Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Artemether-Lumefantrine in combination with Arthrospira platensis as an Adjunct Therapy on Lipid Profile Parameters and Parasitaemia Levels in Children with Acute Uncomplicated Malaria
*Corresponding author: Theresia Njuabe Metoh, Department of Biochemistry, Faculty of Science, The University of Bamenda, Cameroon.
Received: February 16, 2022; Published: March 04, 2022
DOI: 10.34297/AJBSR.2022.15.002147
Abstract
Malaria being one of the most life-threatening diseases in Africa is of public health importance in Cameroon with Plasmodium falciparum species responsible for over 98% of deaths in children in this endemic zone. Changes in the lipid profile are commonly reported in malaria infected children and the use of artemisinin-based combination therapy has been one of the main strategies to curb the disease but has faced some challenges. Due to this effect, this study aimed to evaluate the effect of Arthrospira platensis (a cyanobacteria which has been known to demonstrate antimalarial and lipid modulatory effects) on the parasitaemia clearance rate and the lipid profile in Cameroonian children below 16 years of age. In an open labeled randomized clinical trial, enrolled participants who had lipid parameters within normal ranges (TC= <200 mg/dL, TG= <150mg/dL, LDL= <150mg/dL, HDL= >60mg/ dL), and individuals who had uncomplicated P. falciparum malaria were randomly assigned to receive: coartem (AL) only; AL and capsulated Arthrospira plantensis (AP) (4 x 500mg) dose for 3 days. On days 0, 1, 2 and 7 gametocytes were assessed and quantified by microscopy and quantification of lipid parameters by spectrophotometry. Data analysis was carried out using SPSS version 21.0. The overall findings showed that, parasite density affected lipid profile parameters with a significant average drop (TC: 150.5547mg/ dl to 90.8218mg/dl with p-value of 0.0239, HDL: 45.53333mg/dl to 22.3 p-value: 0.0306, LDL: 83.64667mg/dl to 47.67mg/dl p = 0.0413 and increase in TG from 104.259mg/dl 116.8733mg/dl p = 0.043). The values of lipid profile parameters (TC, HDL, and LDL) where seen to increase after treatment with AL but a significant increase was seen with those treated with AL+AP with mean±SD of TC (152.6344mg/dl): 152.63440±15.175355; p=0.0001, HDL(50.95mg/dl): 50.9500±9.703407; p=0.0001, LDL(84.877mg/dl): 84.87700±9.551049; p=0.0001 and a significant decrease in TG(84.037mg/dl) with mean±SD of 84.03700±25.032346 and p value of 0.292. Parasite density was seen to decrease in both groups from D0 to D7 but decreased more rapidly and significantly in the group receiving AL+AP compared to AL with mean difference of -3190; p-value 0.825, 12260; p-value 0.155, 90; p-value 0.0001 and 560; p-value 0.038 on D0, D1, D2 and D7. There was a strong negative correlation between parasite density and TC, HDL and LDL with r = -0.94373, -0.97221, and -0.98686 respectively and a strong positive correlation between parasite density and TG with r = 0.96412. Also, signs and symptoms of malaria were seen to clear off more rapidly in those receiving Arthrospira platensis than in those receiving just AL. Conclusively, Arthrospira platensis has lipid modulatory effects and works in synergy with AL for the treatment of uncomplicated malaria due to its antimalarial properties.
Keywords: Malaria, Arthrospira plantensis, Lipid Profile, Dietary Supplement.
Abbreviations: ACT: Artemisinin-Combined Therapy; AL: Artemether-Lumenfantrine; CI: Confidence interval; D: Day; DHAP: Dihydroartemisinine plus piperaquine; Hb: Hemoglobin; HDL: High Density Lipoprotein; HIV: Human Immunodeficiency Virus; ITN: Insecticide Treated nets; K-S: Kolmogorov-Sminov; LDL: Low Density Lipoprotein; LLINs: Long lasting insecticidal nets; N: Number; PCR: Polymerase Chain Reaction; RDT: Rapid Diagnostic Test; AP: Arthrospira platensis; TC: Total Cholesterol; WBCs: White blood cells; WHO: World Health Organization
Background
Malaria is still at the top list of Cameroon’s public health concerns and in other parts of the Sub–Saharan Africa despite all management measures put in place [1]. In the world, it still causes approximately 229 million cases annually, with 409,000 deaths reported [2]. It is the major cause of morbidity and mortality among the most vulnerable groups including children aged under 5years [2] with the major causative agent being Plasmodium falciparum responsible for about 95% of all malaria cases. In Cameroon, malaria is a public health challenge with more than 1,500,000 cases and 3162 deaths in health facilities per year [3]. The management of malaria involves preventive measures that aim at controlling the vectors such as use of insecticide-treated nets (ITNs), indoor residual sprays (IRS) and parasite elimination by use of conventional drugs including artemisinin monotherapies and artemisinin-based combination therapies (ACTs) [4,5] which have led to major changes in malaria epidemiology and vector biology [6]. Due to increase resistance to parasite ancient drugs such as Chloroquinin and mefloquine, ACT has been recommended as the first line treatment for patients infected with uncomplicated Plasmodium falciparum [2]. Artemether/Lumefantrine (AL) is one of the approved and most successful fixed dose ACT used in the treatment of uncomplicated malaria by P. falciparum. Unfortunately, recent partial artemisinin resistance has been reported which is seen to be characterized by slow parasitological response defined as delayed parasite clearance to treatment during the 3 days treatment with AL as recommended by the WHO as the stipulated time for complete parasite clearance from infected blood [7]. Early diagnosis and prompt treatment with an effective drug regiment remain important components of malaria control and elimination strategies [8]. In Cameroon, one of the recommended drugs for the treatment of uncomplicated malaria caused by Plasmodium falciparum, is AL which is commonly known as Coartem [9]. In research to evaluate the efficacy of Amodiaquine-Artesunate versus Artemether Lumefantrine against uncomplicated malaria in children less than 14 years in Ngaoundere North Cameroon reported that, both drugs were effective in parasite clearance and PCR-corrected cure rates were 100% and 96.4%. However, several laboratorial abnormalities occur in the course of the infection such as anemia, thrombocytopenia, methemoglobinemia, and lipid blood levels [10]. Metoh, et al., 2021, in a recent study to evaluate the efficacy and safety of Artemether-lumefantrine, Artesunatemefloquine vs Dihydroartemisinin-piperaquine in the treatment of P. falciparum malaria in children have shown that of these, dihydroartemisinine plus piperaquine (DHAP) is the preferred antimalarial treatment that plays an important role in the reduction of malaria transmission in children in Cameroon [11].
