Youngah Choi, Department of Internal medicine, Seoul Metropolitan Seobuk Hospital, Seoul 03433, Korea.
Received: September 24, 2021; Published: October 21, 2021
DOI: 10.34297/AJBSR.2021.14.002010
Abstract
Between March 2, 2020, and August 31, 2021, 2,498 COVID-19 patients have been admitted to Seobuk Metropolitan Hospital, of which 2,285 have been discharged. 23 were transferred to a life treatment center or other hospital due to constraints on the hospital beds or for family together admission. 190 patients, almost 7.6% of the total number, needed to be transferred to a university hospital because of the severe progression of their pneumonia. The Korean quarantine system hospitalizes COVID-19 patients in the early stages of the (COVID-19) disease. We believe that it is due to this system that Korea has been able to keep a considerably low death rate compared to many other countries. In this paper we examine the results of the chest CT scans of all 1,523 corona patients hospitalized from March 2, 2020, to May 25, 2021. We charted the data of the 1,523 patients to look into comorbidities. We used a systemic classification to analyze the data of the existing comorbidities of inpatients and their diseases diagnosed at the time of hospitalization. The purpose of this study is to explain the disease pattern of COVD-19 by looking at the accompanying diseases of the patients as well as at their newly diagnosed diseases. In our approach, we have found it important to administer monoclonal antibody Regdanvimab(Regkirona) at the earliest possible stage of the infection. We also reviewed the charts of 2,498 COVID-19 patients between March 2, 2020, and August 31, 2021, for investigating efficacy of monoclonal Ab and antiviral agent. We administered the antiviral drug, Veklury (Remdesivir) the minute the oxygen saturation begins to drop. It is important to start these treatments at least 7-10 days after the onset of symptoms. The Korean quarantine system allows patients to be hospitalized and observed immediately after being diagnosed with COVID-19. This treatment at the initial stage of COVID-19 is what is believed to have kept the death toll in Korea considerably lower than in other countries [1].
Introduction
Today, on September 6, 2021, the total cumulative number of COVD-19 patients in the Republic of Korea is 263,374 and the death toll stands at 2,330. The mortality rate is 0.88%. In the Republic of Korea, the COVID-19 vaccine was first administered in April 2021 to the elderly and vulnerable (including patients in nursing homes for homeless and disabled people), as well as to hospital and other government quarantine facilities staff members. Nowadays, the number of COVID-19 patients under the age of 60 who are not yet fully vaccinated has increased compared to the age pattern of patients we had in 2020 [2].
A person who has been tested positive to the corona virus, is transferred to one of the designated hospitals for infectious diseases or a life treatment Center within the shortest time possible. If they are over 60 years old, or younger but with an already existing medical condition, they will be transferred to an infectious disease hospital. If the patient is under 60 and has no underlying diseases, he or she is transferred to a life treatment center first. If the patient develops any severe symptoms while staying at the life treatment center, he or she will be transferred to one of the infectious disease hospitals. As of today, September 6, 2021, there are 7 Seoul city governmental hospitals and 13 other hospitals which are designated as COVID-19 hospitals in the Seoul city and Gyeonggi -do area. 1,808 patients are hospitalized. As of September 6, 2021, there are 14 life treatment facilities operating in the Seoul city and Gyeonggi -do area with a current number of 1,951 corona patients quarantined.
Seoul Metropolitan Seobuk Hospital is a hospital which is directly managed by the Seoul Metropolitan Government and has mainly been treating homeless people and tuberculosis patients. It is a public hospital providing primarily inpatient and outpatient treatment for the elderly and vulnerable people groups, including the homeless and the disabled. From March 2, 2020, to August 31, 2021 2,498 COVID-19 COVID-19 patients have been admitted to Seobuk Metropolitan Hospital and which 2,285 patients have been discharged.
During the last two months, the number of daily confirmed COVID-19 patients in Korea has been over 1,500 and our hospital continue to treat many patients, daily filling the available hospital beds. As soon as COVID-19 inpatients are diagnosed through a corona test, inpatient treatment at an infectious disease hospital will be maintained for an average of 7-14 days after which, being released from isolation, patients are discharged.
