Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Case Report: The treatment progress of a typical case of COVID-19 in WUHAN
*Corresponding author: Douglass Hanly Moir Pathology 14 Giffnock Avenue Macquarie Park 2113 NSW, Australia.
Received: February 02, 2022; Published: February 15, 2022
DOI: 10.34297/AJBSR.2022.15.002122
Abstract
The patients are typical patients with moderate to severe new coronary pneumonia. The treatment group formulates and adjusts the treatment plan for patients during their stay in the ICU according to the province’s 8-point treatment consensus [1] on COVID-19 pneumonia and clarifies the patient’s medication and nutritional support at different stages. The summary of the experience is significant for guiding future treatment and rescue of patients.
Introduction
The patient was a nurse in our hospital’s isolation ward who went to see a doctor for “repeated fever for 4 days”. Before the positive result from the nucleic acid test, the imaging changes from her lung CT were used to diagnose the new coronary pneumonia and to admit the patient to the hospital for treatment. However, her condition gradually worsened, her vital signs and nutritional status were repeatedly uncertain, and she entered a critical state at one time.
Case
Patient Description
Patient: Miss A, female, 25 years old, height 167 cm, weight 67 kg, BMI 24, unmarried;
Main complaint: 2020-02-07 admitted to hospital for “recurrent fever for 4 days”;
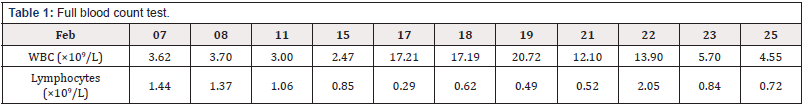
History of present illness: 4 days before admission, the patient developed fever without obvious stimulus and her body temperature reached as high as 38.5℃. She experienced sputum, tightness in the chest, shortness of breath, and no cough, anorexia, nausea, vomiting, or diarrhea. The patient went to the outpatient clinic of our hospital on 2020-02-07. The lung CT showed infectious lung lesions. The blood test showed: white blood cells: 3.62×109/L, neutrophils 1.70×109/L, lymphocytes 1.44×109/L, CRP 0.58 mg/L; the outpatient department was admitted to the hospital with possible “COVID-19 pneumonia”.
The patient’s spirit, appetite, sleep, urination and defecation have been acceptable since the onset of this disease.
No special medical history.
The patient has no long-term residence history in the Wuhan epidemic area and was originally a nurse in the isolation ward of our hospital.
Admission physical examination: T 37.8℃, P 86 bpm, R 20 times/min, BP 120/86 mmHg, SPO2 98%. Consciousness, physical examination and cooperation. The patient has mild fatigue, no obvious yellow staining of the skin and sclera, no cyanosis of the lips, soft neck, heart rate 86 beats/min, flat and soft abdomen, no tenderness and rebound pain, under the ribs of the liver and spleen, and no percussion pain in the kidneys. There is no edema in both lower limbs, and the double Pap sign is negative (Figure1).
Auxiliary examination: white blood cells: 3.62×109/L, neutrophils 1.70×109/L, lymphocytes 1.44×109/L, CRP 0.58 mg/L.
Results of Pathological Tests and other Investigations
The new type of coronavirus has been included in the Class B infectious diseases stipulated in the “Law of the People’s Republic of China on the Prevention and Control of Infectious Diseases”, but in accordance with the prevention and control measures for Class A infectious diseases. Therefore, all the following processes of specimen collection, testing, packaging and transportation, and waste destruction of the new coronavirus are carried out in accordance with national regulations for biosafety protection [2,3].
Diagnose Based On
Patient History: Had a history of exposure to patients with new coronary pneumonia at work.
2020.02.10: Compared to the previous CT scan, the lesion in the lower lobe of the left lung was enlarged. A new ground-glass lesion appeared in the upper lingual segment of the left upper lobe (Figure2-5).