Changes in the lipid profile are associated with so many factors such as genetics, inflammatory diseases and infectious diseases. Recent studies carried out has proved that changes in lipid profile of malaria infected patients is a characteristic feature of the disease [12]. Patients with malaria were seen to present hypolipidemia; decreased levels of LDL and HDL and accompanied with increased levels of triglycerides. Such lipid profile changes have been seen to occur in the most prevalent species of Plasmodium as well as in complicated and uncomplicated cases. Other cases provide evidence of the effect of Plasmodium falciparum on the lipid profile of infected persons [12] since the malaria parasite cannot synthesis lipid de novo and so, it tends to scavenge the host lipids in its developmental stages, leading to a rapid decrease in the levels of lipid parameters in blood [13]. Recently, researchers have placed focus on harnessing and exploring beneficial effects of some plants and animal products for the treatment of numerous diseases such as hepatitis, diabetes, HIV etc. Arthrospira platensis, a cyanobacteria have been used as a nutraceutical as it has a high nutritive value and therapeutic ability in many cases like cancer, chronic arsenic poisoning, rhinitis [14], diabetes, hypertension, Human Immunodeficiency Virus (HIV) infections, and activation of the innate immune system, obesity, cardiovascular disease, and nonalcoholic fatty liver disease and to exhibit antimalarial effects [15]. Recent studies have shown that, Arthrospira platensis could be used not just as a food but also as an adjunct therapy in the medical domain to curb oxidative stress caused by AL used in the management of malaria [16]. Thus, with these numerous therapeutic potentials, this study aimed to investigate the effect of Arthrospira platensis combined with artemether-lumefantrine on the lipid profile of malaria patients and the clearance rate of parasite in the blood of children less than 16 years of age.
Methods
Study Area
The study was carried out in the Bamenda Regional Hospital, Azire Preventive clinic, Gilead Health Center and Vision Laboratory which are all based in Bamenda situated in the Northwest Region of Cameroon, where it functions as the regional administrative headquarter. Bamenda is found in Mezam division and located between latitudes 5056‟ to 5058‟ North of Equator and between longitude 100 08‟ and 10010‟ East of Greenwich Meridian [17]; and occupies a total surface area of 3,125 hectares [18]. It is bounded by Bafut subdivision to the North, flanked to the West by Mbengwi, to the South by Santa sub-division, to the Southwest by Bali subdivision and bordered by Tubah sub-division in the East.
Study Design
This study was a clinical trial study and was carried out from June 2021 to September 2021. This was a randomized open label clinical trial (longitudinal study) divided into 2 sections. The first section was to assess the lipid profile (total cholesterol, and triglycerides) status in malaria infected patients according to various age groups and the second section was to determine the effect of Arthrospira platensis on the lipid profile parameters (total cholesterol, high-density lipoprotein, low-density lipoprotein and triglycerides) and parasite clearance rate when used in combination with artemether–lumefantrine (AL) treatment regimen in children.
First section: Those enrolled in this study were individuals attending in the Bamenda Regional Hospital, Cameroon of all age groups divided into cases and control groups. The age groups were classified into six, that is, 0-15yrs, 16-30yrs, 31-45yrs, 46-60yrs,61- 75yrs, and +75yrs. Subjects, who presented clinical signs and were diagnosed with malaria in the laboratory were recruited for this study through random sampling as case group. Subjects without malaria were recruited as control group. Both patients and control were related in age and sex.
Second section: Those enrolled here were children from 3 to 15 years who had uncomplicated malaria with parasitaemia count above 2000 parasites/ul blood, and whose parents gave their proxy-informed consent. Participants were screened for the presence of co-infections that could lead to faulty results. Such individuals with co-infections were excluded from the study. The study was designed to have one control group and two treatment groups (Groups 1, 2 and 3). Upon meeting all enrolment criteria, participants were randomized to receive either of the two treatment regimens; (i) AL (Coartem; Novartis Pharma AG, Basel Switzerland- 20 mg artemether and 120 mg lumefantrine) as a standard and for the other group, therapeutic dose of AL and therapeutic dose of Arthrospira platensis (150 mg/kg) [19].