COVID-19 patients’ living costs are fully covered by a governmental fund during the patients’ stay at an infectious disease hospital or a life treatment center. In other countries, including the United States, most patients are usually only admitted to hospital and receive treatment when their disease reaches a more severe status, when they are in need of oxygen therapy or even a ventilator. In the Republic of Korea, however, the quarantine system operates in such a way that isolation and treatment begin at a life treatment center, or a hospital dedicated to COVID-19 within 1-2 days of receiving a positive corona test result [3].
Materials and Methods
In this article, we would like to talk about the disease patterns of hospitalized COVID-19 patients. We also talk about the symptoms and physical signs of the patients who already have an underlying disease. We analyze the charts of 1,523 patients who received inpatient treatment at our hospital between March 2, 2020, and May 25, 2021. We examine the comorbidities applying a systemic classification by analyzing the data of the existing comorbidities of inpatients and their diseases diagnosed at the time of hospitalization. We use the results of the chest CT scans of all 1,523 corona patients hospitalized from March 2, 2020, to May 25, 2021. In November 2020, we started to administer the antiviral agent Veklury (Remdesivir) as well as steroids, including Dexamethasone injections. In Febuary 2021, we also began with the administration of the monoclonal antibody treatment Regdanvimab (Regkirona). We also reviewed the charts of 2,498 COVID-19 patients between March 2, 2020, and August 31, 2021, for investigating efficacy of monoclonal Ab treatment Regdanvimab (Regkirona) and antiviral agent Veklury (Remdesivir).
Results
The tables below show a classification of pre-existing diseases the patients had before contracting the virus, as well as those diagnosed during hospitalization. In addition, we also discuss the difference between the clinical picture of COVID-19 itself and the clinical picture due to accompanying diseases.
Comorbidities or newly diagnosed diseases of COVID-19
We had expected that the course of the COVID-19 disease would differ depending on the patient’s age and pre-existing medical condition, but this was not necessarily the case. Young patients with no pre-existing disease and in otherwise good health, can develop a COVID-19 disease pattern that is often rapid and very severe, whereas in many cases, elderly patients with multiple chronic diseases can overcome COVID-19 well and without any major complications and sequelae.
In this paper, we analyze the data of the 1,523 patients hospitalized in Seobuk Metropolitan Hospital between March 2, 2020 and May 25, 2021, according to diagnosed diseases, diseases diagnosed by clinical features during the time of hospitalization, the patients’ past history and current medication. We describe the existing and past diseases as well as the COVID-19 related diseases of the COVID-19 patients who were admitted to the hospital.
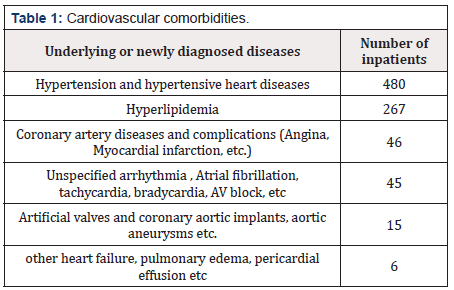
Tables 1 to 8 summarize the diagnoses according to a systemic disease classification(Table 1)
The most common underlying cardiovascular diseases were hypertension, hyperlipidemia, coronary artery disease, arrhythmia, and artificial valves or implants. Many patients with a prior coronary artery implant suffered from high blood pressure and increased pulse rate due to COVID-19 infection status. The COVID-19 disease itself increases the association between the onset of cardiovascular diseases and blood clots, as well as the frequency of overall cardiovascular diseases, and creates many situations that require medication. In most cases, the patients were instructed to continue with their medication even after being discharged and to conduct a follow-up examination (Table 2).