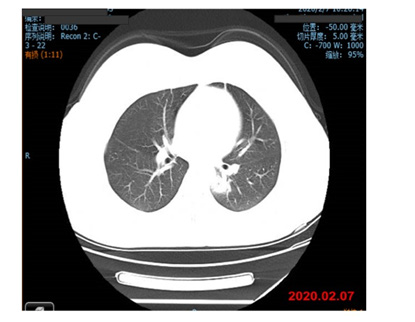
Figure 2: 2020.02.07 Lung CT showed infectious lung lesions and multiple ground-glass lesions in both lungs.
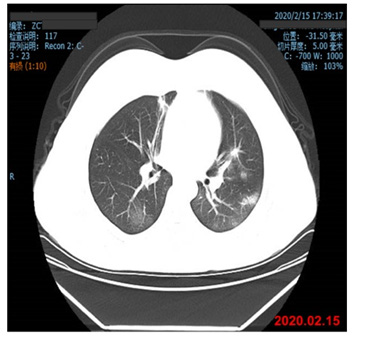
Figure 3A: 2020.02.15 Compared to the previous CT scan: the lesions in the dorsal and posterior basal segments of the left lower lobe were significantly absorbed, and the lesions in the outer basal segment of the left lower lobe and the upper tongue of the left upper lobe were significantly larger. A new ground-glass lesion appeared in the basal segment of the lower lobe of the lung.
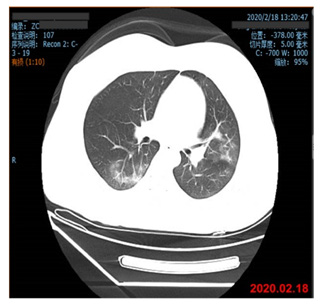
Figure 3B: 2020.02.18 Multiple infectious lesions in both lungs. Compared to the previous CT scan: the lesions in the dorsal segment of the left and right lower lobe increased and the density increased. Among them, the outer basal segment of the left lower lobe consolidated within the lesion, and the upper right lung. New lesions appeared in the anterior and posterior basal regions.
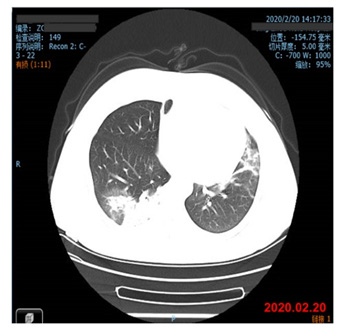
Figure 4: 2020.02.20 Multiple lesions occurred in both lungs, and the area of the front film was enlarged compared to the previous film, and it became dominant with a little fibrosis.
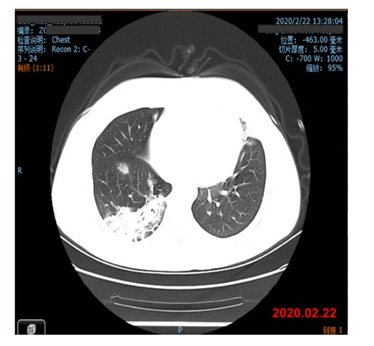
Figure 5: 2020.02.22 There were multiple lesions in both lungs, and the area of the front film was enlarged compared to the previous film, and it became dominant with a little fibrosis; the right middle lobe and there were ground-glass shadows in the posterior basal segment of the left lower lobe, which were new lesions.
Arterial Blood Gas Analysis
2020.02.21: PH 7.38, PO2: 97 mmHg, PCO2: 40.1, SO2: 97.4.
2020.02.22: PH 7.52, PO2: 103 mmHg, PCO2: 30.2, SO2: 98.6.
2020.02.23: BPH 7.39, PO2: 68 mmHg, PCO2: 40, SO2: 93.