Sample Population and Randomization
Overall, of 144 participants included in this study, 75 were females and 69 were males. 72 were malaria positives of all age group giving a prevalence of 50% (72/144). Of the overall, 80 participants of all age groups were divided into 2 groups, 40 were study patients with positive malaria cases and 40 were the control group with negative malaria cases. Also, of the overall participants, a subset of 74 children between the ages of 3 to 15 belonging to the control and malaria infected group were selected for treatment. The children were enrolled and assigned to three groups (control, AL and AL+AP groups) randomly including 32 malaria positives to the study groups 2 and 3 (AL and AL+AP groups respectively) and 32 malaria negatives in the control group (Group 1). Follow-up was done for seven days for the assessment of parasite density and lipid profile.
Drug Administration, Treatment and Grouping
The 32 patients recruited as malaria positive cases were placed into two groups (groups 2 and 3). Group 2 received artemetherlumefantrine only while group 3 received artemether-lumefantrine together with capsulated Arthrospira platensis. Group one was made up of non-positive cases, that is children whose microscopic examination did not show the presence of P. falciparum or any other malaria species and were called normal individuals.
For group 2, artemether–lumefantrine was administered based on the manufacturer’s prescription which is based on the body weight of the child. The treatment lasted for a period of 3 days (72 hours) with a treatment interval of 8 hours as recommended by WHO. That is, drugs taken twice a day; morning and evening [8]. For 5 kg to less than 15 kg body weight, patients took one tablet as an initial dose, 1 tablet again after 8 hours and then 1 tablet twicedaily (morning and evening) for the following 2 days (total course of 6 tablets). For 15 kg to less than 25 kg bodyweight, two tablets as an initial dose, 2 tablets again after 8 hours and then 2 tablets twice-daily (morning and evening) for the following 2 days (total course of 12 tablets). For 25 kg to less than 35 kg bodyweight, three tablets as an initial dose, 3 tablets again after 8 hours and then 3 tablets twice-daily (morning and evening) for the following 2 days (total course of 18 tablets). For 35 kg bodyweight and above, four tablets as a single initial dose, 4 tablets again after 8 hours and then 4 tablets twice-daily (morning and evening) for the following 2 days (total course of 24 tablets). Each tablet of AL contains 20 mg of artemether and 120 mg of lumefantrine. For group 3, artemetherlumefantrine was administered the same way as in group 2. Arthrospira platensis was administered based on age ranges.
For follow–up, the treatment was initiated on D0 (enrollment Day) and participants were asked to return to study clinic on days 1, 2 and 7. On each follow-up day, study participants were assessed for any symptoms, possible adverse effects, concomitant medication, measuring axillary temperature and collecting blood samples. In case a participant did not show up at the clinic, a field worker was sent to the house to find out the reason and possibly to bring the participant at the clinic for clinical examination and sampling. At all visits, blood was collected by finger-prick for blood smears and 2mls of blood collected in red tubes for lipid parameter quantifications. A patients’ case report form was filled each day of follow up. This was to check for decrease of clinical signs of malaria (fever, temperature, vomiting, loss of appetite, abdominal pain, headache, dizziness and body weakness) and if there was any adverse effect of the drug administered.
Malaria Parasite Count Estimation
The method used for quantification or estimation of parasite density in enrolled patients was microscopy which was performed by counting parasites within a given number of microscopic fields against counted white blood cells (WBCs) within the same fields [20]. Because of the scant resources in malaria-endemic countries for the quantification of patients’ WBCs, an assumed WBC count of 8.0 x 109cells/l is used to quantify malaria parasite density which was the same value applied in this study. Blood samples were collected from patients on D0 upon recruitment by finger pricking using lancets and the slides labelled with patient ID number and day of collection. The blood was then made to drop on a clean sterilized microscopic slide (approximately 10ul) and a thick smear made in a circular motion. The slides were allowed to air dry before staining with giemsa. Air dried slides were fixed with methanol by dipping into the container of methanol for 2–3 minutes. The slides were then placed back-to-back in a staining trough containing giemsa solution making sure all fixed sample faced to one direction and allowed for 20 minutes. After which the slides were rinsed with clean water, allowed to air dry for 5minutes then viewed under the microscope. The slides were examined under the x100 oil immersion objective lens of a light microscope. The asexual parasites density was counted against WBCs counted in microscopic field examination. A patient was considered positive if P. falciparum was seen during the microscopic examination. This procedure was repeated for D1, D2 and D7 follow up of patients.
Lipid Profile Measurements
The method used for the measurement of total cholesterol, triglycerides, high-density lipoprotein and low-density lipoprotein was spectrophotometry using the RANDOX MONACO machine which is automated with a built-in inventory management system. On D0, D3, D7 of follow-up, 2ml of blood was collected from patients via venipuncture and placed in to a 4ml EDTA test tube. Blood samples were centrifuged using a centrifuge at 3000 rpm for 15 minutes as per standard clinical laboratory procedures. The plasma was then separated and transferred into dry tubes and stored in a refrigerator set at 0 to 4oC.The samples were then analyzed using RANDOX MONACO for cholesterol, triglycerides, high-density lipoprotein (HDL), low-density lipoprotein (LDL) Which uses enzymatic colorimetric and spectrophotometric test. Blood analyzed were collected on D0 before treatment and D2 and D7 after treatment.
Data Analysis
Data were entered and analyzed using SPSS software version 21.0 and Microsoft excel 2013. Normality was checked using the Kolmogorov-Sminov (K-S) test. Descriptive statistics were done. An independent t-test was used to show mean differences of lipid parameters parasite density among malaria patients and control groups. Analysis of variance was employed to know mean differences of lipid parameters and parasite density among low, moderate, and high malaria parasitemia grades. P-values <0.05 were considered as statistically significant. Finally, a correlation test was carried to show the relationship between parasite density and lipid profile parameters.