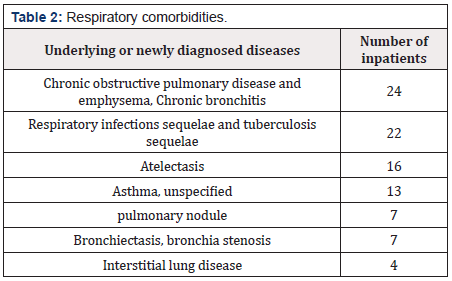
Respiratory diseases such as chronic obstructive pulmonary disease, emphysema, sequelae of tuberculosis, asthma, and bronchiectasis were common accompanying underlying diseases. For all COVID-19 patients hospitalized, chest CT scans are conducted to check the progress of the disease and to detect any underlying lung disease. In some cases, the follow up examination after discharge confirms a resolved pneumonia or lung lesions (Table 3) [4].
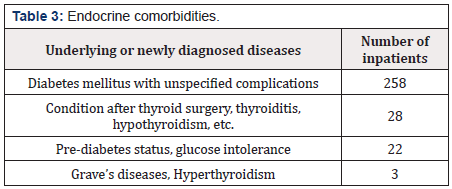
Diabetes mellitus is the most common endocrine accompanying underlying disease. Many patients are hospitalized and diagnosed with diabetes. COVID-19 disease itself can be an extremely stressful situation, which in itself can easily provoke the development of diabetes. In addition, the treatment for COVID-19 itself (Dexamethasone) causes increased blood sugar during treatment. Patients need to receive long-term diabetes or glucose intolerance status follow-up after their discharge from hospital (Table 4).
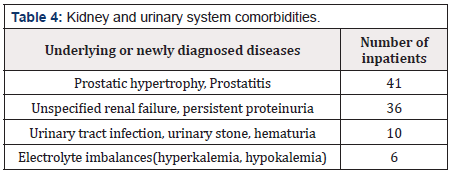
Several patients with an underlying disease of the kidney urinary system had chronic renal failure and had to continue on with medication. The corona disease itself generally causes persistent high fever, along with difficulties in ingesting food and water. COVID-19 patients frequently present very severe dehydration problems which can lead to a damage of their kidney function. Treatments such as electrolyte and dehydration correction are required (Table 5).
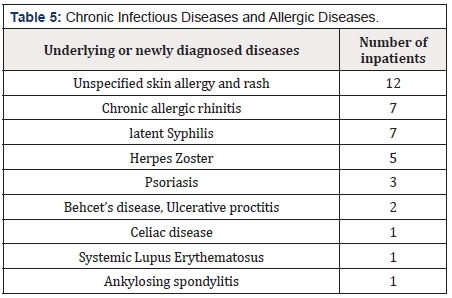
In patients with pre-existing, well controlled chronic infectious and allergic diseases, sometimes symptoms similar to their own disease develop. We saw both the original underlying disease flare up as well as the appearance of new skin rashes occur during hospitalization due to COVID-19. In many cases, patients’ reactions to the corona virus itself are also perceived as individual allergies or anaphylaxis-like reactions. These symptoms usually disappear when they recover from COVID-19 (Table 6).
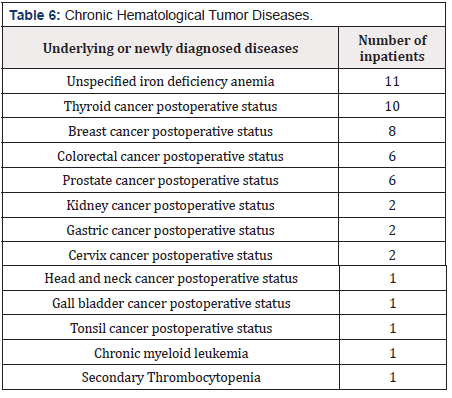
We didn’t find any special complications for patients who had completed cancer surgery and chemotherapy 2-3 years prior to contracting the corona virus. However, as for any other patient, the amplified viral load, the high fever and the prolonged severe inflammation causes a temporary thrombocytopenia and a decrease in the count of neutrophils along with the sepsis. These parameters return to normal as the patient recovers from Corona (Table 7).
