Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Bilateral Covid-19 Pneumonia and Obesity: A Case Report of an Elderly Woman at High Resolution Computed Tomography
*Corresponding author: Francesco Messina, MD at Radiology Unit of Riuniti Hospital, Azienda Ospedaliera Grande Ospedale Metropolitano (G.O.M.), “Bianchi-Melacrino-Morelli” Reggio Calabria, Italy
Received: January 06, 2022; Published: January 21, 2022
DOI: 10.34297/AJBSR.2022.15.002106
Abstract
The Covid-19 Coronavirus infectious pandemic started since December 2019. From the first reported cases in Wuhan in this date, the disease has spread so rapidly over the world that it was declared a pandemic by the World Health Organization in March 2020. It caused mainly bilateral interstitial pneumonia in the patients. The heterogeneity of the course and clinical frameworks of the disease represents an important problem both for the acute phase and for the possible complications. Many typical imaging features of this disease were described. Now, we describe a case of an elderly Italian woman with obesity that had Covid-19 pneumonia, bilaterally, documented at Computed Tomography.
Keywords: Covid-19; Pneumonia; Obesity; High Resolution Computed Tomography (HRCT); Chest
Case Presentation
A 77-years-old woman with hypertension and diabetes mellitus was admitted to the emergency department after 5 days with persistent chest pain, shortness of breath, sore throat and fever (38°C). She had done only the first dose of the vaccine against Covid-19 pneumonia, and she recently had a contact with a people positive at Covid-19.
At emergency department the patient:
a. had fever (temperature 39°C).
b. hypertensive (blood pressure 170/90 mmHg) and tachycardic
(heart rate 106 beats for minute).
c. MV was significantly reduced bilaterally at auscultation of
thorax.
d. arterial oxygen saturation (SaO2) was 89%.
e. laboratory: leukopenia (3.4 G/L); increased values of C-reactive
protein (260 mg/L), LDH, and procalcitonin.
She was an obese patient (body weight 110 kilograms [kg], height 1.6 metres [m], body mass index (BMI) 40.40). Oropharyngeal swab was positive for SARS-CoV-2 by real-time polymerase chain reaction (RT-PCR). A chest CT scan was urgently performed, in basal conditions and high-resolution algorithm (HRCT), with a 64-slices multidetector scanner, and the images so obtained were analyzed with a slice-thickness of 1.2 mm and MPR reconstructions (axial, sagittal, and coronal). HRCT had documented (Figure 1a, b) in both lungs the presence of multiple thickenings with a “ground glass” pattern, and some areas of interstitial consolidations and thickenings. In the mediastinum there were some small, reactive, lymphnodes. There was also the presence of a minimal pleural effusion, on the right. CT had also showed the signs of obesity, such as the increase in adipose tissue and fat mass in different areas, bilaterally, with great precision.
In consideration of the worsening of the clinical conditions, the patient was immediately hospitalized, and a multi-drugs therapy with also high-flow O2 was immediately begun. On the sixth hospitalization day the patient had a modest, but progressive, improvement. The duration of hospital stay was twenty-five days.
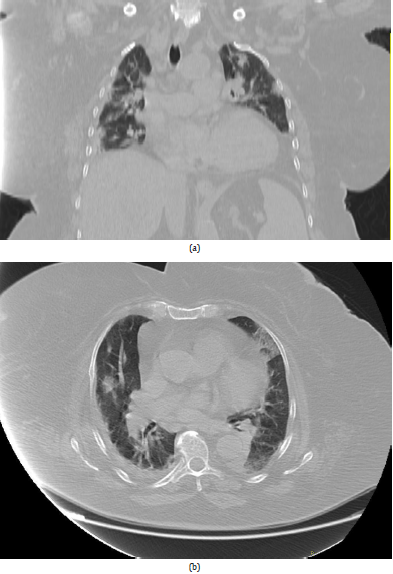
Figure 1a,b: Chest High Resolution Computed Tomography (HRCT); (a) coronal MPR reconstruction; (b) axial MPR reconstruction. HRCT had identified in both lungs the presence of multiple thickenings with a “ground glass” pattern, and some areas of interstitial consolidations and thickenings. Presence of a minimal pleural effusion, on the right. HRCT had also showed the signs of obesity, such as the increase in adipose tissue and fat mass in the context of the adipose and muscular planes adjacent to the lateral thoracic wall, bilaterally.
Discussion
Covid-19 pneumonia is a disease with different outcomes within the population: with increasing of the age the prognosis becomes worse. Age was immediately identified as a “risk factor” and over the months it was realized that other conditions can worsen the course of Covid-19 pneumonia. A condition that significantly worsens the prognosis is obesity. Obesity is often accompanied by other comorbidities: arterial hypertension, diabetes mellitus, hypercholesterolemia, other cardiovascular diseases, and chronic respiratory diseases [1]. Obesity was an important risk factor for the hospitalization and death during the 2009 H1N1 influenza pandemic [2]. Similarly, now, obesity is an increasingly recognized risk factor for severe Covid-19 and death; it’s the second most common risk factor among the patients hospitalized with Covid-19 pneumonia [3]. In fact, there are several possible reasons for the correlation between obesity and Covid-19. Physical inactivity, common in obesity, may lead to impaired immune response. The altered dynamics of pulmonary ventilation with reduced diaphragmatic excursion and a relative increase in anatomical dead space may account for the increased incidence of severe Covid-19 in patients with obesity.