Results
Socio-Demographic Data
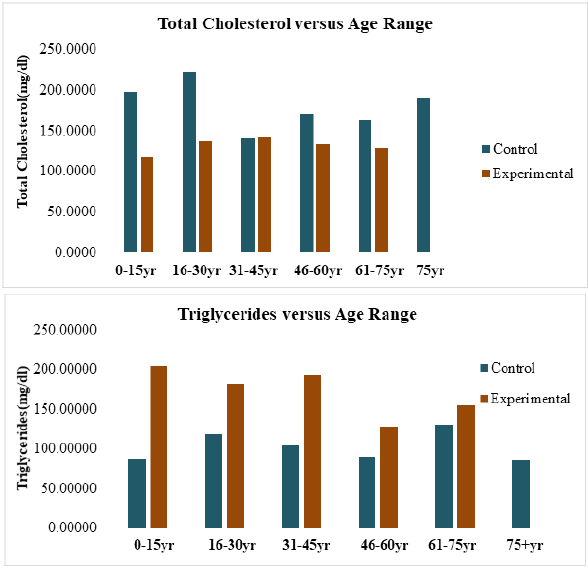
The baseline characteristics of participants (144) who met the inclusion criteria are displayed (Table 1) below. Of the overall, children enrolled had a mean weight of 36.4Kg. There was a significant difference in hemoglobin (Hb g/dL) in study cases and control group (p = 0.04) as well as in their temperatures which recorded a significant difference with p-value of 0.04 between control and test cases (Table 1).
Effect Of Malaria Variation of Total Cholesterol and Triglycerides with Different Age Groups in Control and Experimental Groups
The total cholesterol level distribution among the six age groupings of this study indicated that there was a great decline in mean (SD) total cholesterol in the age group 16-30 years in malaria patients when compared to the controls i.e., from 222.1700(68.04763) mg/dl to 137.0867(49.70639) mg/dl and it was represented by a decline of 85.0833mg/dl. Though total cholesterol showed relative decrease among the different age groups the correlation was not significant (0.124) and (p>0.05) (Figure 1a). An overview of triglycerides level showed that in the age group 0-15years (204.18889(134.098438)), it was generally higher in infected subjects when compared to the uninfected subjects 86.30000(21.071782) leading to an increase of 117.7mg/ dl. This correlation was significant (p<0.05) An increase of 62.5mg/ dl was observed within 16-30 age group, 88.52mg/dl within 31- 45 years and 36.64mg/dl within 61-75 age group when both the mean (SD) of both control and experimental were compared in the different age groups. Although there was this increase in serum concentration of triglycerides in the different age groupings, the correlation between age and the concentration of triglycerides was not statistically significant (p=0.310) (Figure 1b) (Figure 1).
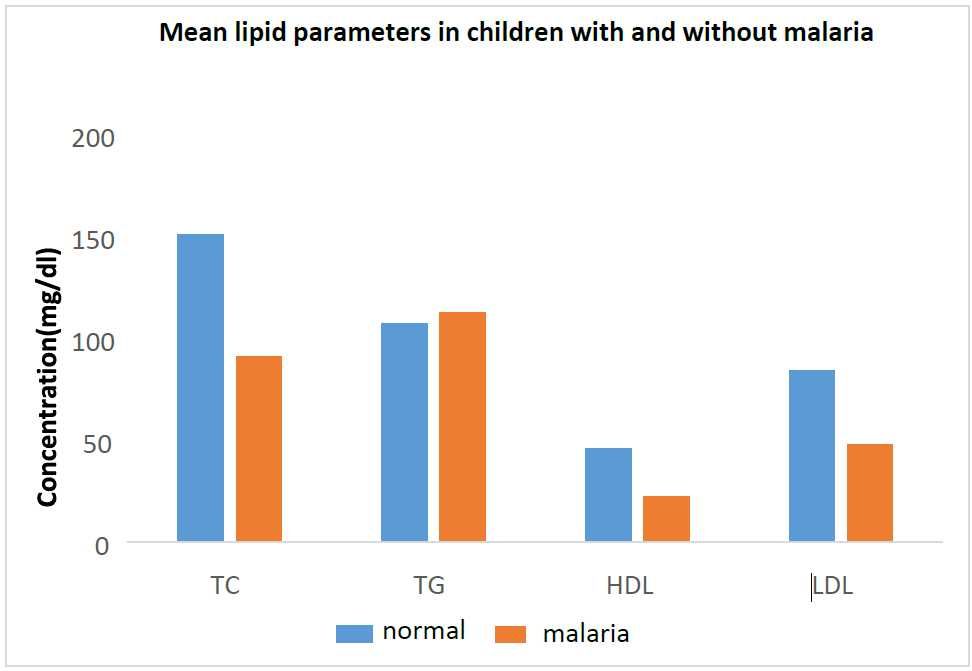
Effect Of Malaria on The Lipid Profile of Children
A comparison of the mean values of lipid parameters in normal children and children infected with malaria caused by P. falciparum was done and the results presented below (Figure 2). There was a decrease in the means of lipids in children suffering from malaria from that of normal individuals not affected by the parasite. Total cholesterol from 150.55mg/dl to 90.82mg/dl with a p-value of 0.0239, TG from 104.25900mg/dl to 106.87mg/dl with a p-value of 0.413, HDL from a mean of 45.53mg/dl to a mean of 22.30mg/dl and a p-value of 0.0306 and LDL from a mean of 83.64667mg/dl to 47.67000mg/dl and with a p-value of 0.0413 (Figure 2).