COVID-19 Nucleic Acid Test
2020.02.08: Throat Swab (Negative)
2020.02.10: Throat Swab (Negative)
2020.02.12: Throat Swab (Negative)
2020.02.17: Throat Swab (Negative)
2020.02.17: Blood Serum (Negative)
2020.02.19: Blood Serum (Suspected)
2020.02.20: Blood Serum (Positive)
Treatment Plan
2020.02.07-2020.02.16: Treatment plan start from admission day
Arbidol 0.2 g/tid (anti-coronavirus drug)
Ribavirin 0.5 g/bid (anti-coronavirus drug)
Moxifloxacin 0.4 g/qd (anti-secondary infection medication)
Ambroxol 60 mg/bid (anti-hypoxemia medication)
Continuous low-flow oxygen inhalation through nasal cannula: flow rate 5 L/min.
Expected Outcome of this Treatment Plan
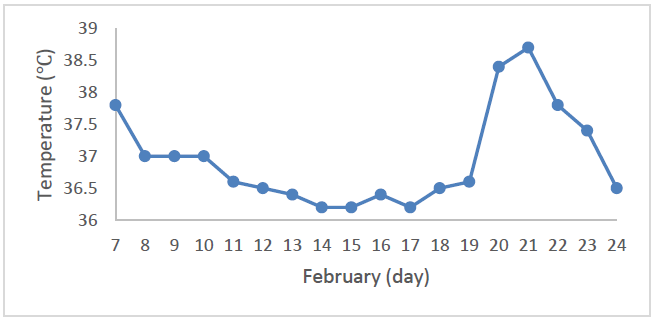
According to the patient’s symptoms, signs and laboratory examinations at the time of admission, the initial consideration is pulmonary infection, with the possibility of COVID-19. Therefore, the treatment plan at this stage is focused on completing various examinations as soon as possible and routine anti-infection (Table1-2).
Actual Outcome
The patient’s body temperature has dropped. Although the patient’s COVID-19 nucleic acid test result is still negative, the examination via lung CT showed that the lesion is progressing rapidly: “The lesion in the lower lobe of the left lung was enlarged, and a ground-glass sample was added to the upper tongue of the upper lobe of the left lung.
2020.02.16-2020.02.18: Adjusted the treatment plan on February 16th:
Methylprednisolone 20 mg/q12h
Lubinavir 1 tablet/qd
Intravenous injection of gamma globulin 10 g/qd
Ambroxol 75 mg/bid
Thymus Faxin 1.6 mg/bid
Continuous low-flow oxygen inhalation through nasal cannula: flow rate 5 L/min.
Expected Outcome of this Treatment Plan
According to the treatment guidelines for COVID-19 [1], glucocorticoids can be used in a short period of time (3 to 5 days) as appropriate for patients with progressive deterioration of oxygenation indicators, rapid imaging progress, and excessive activation of the body’s inflammatory response. Therefore, the treatment plan must be adjusted, and the use of glucocorticoids, intravenous gamma globulin, and the immunomodulatory drug ‘Thymus Faxin’ must be increased [4].
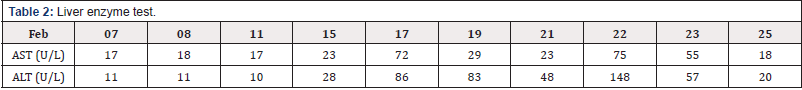
Actual Outcome
Two days after the use of glucocorticoids and immunomodulatory drugs, the white blood cell count increased, the liver function suggested cell damage, the lung imaging showed rapid progression of lesions and the appearance of new unidentified lesions [4-9]. According to changes in the condition and the current drug use plan, glucocorticoids may be the primary cause [5, 6].
2020.02.18-2020.02.20: Adjust the treatment plan on February 18:
Hydroxychloroquine 0.2 g/bid
Cefotaxime sulba 2.25 g/bid
Ambroxol 75 mg/bid
Thymus Faxin 1.6 mg/bid
Continuous low-flow oxygen inhalation through nasal cannula: flow rate 5 L/min.