It is known that the most serious effects of Covid-19 derive from a sort of over-reaction of our immune system which, failing to manage the infection, causes an enormous immune and inflammatory response which in some cases leads to the death of the patients. Obese patients are subject to a mild persistent systemic inflammation which often remains silent for years, but which in case of stimulation can worsen in a short time. We can hypothesize that this mild state of systemic inflammation that characterizes obese subjects could result in a particularly violent autoimmune reaction in case of Sars-CoV2 infection. It is as if a lot of flammable material accumulates inside obese subjects and the Sars-CoV2 infection represents an open flame that triggers a very violent “immunitary-fire”. The presence of a pro-inflammatory state in obesity may impair immune response and pulmonary function [4-5]. The leptin had a particular interestis and is involved in weight regulation by decreasing energy intake and increasing energy expenditure, as well as modulation of the innate and adaptive immune function through activation of neutrophils, macrophages, and T lymphocytes. It was proposed that leptin was a co-factor for the 2009 H1N1 pandemic and had an interesting observation for the association of obesity with lower Vitamin D serum levels. As vitamin D reduces the risk of viral infections through enhancing both innate and adaptive immunity, this might contribute to increased risk of Covid-19 in people with obesity. And vitamin D also modulates the expression of angiotensin converting enzyme 2 (ACE-2), which is the putative co-receptor for cellular SARSCoV-2 entry. Increased adipose tissue in obesity could lead to increased ACE-2 expression and risk of infection. Obesity leads to poorer vaccination success and emergence of more virulent virus strains, due to blunted cytokine and interferon production. In addition, people with obesity carry more infectious virus in exhaled breath due to higher ventilation volumes [6-8].
The level of neutralizing anti-Spike IgG antibodies was studied, which are the antibodies that our system produces to neutralize Sars-CoV2; they are used as an indicator of an adequate response to infection. Obese patients have a very low amount of neutralizing antibodies compared to normal weight patients. This observation could explain why obese patients have a worse prognosis. Furthermore, obese and Covid-19 patients, in addition to having few neutralizing antibodies, also have autoantibodies that can contribute to the severity of the disease [9-10].
High Resolution Computed Tomography (HRCT) of the thorax is useful in early diagnosis of Covid-19 infection, in monitoring disease progression, coinfection, or disease stability. Computed Tomography had the possibility to evaluate accurately the type and extent of lung lesions. In our experience, we found that the most common CT findings were: GGO, consolidations, crazy-paving patterns, and pleural effusion. Consolidation was significantly more frequent in severe/critical patients, which indicates that the alveoli are completely filled by inflammatory exudation; this usually means that the virus diffuses into the respiratory epithelium, leading to necrotizing bronchitis and diffused alveolar damage [11-12].
Conclusions
The patients with obesity are more at risk of developing a severe form of Covid-19 pneumonia. Obesity often manifests itself with other pathologies and cardiovascular risk factors, such as arterial hypertension, diabetes mellitus and hypercholesterolemia, that are also risk factors for Covid19-pneumonia. Obesity had an important role in virus transmission because adipose tissue may become a reservoir for SARS-CoV-2. Computed Tomography findings of consolidations, linear opacities, bronchial wall thickenings, and other signs, may be features of severe/critical Covid-19 pneumonia. Computed Tomography had an important role for the diagnosis and evaluation of the severity of this disease, also in the patients with obesity, because it investigates very well the dynamic CT changes in different stages of Covid-19 pneumonia, and also for the follow-up and the best outcome/management of the patients.
Conflicts of interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Patient Consent Statement Mandatory
The patient confirmed the consense for publication of our case report.
References
- Fei Zhou, Ting Yu, Ronghui Du, Guohui Fan, Ying Liu, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (Lond Engl) 395: 1054-62.
- Oliver W Morgan, Anna Bramley, Ashley Fowlkes, David S Freedman, Thomas H Taylor, et al. (2010) Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease. PLoS One 5(3): e9694.
- Arthur Simonnet, Mikael Chetboun, Julien Poissy, Violeta Raverdy, Jerome Noulette, et al. (2020) High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring) 28(7): 1195-1199.
- Livio Luzi, Maria Grazia Radaelli (2020) Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol 57: 759-64.
- Peter Mancuso (2013) Obesity and respiratory infections: does excess adiposity weigh down host defense? Pulm Pharmacol Ther 26: 412-419.
- Jennifer S Walsh, Simon Bowles, Amy L Evans (2017) Vitamin D in obesity. Curr Opin Endocrinol Diabetes Obes 24: 389-394.
- William B Grant, Henry Lahore, Sharon L Mcdonnell, Carole A Baggerly, Christine B French, et al. (2020) Evidence that vitamin d supplementation could reduce risk of influenza and Covid-19 infections and deaths. Nutrients 12(4): 988.
- Stephen J Carter, Marissa N Baranauskas, Alyce D Fly (2020) Considerations for obesity, vitamin D, and physical activity amidst the Covid-19 pandemic. Obesity (Silver Spring) 28(7): 1176-1177.
- Radwan Kassir (2020) Risk of Covid-19 for patients with obesity. Obes Rev 21(6): e13034.
- R Huttunen, J Syrjänen (2013) Obesity and the risk and outcome of infection. Int J Obes 2005 37(3): 333-340.
- Muhammad Umer Nasir, James Roberts, Nestor L Muller, Francesco Macri, Mohammed F Mohammed, et al. (2020) The role of emergency radiology in Covid-19: from preparedness to diagnosis. Can Assoc Radiol J 71(3): 293-300.
- Koo HJ, Lim S, Choe J, et al. (2018) Radiographic and CT features of viral pneumonia. Radiographics 38: 719-739.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.