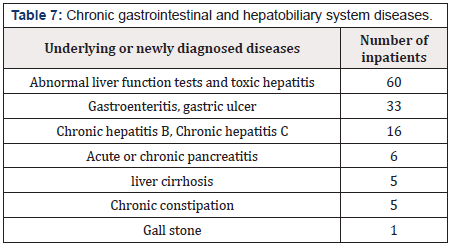
An elevated liver function is a commonly diagnosed pathology during hospitalization, indicating the accompanying underlying disease of a toxic hepatitis due to the COVID-19. Patients who confirmed that their liver function tests were normal before admission, as well as patients with existing chronic diseases, such as hepatitis B, hepatitis C and cirrhosis, whose liver function levels were maintained at near normal levels before the outbreak of COVID-19, often experienced a rise in the liver function parameters attributed to the COVID-19 infection. The most common digestive symptoms during hospitalization were diarrhea, nausea and vomiting. Loss of taste and loss of smell and poor oral intake are also common (Table 8).
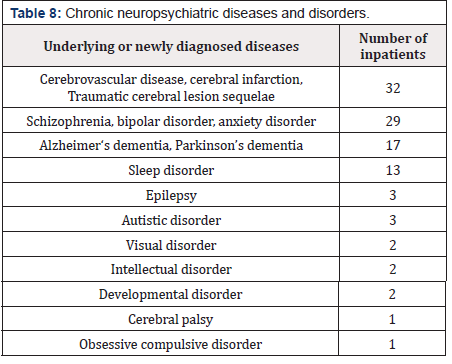
Patients with an underlying cerebrovascular and psychiatric disease suffer from a long-term chronic disease and have to be hospitalized with the caregiver family member due to their paralysis or disability. The process of isolation and communication with bedridden and psychiatric patients is very challenging and difficult due to their psychiatric problems and disabilities, but we do not think that the underlying diseases had much influence on the diagnosis, clinical picture, and medication process of COVID-19 [5-7].
CT findings of COVID-19
In general, we performed two or three CT scans to confirm the diagnosis and treatment efficacy about pneumonia during the time of hospitalization. A chest CT scan usually confirms the increase or decrease of the pneumonia. We analyze the data of the 1,523 patients hospitalized in Seobuk Metropolitan Hospital between March 2, 2020 and May 25, 2021. 1,236 out of 1,523 patients had pneumonia. 285 patients did not have any pneumonia. 244 of the 1,523 patients received oxygen therapy, including high flow therapy. Many patients’ pneumonia improved with the administration of monoclonal antibody Regdanvimab (Regkirona) therapy, antibiotics, and fluids, oxygen therapy and antiviral Veklury (Remdesivir) treatment.
Oxygen therapy and therapeutic agents for COVID-19 patients
We would also like to examine how oxygen therapy has been implemented and how many patients developed pneumonia during their time of hospitalization. Patients admitted to the hospital are given a finger pulse oximeter which allows them to check and record their O2 saturation several times a day by themselves. Oxygen is sometimes used intermittently for chest tightness even when the oxygen saturation parameter is over 95% to improve the patient’s subjective well-being. However, when the oxygen saturation parameter drops to below 94% in room air, oxygen therapy must be administered. At that point we usually also start with an antiviral Veklury(Remdesivir) treatment. By starting oxygen supply, the saturation can be maintained above 94%. As high fever continuing means the pneumonia progression and the pneumonia progresses, oxygen demand also increases while the improvement of the pneumonia lets the oxygen demand decrease. If, because of high oxygen demand, the oxygen saturation cannot be maintained above 95 % by using a reservoir mask of 5L/min, we start to use a high flow O2 machine to increase the O2 supply. If the oxygen saturation cannot be maintained above 95 % by using a high flow O2 machine at its highest level, the COVID-19 patients have to be transferred to a university hospital for ventilator and ECMO therapy. As the COVID-19 pneumonia improves, oxygen demand also decreases and oxygen tapering and stopping become possible. The patients are usually discharged when their oxygen saturation is higher than 95 % at room air without oxygen therapy. The purpose of this study is also to analyze the data of therapeutic agents during the patients’ hospitalization period.