Expected Outcome of this Treatment Plan
Glucocorticoids were temporarily stopped. Hydroxychloroquine, an anti-coronavirus drug, and cefotaxime sulla, an anti-secondary infection drug, were added, and the lung imaging changes and COVID-19 blood nucleic acid testing results were monitored [1,4].
Actual Outcome
Multiple lesions continued to appear in both lungs. Compared to the previous CT results, the extent of the lesions increased and became dominant with a little fibrosis, suggesting poor control of lung infection. At the same time, COVID-19 pneumonia was initially diagnosed by the nucleic acid test. At present, the patient is beginning to experience a drop in blood oxygen partial pressure, shortness of breath, and mild breathing difficulties.
2020.02.20-2020.02.23: Adjust the treatment plan on February 20:
Hydroxychloroquine 0.2 g/bid
Azithromycin tablets 0.5g/qd
Thymus Faxin 1.6 mg/qd
Methylprednisolone 20 mg/q12h
Liver protection drugs
Intermittent high flow oxygen supply: flow rate 40 L/min, concentration 30%.
Expected Outcome of this Treatment Plan
Glucocorticoids and immunomodulatory drugs were used for two days and then added to the treatment plan. Meanwhile, as liver function tests indicated liver cell damage, drugs to protect liver cells were added [4]. According to the patient’s current situation, we adjusted the oxygen concentration from continuous low-flow oxygen inhalation to intermittent high-flow oxygen inhalation. We also asked the doctor on duty to make dynamic adjustments based on the patient’s terminal blood oxygen concentration monitoring and arterial blood gas analysis [7,8].
Actual Outcome
The patient’s liver cell damage has been relieved, and the lung infection has been controlled.
2020.02.23-2020.02.25: Adjust the treatment plan on February 23:
Hydroxychloroquine 0. 2g/bid
Azithromycin tablets 0.5 g/qd
Thymus Faxin 1.6 mg/qd
Methylprednisolone 40 mg + 20 mg
Ambroxol 150 mg/q12h
Xuebijing 50 mg/q12h
Enteral nutrition
Liver protection drugs
Intermittent high flow oxygen supply: flow rate 40 L/min, concentration 30%.
Expected Uutcome of this Treatment Plan
To maintain the original treatment plan with the addition of enteral nutrition, due to the patient’s difficulty eating. Attention was paid to the balance of intake and output [1,4].
Actual Outcome
The current treatment regimen was maintained, and Methylprednisolone temporarily discontinued. The patient’s condition further eased and she was transferred to the general isolation ward two days later.
Discussion
The patient is a nurse in the infectious disease isolation ward of our hospital and has a history of exposure to patients with COVID-19 pneumonia at work. Therefore, based on the CT results in the early stage of the patient’s symptoms, it was considered to be COVID-19 pneumonia and the patient was promptly isolated and treated as such, even if the nucleic acid test failed to find an abnormality.
Yang et al. analyzed 4021 cases of COVID-19 pneumonia diagnosed nationwide and found that the proportions of light, normal, and severe patients were 4.5%, 69.9%, and 25.5%, respectively [9]. The patient’s condition is progressing smoothly, and it is the common COVID-19 pneumonia that accounts for the largest proportion of the total number of patients. Therefore, the diagnosis and treatment process of this case is of great significance for the verification of the diagnosis and treatment consensus of experts in our province.
There are 8 points in our province’s expert consensus on the treatment of COVID-19 pneumonia. Simply put, the treatment guidance plan for COVID-19 pneumonia is 4 “Anti-” and 4 “maintain-” [1].
The specific treatment guidance plan is as follows:
1. Anti-New Coronavirus Drugs;
2. Anti-secondary infection medication;
3. Anti-hypoxemia medication;
4. Anti-septic shock medication;
5. Medication to maintain nutritional balance;
6. Medications to maintain the water-electrolyte acid-base balance;
7. Medications for maintaining micro-ecological balance;
8. Medication to maintain the balance of tissue and organ function.
The COVID-19 treatment consensus does not recommend the simultaneous application of 3 or more antiviral drugs and emphasizes that the use of related drugs should be stopped when intolerable side effects occur; therefore, we used Arbidol in the first medication after the patient was admitted to the hospital on February 7 and two antiviral drugs, Ribavirin and Moxifloxacin, were used to treat expected secondary infections [1].