Comparison of Means of Lipid Profile Parameters in AL And AL + AP After Follow-Up on Day 7
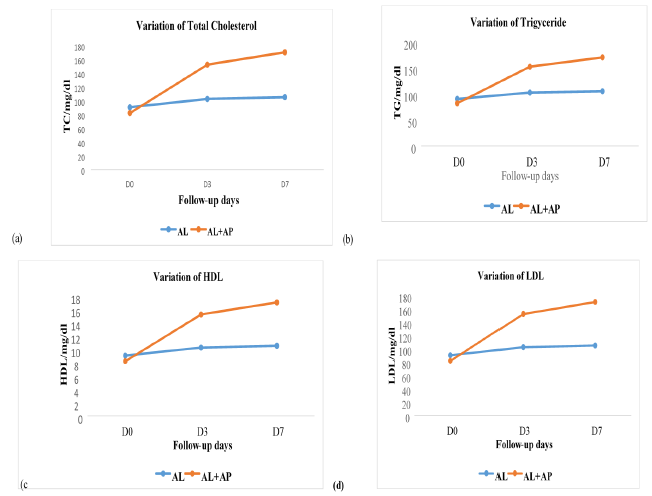
Figure 3: Representation of the changes in lipid profile in different treatment groups: (a) variation of TC, (b): variation of TG, (c): variation of HDL, (d): variation of LDL.
The data represented below shows a continuous increase in the lipid profile TC, HDL, and LDL and a decrease in TG of infected individuals during treatment and after treatment. The graph (Figure 3a) shows an increase in total cholesterol levels from a mean concentration of 82.34mg/dl on D0 to a mean concentration of 170.70mg/dl on D7 in AL+AP treatment group which is much higher than in the AL group which moved from 90.8218mg/dl on D0 to 105.48 on D7 of follow up. The level of triglycerides increased from D0 through D3 to D7 in both groups but with a much more increase in AL+AP group with a mean concentration of 104.618mg/ dl on D0 to 78.897mg/dl on D7 (Figure 3b). The HDL level was lower in AL+AP group on D0 but higher on D3 at 50.95mg/dl and on D7 at 62.22mg/dl (Figure 3c). LDL levels were also seen to increase in AL+AP group as compared to AL group from D0 of recruitment to D7 of follow up with a mean concentration of 44.724mg/dl on D0 and to 92.706mg/dl on D7 in AL+AP treatment group (Figure 3d) (Figure 3).
Effect Of Treatment on The Parasite Density
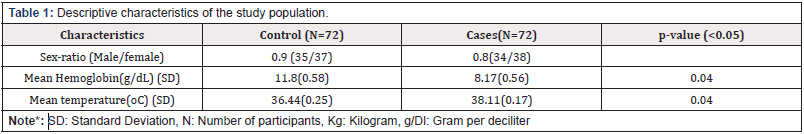
The findings from comparing the mean parasite density in AL and AL + AP group are recorded below (Table 2). The mean of the parasite density of AL group and AL + AP group on the D0 were 23730.00±5.683 and 26920.00±3.993, on D1 it was 17960.00±4.914 and 5700.00±7.168, D2: 90.00±4.914 and 0.00±0.000 and finally on D7: 560.00±5.035 and 0.00±0.000 respectively. The mean difference between AL and AL+AP on the D0 was 3190.000 and with a p-value of 0.825, on D1 the mean difference was 12260.000 with a p value of 0.155, on D2 the mean difference was 90.000 with a p value of 0.0001 and on D7 the mean difference was calculated to be 560.000 and a p value of 0.038 (Table 2).
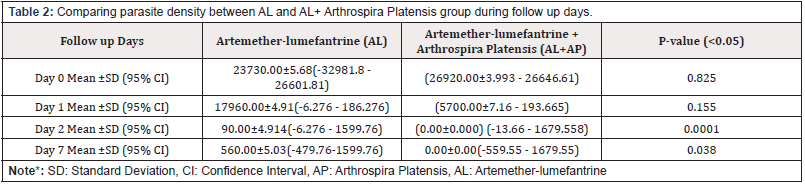
Table 2: Comparing parasite density between AL and AL+ Arthrospira Platensis group during follow up days.
Note*: SD: Standard Deviation, CI: Confidence Interval, AP: Arthrospira Platensis, AL: Artemether-lumefantrine
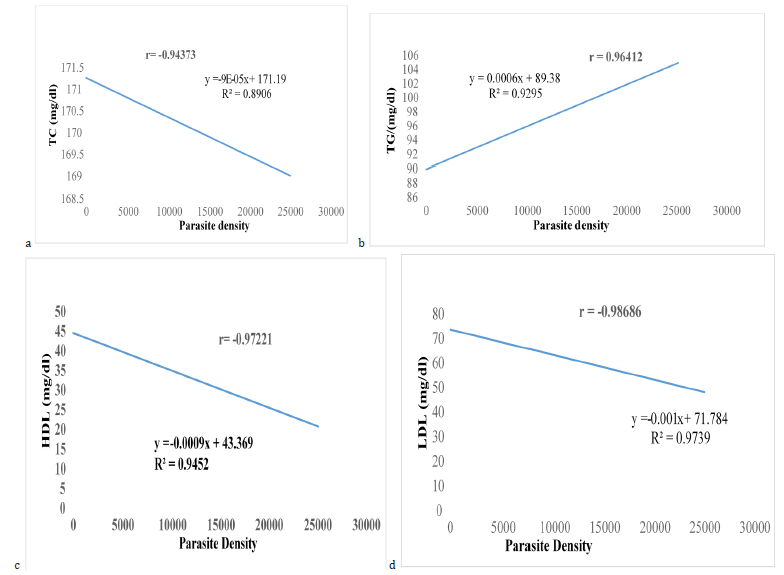
Correlation Between Parasite Density and Lipid Profile Parameters.