The COVID-19 patients hospitalized at our hospital from early March 2020 to July 2020 were usually young and came from abroad. Many of them did not have severe symptoms. We implemented general treatments (analgesic, antipyretic, antibiotic, antihistamine, fluid therapy, etc.) used to treat common respiratory infections (bacteria, virus). We used Kaletra, which is an antiviral drug given for AIDS treatment, on 686 corona virus patients between March 2020 and April 2021. Many patients discontinued this treatment halfway through because of its harsh side effects such as diarrhea and anorexia. At that time, we believed that Kaletra would reduce the viral load, but we finally came to the conclusion that it did not help much. From August 2020 on, we saw a rise in hospitalization of many elderly, medically chronic patients, and patients with worsening symptoms and other drugs were recommended as treatments. In August 2020, many COVID-19 patients were in need of other antiviral drugs.
In November 2020, we started to administer the antiviral agent Veklury (Remdesivir) as well as steroids (Dexamethasone etc.) injections. In March 2021, we began with the administration of the monoclonal antibody treatment Regdanvimab (Regkirona). The monoclonal antibody treatment Regdanvimab (Regkirona) is the preferential prophylactic treatment for severe forms of pneumonia and is administered in the case of a pneumonia with a maintained oxygen saturation above 95% in room air and symptoms occurring within 7 days. In case of pneumonia with oxygen saturation falling below 94% in room air, we start oxygen therapy and also start to use Veklury (Remdesivir) as an antiviral agent together with a Dexamethasone injection of 1.2 mg for 5 days. The dose of Dexamethasone is gradually decreased within 10 days. It usually takes one or two weeks for the pneumonia to improve and the oxygen saturation to be restored to normal level.
We reviewed the charts of 2,498 COVID-19 patients between March 2, 2020, and August 31, 2021, for investigating efficacy of monoclonal Ab and antiviral agent. We applied a 1 day scheduled use of Regdanvimab (Regkirona) on 710 patients, a 5-day scheduled use of Veklury (Remdesivir) on 359 patients and a 5-day scheduled use of Dexamethasone injection on 441patients.
Treatment progress of inpatients
The average time of hospitalization of the 2,498 COVID-19 patients between March 2, 2020, and August 31, 2021, was between two and three weeks. Of the 2,498 patients, 2,285 were discharged to home after being cured and 23 were transferred to a life treatment center or other hospital due to constraints on the hospital beds. It was too early to release them from quarantine, but they did not otherwise have any severe problem with COVID-19 itself. 190 patients, almost 7.6 % of the total number, needed to be transferred to a university hospital because of the severe progression of their pneumonia.
Discussion
Human-to-human transmission is assumed to be the primary route of infection, but a number of research results suggesting the possibility of airborne transmission have recently been published. It is known that an infection with the COVID-19 virus is most contagious just before the onset of symptoms and in the early stages of the disease, and the infectivity is weakened 5 days after the onset of symptoms.
Patients whose symptoms of pneumonia develop within 7 days of admission, and whose oxygen saturation is maintained at 95% or above, will be administered a monoclonal antibody treatment Regdanvimab (Regkirona) first. If their fever rises as the pneumonia develops and their CRP rises above 3-5, they will be placed under the antibiotic Tazoperan for 5 or more days. If their oxygen saturation falls below 94% as the pneumonia progresses, they will be administered Veklury (Remdesivir) for about 5 days. During the 5 days of administration of Veklury (Remdesivir), the fever usually drops and the oxygen demand starts to decrease. It is difficult to predict who will develop a severe pneumonia and who won’t. Age or underlying diseases are not necessarily factors that cause the pneumonia to worsen. Of course, it is true that for elderly people with many underlying diseases, it is difficult to endure the ventilator treatment in the case of a severe pneumonia, so the mortality rate is high. Frankly speaking, we found that age, gender, nationality and underlying diseases are not predictors of disease severity. Obesity, however, is probably a risk factor in the progression of disease severity. From the clinical picture, it is true that high fever itself indicates that the pneumonia or other organ’s inflammation is progressing, and it is clear that oxygen saturation decreases rapidly as the pneumonia progresses. It is important to administer monoclonal antibody therapy Regdanvimab(Regkirona) in the earliest possible stage of the infection. Likewise, the antiviral drug, Veklury (Remdesivir) should also be administered at the moment in which the oxygen saturation begins to drop. In young people in particular, COVID-19 develops and progresses very fast, therefore the two drugs, Regdanvimab(Regkirona) and Veklury (Remdesivir) should be administered in the early phase of the disease. Early phase treatment including monoclonal antibody treatment and antiviral agent is very important to control the COVID-19 disease. The current quarantine system in the Republic of Korea allows COVID-19 patients to be treated in hospitals at the initial stage of their COVID-19 disease. Early treatment of COVID-19 disease is believed to have lowered the death rate considerably compared to many other countries [8,9].