According to the reminder by the consensus, patients with severe COVID-19 pneumonia will have severe alveolar inflammatory exudation and a large amount of mucus. Therefore, expectorant drugs such as ambroxol, bromhexine, and related measures should be used as soon as possible. According to the patient’s current condition, ambroxol was selected for treatment [10,11]. The efficacy of the currently tried drugs was monitored and evaluated based on the current treatment plan.
In the next few days, although the patient’s oxygenation indicators did not experience progressive deterioration, the imaging studies showed that the disease was progressing rapidly and that the body’s inflammatory response was over-activated. According to consensus [1], glucocorticoids can be used within a short period of time of three to five days as appropriate [12]. Therefore, the treatment group adjusted the treatment plan, increased the use of glucocorticoids, intravenous injection of gamma globulin, and the immunomodulatory drug ‘Thymus Faxin’ [1,13].
After using glucocorticoids and immunomodulatory drugs for two days, the total number of white blood cells and the proportion of neutrophils increased. This, combined with the changes in lung imaging, suggested a stress response or bacterial infection. At the same time, liver function tests indicated liver cell damage. After consultation, the treatment group temporarily stopped glucocorticoids, added the new anti-coronavirus drug hydroxychloroquine and the anti-secondary infection drug cefotaxime sulba, and continued to monitor lung imaging changes [1,14].
However, the treatment plan above did not improve the status of the patient, who began to experience mild breathing difficulties, decreased blood oxygen pressure, and shortness of breath. In addition, multiple lesions continued to appear in both lungs. A comparison with the previous CT scans showed that the extent of the lesions was enlarged and became the main one with a little fibrosis, suggesting poor control of lung infection. At the same time, COVID-19 pneumonia was initially diagnosed by the nucleic acid test,. This process of treatment has verified the therapeutic effect of hydroxychloroquine on new coronary pneumonia, proving that at least the early and mid-term treatment effect is not good. But at the same time, it should be recognized that there are related reports that hydroxychloroquine has a good therapeutic and preventive effect on new coronary pneumonia [15,16,17].
According to the patient’s current status, the treatment team has formulated four keynotes for the patient’s treatment: 1. Strengthen infection control; 2. Adjust immunotherapy medication; 3. Adjust and strengthen the patient’s nutritional support; 4. Protect liver tissue and liver function.
Therefore, after adjusting antibiotics, add glucocorticoids and immunomodulatory drugs again, adjust liver protection drugs, use nutritional support including for gastrointestinal nutrition, and use enteral nutrition preparations rich in omega-3 fatty acids to prevent systemic immune function decline caused by poor nutrition supply [18,19].
After modifying the treatment plan, the patient’s blood oxygen partial pressure and respiratory symptoms were significantly improved by the evening of the same day. Three days later, glucocorticoids were stopped again, but the other treatment options, especially nutritional support, and the patient was encouraged to take oral nutritional intake. Two days later, the patient was transferred to the general isolation ward.
Conclusion
Our province’s 8-point treatment consensus on COVID-19 pneumonia has an important guiding significance for our treatment and rescue of patients. The essential formulation and adjustment of our treatment plan are carried out in accordance with the consensus of “anti-” plus 4 “maintain-” [1]. During the treatment process, the treatment group also summarized some of their treatment experiences for typical moderate and severe patients.
Firstly, the question of testing. Nucleic acid testing is of course a gold indicator, but the testing process of this patient shows that even blood and throat swab tests are negative at an early stage, and that a positive result does not appear until nearly 14 days later. Therefore, lung imaging results, especially CT results, are very important for early diagnosis [1,2,3].
