Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
COVID-19 and Venous Thromboembolic Disease Clinical Case
*Corresponding author: Merly Yamile Jurado Hernández, Hospital Departamental de Nariño E.S.E, Parque Bolivar-San Juan de Pasto- Nariño-Colombia, Colombia.
Received: December 26, 2021; Published: January 03, 2022
DOI: 10.34297/AJBSR.2022.15.002086
Case Report
Patients hospitalized with COVID-19, have an increased risk of Venous Thromboembolism (VTE), especially those admitted to Intensive Care Units (ICU), due to an excessive inflammatory reaction, hypoxia, prolonged immobilization, and diffuse intravascular coagulation. Therefore, having reliable data about the incidence of thromboembolic complications in these patients is of major importance [1]. We are present a clinical case of 48-year-old male who presented sudden pain in the left pelvic limb, associated edema and changes in color and temperature. He reported dyspnea mMRC2 that progressed to mMRC4, as well as dry cough and pleuritic pain in the left hemithorax. At physical examination BMI 25.7 Kg/m2, BP: 110/70mmHg, SpO2: 87% at room air. Chest with decreased breath sounds in the left infra-scapular region, bilateral crackles in infra-scapular region. Tachycardic and Rhythmic heart, Lower extremities asymmetric, left leg hypertrophic, with hard edema, without fovea, grade III, with hyperemia, erythema and pain on palpation, capillary refill 4 seconds; pulses were present; a positive Homans and Olowe signs were found.
Wells DVT score 3 points. Wells PE score 9 points. Geneva score 15 points. PERC score 4 points. US Doppler reporting a thrombus in the left femoral vein. Initial laboratory workout reported D-Dimer 4,700 ug/L, ferritin 2535 ng/ml, PCR 270 mg/l, fibrinogen 934 mg. CPK / MB 106/11 U/L. CBC: Hgb 12.8 gr, leukocytes 24,400, platelets 205.000. BNP 10 pg./ml. PaO2/FIO2 = 142 mmHg. EKG: sinus tachycardia, SQ3T3 pattern, as well as late R in AVR suggestive of dilatation of the right ventricle. No evidence of growth of heart chambers (Figure 1b). Chest radiograph showed bilateral consolidation of peripheral distribution, predominantly left basal, classified on the ERVIN scale as severe (Figure 1a). Contrast chest angiotomography showed hypodense-filling defect in the subsegmetary branch for the upper basal and posterior basal segment of the left lung, with the presence of a lung consolidation area. Furthermore, a hypodense image was also observed, of triangular morphology at the pleural base which did not present reinforcement in the contrasted phase in relation to the zone of pulmonary infarction (Figure 2a), in lung window axial Multiple pulmonary consolidations of peripheral distribution were observed, related to the typical SARS CoV-2 pneumonia, specifically type C pattern, with a severe degree involvement (Figure 1c and 1d). Therefore, the patient is considered a COVID-19 suspected case and nasopharyngeal sample for real-time PCR was performed with was later reported positive.
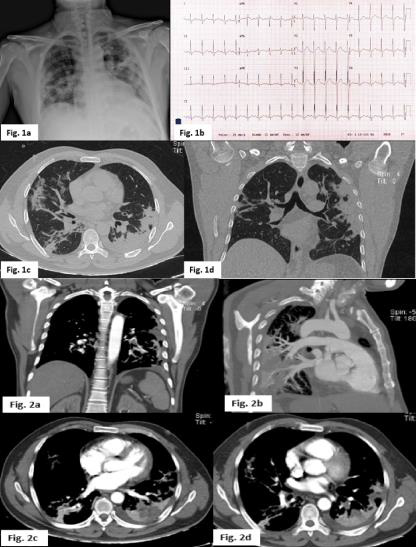
Figure 1: a Chest radiograph in anteroposterior projection with multiple ground glass images and bilateral consolidation. Figure 1b SQ3T3 pattern electrocardiogram as well as late R in AVR suggestive of dilatation of the right ventricle. Figure 1c and 1d Axial section lung window: Multiple pulmonary consolidations of peripheral distribution are observed in relation to the typical pattern with SARS CoV-2 pneumonia with a type C pattern, with a degree of severe involvement. Figure 2a and 2b. Contrast-phase computed tomography with hypodense bundle defect in the upper basal segment and the left posterior basal segment. Figure 2b and 2c Hypodense image, with pleural based triangular morphology that does not present reinforcement in the contrasted phase in relation to the zone of pulmonary infarction.