In most cases, the course of the COVID-19 disease passes within 14 days of the COVID-19 diagnosis. Usually, the disease progresses rapidly and then patient recovers. Antiviral drugs, especially Veklury (Remdesivir) treatment, are effective in the early stages of COVID-19 disease. Monoclonal antibody treatment such as Regdanvimab (Regkirona) also helps prevent the disease from progressing to a severe form in the early stages of the disease. In many countries, hospital treatment is only started when the patient already presents breathing difficulties, yet we have seen that it is important that all these treatments should be given at least 7-10 days after the symptom onset.
Acknowledgement
None.
Conflicts of Interest
No Conflicts of interest.
References
- Andreas Rank, Athanasia Tzortzini, Elisabeth Kling, Christoph Schmid, Rainer Claus, et al. (2021) One Year after Mild COVID-19; The Majority of Patients Maintain Specific Immunity , But One in Four Still Suffer from Long term Symptoms. J Clin Med 10(15): 3305.
- Chieh Chen Wu, An Jen Lee, Chun Hsien Su, Chu Ya Huang, Mohaimenul Islam, et al. (2021) Statin Use Is Associated with a Decreased Risk of Mortality among Patients with COVID-19. J Clin Med 10(7): 1450.
- Joon Young Song, Jin Gu Yoon, Yu Bin Seo, Jacob Lee, Joong Sik Eom, et al. (2021) Ciclesonide Inhaler Treatment for Mild-to-Moderate COVID-19: A Randomized, Open-Label, Phase 2 Trial. Journal of Clinical Medicine 10(16): 3545.
- Talida Georgiana Cut, Cristina Tudoran, Voichita Elena Lazureanu, Adelina Raluca Marinescu, Raluca Dumache, et al. (2021) Spontaneous Pneumomediastinum, Pneumothorax, Pneumopericardium and Subcutaneous Emphysema-Not So Uncommon Comlications in Patients with COVID-19 Pulmonary Infection-A Series of Cases. J Clin Med 10(7): 1346.
- Giuseppe Lisco, Anna De Tullio, Assunta Stragapede, Antonio Giovanni Solimando, Federica Albanese, et al. (2021) COVID-19 and Endocrine System : A Comprehensive Review on the Theme. J Clin Med 10(13): 2920.
- Mehdi Ghasemi, Raffaella Pizzolato Umeton, Kiandokht Keyhanian, Babak Mohit, Nasrin Rahimian, et al. (2021) SARS-CoV-2 and Acute Cerebrovascular Events : An Overview. J Clin Med 10(15): 3349.
- Fabiola Atzeni, Ignazio Francesco Masala, Javier Rodríguez Carrio, Roberto Ríos Garcés, Elisabetta Gerratana, et al. (2021) The Rheumatology Drugs for COVID-19 Management : Which and When? J Clin Med 10(4): 783.
- Brunella Posteraro, Giulia De Angelis, Giulia Menchinelli, Tiziana D'Inzeo, Barbara Fiori, et al. (2021) Risk Factors for Mortality in Adult COVID-19 Patients Who Develop Bloodstream Infections Mostly Caused by Antimicrobial-Resistant Organisms : Analysis at a Large Teaching Hospital in Italy. J Clin Med 10(8): 1752.
- (2020) New Infectious Disease Central Clinical Committee, COVID-19 treatment recommendation, National Medical Center/Central Infectious Diseases Hospital Operation Center.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.