The second and most important part is the summary of anticoronavirus medications:
First of all, different versions of anti-coronavirus medications exist, both domestic and abroad, and expert opinions are also inconsistent, indicating that there is no specific anti-coronavirus drug, especially hydroxychloroquine. Although this patient had been using hydroxychloroquine for almost 3 weeks, no obvious therapeutic effect has been observed [14,16].
In addition, anti-coronavirus drugs have large adverse reactions and many interactions, so they should be observed and stopped in time. Pay attention to the adverse effects of drugs: including liver damage and myocardial damage; currently, ongoing clinical trials of antiviral drugs are mostly focused on patients with mild to moderate illness. Whether antiviral treatment is effective for severe patients requires clinical trials to clarify;
There is also the use of drugs to maintain the balance of tissue and organ function, such as glucocorticoids. Some members of our treatment group used to work in the SARS ward in 2003. During the treatment process, it was observed that patients had severe side effects such as bone fibrosis or lung tissue fibrosis after treatment [20,21]. Therefore, for this type of drug, attention should be paid to the time and conditions of use and withdrawal [1,2].
For anti-secondary infection drugs, we should be alert to the possibility of fungal infections. At the same time, we should pay attention to the comprehensive judgment of PCT, CRP, GM experiment and other indicators, and adjust antibacterial drugs. It is best to be able to clarify the type of bacteria, combined with drug sensitivity tests to clarify the type of drugs used [22].
Finally, nutritional support is the basic treatment for new coronary pneumonia.
Many medical websites now discuss the idea that many COVID-19 patients died of starvation. In fact, nutritional support is crucial for the treatment of many diseases, including COVID-19. Therefore, it is necessary to strengthen the nutritional risk screening and nutritional assessment of patients. According to the consensus requirements, patients with normal gastrointestinal function and oral intake that can meet the target energy and target protein requirements can be given a balanced diet. Malnutrition is the main problem that causes and aggravates the disease [23,24].
For patients unable to eat, tube feeding enteral nutrition can be given, but the gastric tube itself may also become the source of infection. Therefore, do not abuse parenteral nutrition, and it is not recommended to use parenteral nutrition alone or supplemental parenteral nutrition combined with enteral nutrition early [25].
This treatment group has not been used early, but only when the patient’s condition gets worse, and the treatment group starts to use it when the gastric tube is reserved before the patient’s condition is getting worse. However, the effect of use shows that nutritional therapy and attention to energy, protein supply and fluid balance are very important to improve the disease.
The above content is the experience summed up by our treatment group during the whole treatment process, hoping to serve as a reference for fellow practitioners.
References
- (2020) Testing Collaboration Group Research Laboratory of Key Projects in COVID-19 Prevention and Control Command Office of the Guangdong Provincial Department of Science and Technology,Expert consensus-based laboratory testing of SARS-CoV-2 in Guangdong Province. Int J Respir 40(22): 1681-1689.
- National Health Commission of the People's Republic of China.New Coronavirus Pneumonia Laboratory Testing Technology Guide[EB/OL].
- Duan XZ,Wang XC,Yu P, Liu W, Li X, et al. (2020) Effect of virus inactivation on weak positive results of nucleic acid test for 2019 Novel Coronavirus[J].Zhonghua Jian Yan Yi Xue Za Zhi. 43(4): 358-363.
- Ying W, Qian Y, and Kun Z (2021) Drugs supply and pharmaceutical care management practices at a designated hospital during the COVID-19 epidemic. Res Social Adm Pharm 17(1): 1978-1983.
- Yang R, Yu Y (2020) Glucocorticoids are double-edged sword in the treatment of COVID-19 and cancers. Int J Biol Sci 17(6): 1530-1537.
- Cari L, De Rosa F, Nocentini G and Riccardi C (2019) Context-Dependent Effect of Glucocorticoids on the Proliferation, Differentiation, and Apoptosis of Regulatory T Cells: A Review of the Empirical Evidence and Clinical Applications. Int J Mol Sci 20(5): 1142.