The relationship between parasite density and lipid profile parameters; total Cholesterol, Triglycerides, HDL and LDL was derived by carrying out a correlation test. Correlating the mean parasite density with total cholesterol of patients infected with P. falciparum on D0, D3, D7 gave a strong negative correlation value of r = -0.94373 and a p-value of 0.004 indicating that there is a relationship between parasite density and total cholesterol (Figure 4). The parasite density decreased, and total cholesterol increased from D0 to D7. Correlating the mean parasite density with total triglycerides of patients infected with P. falciparum on D0, D3, D7 gave a strong correlation value of r = 0.96412 and p-value of 0.001, indicating that there is a relationship between parasite density and triglycerides (Figure 4). The parasite density decreased, and total triglycerides decreased from D0 to D7. Correlating the mean parasite density with HDL of patients infected with P. falciparum on D0, D3, D7 gave a strong correlation value of r = -0.97221 and p-value of 0.0008 indicating that there is a relationship between parasite density and HDL (Figure 4). The parasite density decreased, and HDL increased from D0 to D7. Mean parasite density with LDL of patients infected with P. falciparum on D0, D3, D7 gave a strong correlation value of r = -0.98686 and p-value of 0.0001 indicating that there is a relationship between parasite density and LDL (Figure 4). The parasite density decreased, and LDL increased from D0 to D7.
Discussion
Malaria is still one of the leading causes of child morbidity and mortality and a public health concern in Cameroon and in other Sub-Saharan Africa and Southeastern Asia countries irrespective of the enhanced management measures put in place with Plasmodium falciparum being the major cause of all deaths [1]. Due to the challenge of parasite resistance to ancient malaria drugs such as chloroquine, mefloquine etc., there has been the development and use of ACTs as recommended drugs of choice for first-line treatment of malaria caused by P. falciparum [21]. However, in these areas highly affected by malaria, the use of these ACTs not only provide beneficial but detrimental effects to the body system and metabolic pathways in children most especially the lipid profile which can lead to the pathogenesis of many other ailments. The proposed strategies to curb the negative effects of malaria parasite infection on the lipid profile in children include the use of conventional drugs, phytotherapy and the exploration of microbes for their antimalaria effect [12].
Lipids play a crucial role in the metabolism of Plasmodium in both phases of its life cycle in the human host [22]. These organisms use cholesterol and phospholipids from the host to their metabolic requirements, such as membrane or haemozoin formation [23]. Additionally, it is likely that the parasite modifies metabolic pathways of lipids in the hepatocytes. Finally, oxidative stress has been associated with oxidation of lipoproteins, contributing to the abnormalities of lipids levels [24]. This study shows that malaria infection altered lipid profile of all age groups. The effect was seen to be more pronounced in the age group 0-15 than in the other age groups. Studies have been conducted supporting the fact that malaria affects lipid profile within this age group [12]. For instance, a previous study with Nigerian children with falciparum malaria has shown a significant decrease of total cholesterol in children when compared to the control group and in contrast to our study for triglycerides [25]. Also, in this study, all participants in group 1 registered a normal cholesterol level compared to the other groups. However, such levels were significantly lowered (p = 0.0239) in children with malaria compared to the healthy control. This is possibly due to the fact that reduction of total cholesterol level is a common finding in patients with malaria and has been associated with metabolic requirements (proteins and lipids, such as cholesterol and lipoproteins) of Plasmodium for their optimal development in hepatocytes leading to impairment of lipid synthesis and the excessive consumption of lipids by the parasites [12]. Due to the nature of hepatocytes, previous study carried out by Labaied, et al. [26], has suggested that lipoproteins are in part exploited by the parasite as sources of cholesterol. This is in line with other studies carried out on Nigerian children with P. falciparum malaria showing a significant decrease in cholesterol rich proteins in complicated cases but contrasting in that, only the LDL fraction was significantly lowered in uncomplicated malaria [25]. Another study in the same country has shown a pattern of lipid changes similar to the pattern of this current study [27]. A study also carried out on changes in lipid composition during sexual development of the malaria parasite Plasmodium falciparum, also supports the findings of this current study [28] as well as Orimadegun, et al. [25] who worked on the evaluation of lipid abnormalities in patients with malaria and other infectious diseases, reporting that cholesterol rich lipoprotein levels, such as LDL and HDL, have also decreased significantly in children with malaria at admission, compared to healthy children. In contrast to HDL and LDL, triglycerides were seen to significantly increase (p = 0.0413) in patients with P. falciparum as compared to normal individuals. This could be due to the fact that triglycerides are released from red blood cells when destroyed by malaria sporozoites. This is in line with previous studies carried out on lipid parameters in a hyperendemic area for malaria [29].
The use of Artemether-lumefantrine as combination therapy has become necessary to meet the challenges of malaria infection and curb the disease but faced its own challenges. Dietary supplements have been used in combination with other drugs for the treatment of many ailments such HIV. It is important to note that while some dietary supplements can adversely interact with prescriptions, some supplements may also have a positive impact on the malaria disease processes. In this present study, we evaluated the possible effect of using AL and Arthrospira platensis in the treatment of P. falciparum malaria and its effect on the lipid profile and parasitemia. Total cholesterol was significantly higher on D7 of control as compared to D0 of recruitment. An increase in cholesterol rich lipoproteins; HDL and LDL and a decrease in triglyceride levels of children treated with AL as compared to that of normal patients wasn’t significant. This showed that even though AL was able to raise the levels of total cholesterol, HDL and LDL in malaria positive children, it did not raise the value up to normal levels. These results gotten, maybe as a result of decrease levels of parasite density from D0 to D7 of treatment. Arthrospira platensis in combination with AL, was seen to have significantly increased the levels of TC, HDL and LDL (p<0.05) and insignificantly decrease the level of TG (p>0.05) when comparison was done with those receiving AL only. These results showed that, Arthrospira plantensis significantly affect the dyslipidemia through the inversion of lipid profile when used together with Al. The presence of antioxidant compounds like phycocyanin, phenolic compounds, and polyunsaturated fatty acids in the microalgae Arthrospira platensis can be the reason for increased serum lipids levels of TC, HDL, and LDL and decrease in triglycerides. In previous study, Arthrospira platensis supplementation decreased the levels of plasma lipid concentration and modified the total cholesterol and HDL cholesterol levels [30]. Although the results in this study showed that Arthrospira plantensis might have caused the surge of lipid serum levels, other factors might also have contributed to these results such as feeding habit by the restoration of appetite that was lost during the severity of the disease. This study also investigated the parasite clearance rate in two treatment groups: those receiving AL and those receiving AL together with Arthrospira plantensis. Results showed a significant decrease in parasite density in both groups receiving treatment from D0 to D7 of follow-up. When paired wise comparison was done between the two groups on D0, D1, D2 and D7 the parasite density was seen to have cleared off more rapidly in the group receiving AL together with Arthrospira platensis plantensis than in the AL group. Also, Arthrospira plantensis played a role in the eradication of parasitaemia in the host’s blood which is as a result of the rich content this cyanobacterium has such as phycocyanin which have been known to be the cause of the antimalarial properties of Arthrospira plantensis.
Conclusion
This study has shown that lipid abnormalities were characterized by decreased levels of total cholesterol, LDL, and HDL and by the increased levels of triglycerides. Arthrospira platensis has a positive effect on the lipid profile of children below 16 years of age infected with P. falciparum and also demonstrates antimalarial properties in cases of positive P. falciparum, improved serum lipid biomarkers levels and rapidly reduced the symptoms of malaria. Therefore, malaria has an effect on the lipid profile parameters and AP plus AL both have a synergistic effect in the treatment of uncomplicated malaria.
Ethical Consideration
Ethical approval was sought and obtained from the Regional of public health Bamenda, Northwest Region Cameroon through N/Ref: 110/ATT/NWR/RDPH/BRICAD of 25th May 2021 and the Ethical and Research committee of the University of Bamenda, Northwest Region Cameroon. A Proxy-informed consent was gotten from all individuals enrolled in the study or from parents and guardians of the children for their willingness to participate in the study after explaining the rational of the study and ensuring their confidentiality. Participation was voluntary
Acknowledgements
The authors appreciate the technical staff of the Bamenda Regional Hospital, Azire Preventive clinic, Gilead Health Center and Vision Laboratory for their support.
Authors’ Contributions
MTN conceptualized and designed the study, monitored data collection for the whole trial, analyzed the data, wrote the first draft of the manuscript, and revised the paper. CMM conceptualized and designed the study, interpretation of data and revised the paper. A B-A J managed the collection of data, the statistical analysis, and interpretation of data and revised the paper. JT and NBB managed the study protocols, acquisition of data, statistical analysis and revised the paper. BB managed the literature searches, data collection and revised the paper. All authors read and approved the final manuscript.
Funding
This study is a part of research modernization by the Ministry of Higher education of Cameroon. The sponsors are not involved in the manuscript writing editing approval or decision to publish.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
References
- T N Metoh, JH Chen, P Fon Gah, X Zhou, R Moyou Somo, et al. (2020) Genetic diversity of Plasmodium falciparum and genetic profile in children affected by uncomplicated malaria in Cameroon. Malar J 19(1): 115.
- (2021) World Health Organization, World malaria report 2020: 20 years of global progress and challenges. World Health Organization, 2020.
- The Early Years: Birth of The National Malaria Control Programme.
- A Talipouo, Carmene S Ngadjeu, Patricia Doumbe Belisse, Landre Djamouko Djonkam, Nadege Sonhafouo Chiana, et al. (2019) Malaria prevention in the city of Yaoundé: knowledge and practices of urban dwellers. Malar J 18(1): 167.
- K Plewes, S J Leopold, HWF Kingston, AM Dondorp (2019) Malaria: What’s New in the Management of Malaria?. Infect Dis Clin North Am 33(1): 39-60.
- C Antonio Nkondjio, N Sonhafouo Chiana, C S Ngadjeu, P Doumbe Belisse, A Talipouo, et al. (2017) Review of the evolution of insecticide resistance in main malaria vectors in Cameroon from 1990 to 2017. Parasit Vectors 10(1): 472.