- Shi Y, Huang Y, Zhang TT, Cao B, Wang H, et al. (2019) Chinese guidelines for the diagnosis and treatment of hospital-acquired pneumonia and ventilator-associated pneumonia in adults (2018 Edition). J Thorac Dis 11(6): 2581-2616.
- Masaji N (2016) High-Flow Nasal Cannula Oxygen Therapy in Adults: Physiological Benefits, Indication, Clinical Benefits, and Adverse Effects. Respiratory Care 61 (4): 529-541.
- Yang Y, Lu Q, Liu M, Wang YX, Zhang AR et al. (2020) Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China [J]. medRxiv.
- Shen Y, Huang S, Kang J, Lin J, Lai K et al. (2018) Management of airway mucus hypersecretion in chronic airway inflammatory disease: Chinese expert consensus (English edition). Int J Chron Obstruct Pulmon Dis 13: 399-407.
- Esam Z (2020) Protective potential of expectorants against COVID-19. Med Hypotheses 142:109844.
- Alexaki VI, Henneicke H (2021) The Role of Glucocorticoids in the Management of COVID-19. Horm Metab Res 53(1): 9-15.
- Huang Y, Cai C, Zang J, Xie J, Xu D et al. (2020) Treatment strategies of hospitalized patients with coronavirus disease-19 [published correction appears in Aging (Albany NY) Aging (Albany NY) 12(12): 11224-11237.
- Zhang J, Xie B, Hashimoto K (2020) Current status of potential therapeutic candidates for the COVID-19 crisis. Brain Behav Immun 87: 59-73.
- Fan L, Liu H, Li N, Liu C, Gu Y, et al. (2021) Medical treatment of 55 patients with COVID-19 from seven cities in northeast China who fully recovered: A single-center, retrospective, observational study. Medicine (Baltimore) 100(2): e23923.
- Infante M, Ricordi C, Alejandro R, Caprio M, Fabbri A (2021) Hydroxychloroquine in the COVID-19 pandemic era: in pursuit of a rational use for prophylaxis of SARS-CoV-2 infection. Expert Rev Anti Infect Ther 19(1): 5-16.
- Singh B, Ryan H, Kredo T, Chaplin M, Fletcher T (2021) Chloroquine or hydroxychloroquine for prevention and treatment of COVID-19. Cochrane Database Syst Rev 2(2): CD013587.
- James PT, Ali Z, Armitage AE, Bonell A, Cerami C et al. (2021) The Role of Nutrition in COVID-19 Susceptibility and Severity of Disease: A Systematic Review. J Nutr 151(7): 1854-1878.
- Lin YM, Wang M, Sun NX, Liu YY, Yin TF, et al. (2019) Screening and application of nutritional support in elderly hospitalized patients of a tertiary care hospital in China. PLoS One 14(3): e0213076.
- Zuo W, Zhao X, Chen YG (2009) SARS Coronavirus and Lung Fibrosis. Molecular Biology of the SARS-Coronavirus. 22: 247-258.
- Zhou BP, Lu PX, Chen Q (2015) SARS. Diagnostic Imaging of Emerging Infectious Diseases. 5-27.
- Lee MS, Oh JY, Kang CI, Kim ES, Park S et al. (2018) Guideline for Antibiotic Use in Adults with Community-acquired Pneumonia. Infect Chemother 50(2): 160-198.
- Schaible UE, Kaufmann SH (2007) Malnutrition and infection: complex mechanisms and global impacts. PLoS Med 4(5): e115.
- Katona P, Katona-Apte J (2008) The Interaction between Nutrition and Infection. Clinical Infectious Diseases 46(10): 1582–1588.
- Feinberg J, Nielsen EE, Korang SK, Engell KH, Nielsen MS, et al. (2017) Nutrition support in hospitalised adults at nutritional risk. Cochrane Database Syst Rev 5(5): CD011598.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.