- AM Dondorp, François Nosten, Poravuth Yi, Debashish Das, Aung Phae Phyo, et al. (2009) Artemisinin Resistance in Plasmodium falciparum Malaria. N Engl J Med 361(5): 455-467.
- World Health Organization, World malaria report 2015. Geneva: World Health Organization.
- A Derbie, D Mekonnen, M Adugna, B Yeshitela, Y Woldeamanuel, et al. (2020) Therapeutic Efficacy of Artemether-Lumefantrine (Coartem®) for the Treatment of Uncomplicated Falciparum Malaria in Africa: A Systematic Review. J Parasitol Res 2020: 7371681.
- JK Baird (2013) Evidence and implications of mortality associated with acute Plasmodium vivax malaria. Clin Microbiol Rev 26(1): 36-57.
- M Theresia Njuabe, SM Roger, F Philip Gah, T Ernest, C Jun Hu, et al. (2021) Efficacy and Safety Assessment of Three Artemisinin-Based Combination Therapy (Acts) in the Treatment of P. falciparum Malaria in Cameroon. J Infect Dis Epidemiol 7(12): 242.
- R M Dias, Jose Luiz Fernandes Vieira, Bianca da Conceição Cabral, Isameriliam Rosaulem Pereira da Silva, Laelia Maria Barra Feio Brasil, et al. (2016) Lipid Profile of Children with Malaria by Plasmodium vivax. J Trop Med 2016: 9052612.
- S Shekalaghe, Dominic Mosha, Ali Hamad, Thabit A Mbaga, Michael Mihayo, et al. (2020) Optimal timing of primaquine to reduce Plasmodium falciparum gametocyte carriage when co-administered with artemether-lumefantrine. Malaria Journal 19(1): 34.
- P D Karkos, SC Leong, CD Karkos, N Sivaji, D A P Assimakopoulos (2008) Spirulina in Clinical Practice: Evidence-Based Human Applications. Evid Based Complement Alternat Med 2011: 531053.
- A Finamore, M Palmery, S Bensehaila, I Peluso (2017) Antioxidant, Immunomodulating, and Microbial-Modulating Activities of the Sustainable and Ecofriendly Spirulina. Oxid Med Cell Longev 2017: 3247528.
- T N Metoh, R K A Siberedi, C A Pieme (2022) Evaluating the Effects of Spirulina (Arthrospira platensis) on Artemether/Lumefantrine (Coartem)-Induced Oxidative Stress in Wistar Rats. International Journal of Tropical Medicine 17(1): 1-9.
- A S Neba (1987) Modern Geography of the Republic of Cameroon, Subsequent edition. Camden NJ.
- AchoChi (1998) Human interference and environmental instability: addressing the environmental consequences of rapid urban growth in Bamenda, Cameroon. Environment and Urbanization 10(2): 1998.
- M E NgoMatip, Constant Anatole Pieme, Marcel Azabji Kenfack, Bruno Moukette Moukette, Emmanuel Korosky, et al. (2015) Impact of daily supplementation of Spirulina platensis on the immune system of naïve HIV-1 patients in Cameroon: a 12-months single blind, randomized, multicenter trial. Nutr J 14(70).
- L B Ochola, P Vounatsou, T Smith, M L H Mabaso, C R J C Newton (2006) The reliability of diagnostic techniques in the diagnosis and management of malaria in the absence of a gold standard. Lancet Infect Dis 6(9): 582-588.
- J Naß, T Efferth (2019) Development of artemisinin resistance in malaria therapy. Pharmacol Res 146: 104275.
- K C Gondim, G C Atella, E G Pontes, D Majerowicz (2018) Lipid metabolism in insect disease vectors. Insect Biochem Mol Biol 101: 108-123.
- B J Visser, R W Wieten, I M Nagel, M P Grobusch (2013) Serum lipids and lipoproteins in malaria - a systematic review and meta-analysis. Malar J 12: 442.
- S Jun, S Datta, L Wang, R Pegany, M Cano, et al. (2019) The Impact of Lipids, Lipid Oxidation, and Inflammation on AMD, and the Potential Role of miRNAs on Lipid Metabolism in the RPE. Exp Eye Res 181: 346-355.
- A E Orimadegun, B E Orimadegun (1025) Serum Apolipoprotein-A1 and Cholesterol Levels in Nigerian Children with Plasmodium falciparum Infection. Med Princ Pract 24(4): 318-324.
- M Labaied, Bamini Jayabalasingham, Nazneen Bano, Sung Jae Cha, Juan Sandoval, et al. (201) Plasmodium salvages cholesterol internalized by LDL and synthesized de novo in the liver. Cellular Microbiology 13(4): 569-586.
- S Ogbodo, O Ogah, H Obu, E Shu, C Afiukwa (2008) Lipid and lipoprotein levels in children with malaria parasitaemia. Current Paediatric Research 12: 13-17
- PN Tran, SH J Brown, M Rug, M C Ridgway, T W Mitchell, et al. (2016) Changes in lipid composition during sexual development of the malaria parasite Plasmodium falciparum. Malar J 15: 73.
- F A Neves, A M Ventura, M G Filho, R M Libonati (2013) Lipid parameters in a hyperendemic area for malaria. Lipids in Health and Disease 12: 162.
- L M Colla, A L Muccillo Baisch, J A V Costa (2008) Spirulina platensis effects on the levels of total cholesterol, HDL and triacylglycerols in rabbits fed with a hypercholesterolemic diet. Braz arch biol Technol 51(2): 405-411.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.