During the patient admission, full-dose anticoagulation was started with Low Molecular Weight Heparin (LMWH), as well as treatment for severe COVID-19 pneumonia with 500 mg of azithromycin for 6 days and 300 mg of chloroquine for 7 days. The evolution was favorable, and the patient was discharged with direct oral anticoagulants. Coronavirus disease 2019 (COVID-19) is a respiratory viral infection that might cause a severe acute respiratory syndrome (SARS-CoV-2), predisposing to thrombosis due to excessive inflammation, platelet activation, stasis, and endothelial dysfunction [1]. The presence of microthrombotic disease in the pulmonary arteries as well as the coagulopathy associated with COVID-19 has led physicians to consider Pulmonary Embolism (PE) as the etiology of patients with acute respiratory deterioration. In case reports of patients with COVID-19, PE was identified i without VTE risk factors [2]. cases series of post-mortem autopsies found that venous thromboembolism was present in 58% patients with COVID-19, being PE the direct cause of death [3]. In a single center in France demonstrated the possibility of higher thrombosis incidence in patients with COVID-19 critically i ll, comparing the rates of PE with the number of patients admitted to the same ICU one year earlier and also with patients admitted with influenza in 2012; at the time of analysis, 20.6% of the COVID-19 patients had PE, In comparison, general ICU population one year earlier and the population with influenza in 2012 had PE rates of 6.1% and 7.5%, respectively. The PE cumulative incidence at 15 days in the COVID-19 population was 20.4% [4].
A more recent and larger study reviewed 184 COVID-19 patients admitted to the ICU at three centers in the Netherlands; all patients received standardized doses of subcutaneous nadroparin although the exact dose regimen varied by center. In this study, the outcome was defined as any of following: DVT, PE, ischemic stroke, myocardial infarction, or systemic arterial thrombosis, and all events were symptomatic. The initial study reported 31 events (25 PE, 3 DVT and 3 strokes) representing a cumulative incidence of 31% but affecting only 16.8% of patients. It should be noted that 7 of the 25 cases of PE were limited to the subsegmental arteries [5]. Regarding deep venous thrombosis, the data suggests a higher prevalence in hospitalized patients with COVID-19 and that it is also associated with worse prognosis. The proportion of patients with DVT is strikingly high (46%). The researchers note that 65% of cases occur in the distal veins, making it easy for physicians to go clinically unnoticed. It is unknown if DVT is a problem caused by the coronavirus itself that produces an aggravation of the condition or simply is another marker that appears in patients in the context of severe systemic involvement. Researchers performed echocardiograms in 55% of patients and found that among individuals with DVT there was a slightly higher proportion of patients with pulmonary hypertension.
However, only three CT studies of the pulmonary arteries were performed, so it is not possible to establish if this high incidence of DVT resulted in an increased risk of developing pulmonary embolism. In any case, it seems reasonable to think that COVID-19 infection may be an additional risk factor for the development of DVT [4]. The interest of the present case highlights the need to be alert for any clinical manifestation that may resemble COVID-19 respiratory infectious process. The association of venous thrombosis and symptomatic pulmonary thromboembolism is frequent. The risk severity stratification of the PE event is low [6]. Chest angiotomography shows a single segmental embolism with pulmonary infarction. Biomarkers reflect the systemic inflammatory process of COVID-19 and not necessarily venous thromboembolism.
Abreviatures: VTE: Venous Thromboembolism, ICU: Intensive care units, COVID-19: Coronavirus disease 2019, SARS-CoV-2: severe acute respiratory syndrome, PE: Pulmonary Embolism
Conflicts of interest
No conflicts of interest.
References
- Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, et al. (2020) Incidence of Venous Thromboembolism in Hospitalized Patients With COVID-19 N. J Thromb Haemost 18(8): 1995-2002.
- Danzi GB, Loffi M, Galeazzi G, Gherbesi E (2020) Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J 41(19): 1858.
- Xu JF, Wang L, Zhao L (2020) Risk Assessment of Venous Thromboembolism and Bleeding in COVID-19 Patients. Research Square.
- Zhang L, Feng X, Zhang D, Jiang C, Mei H, et al. (2020) Deep Vein Thrombosis in Hospitalized Patients With COVID-19 in Wuhan, China: Prevalence, Risk Factors, and Outcome. Circulation142(2): 114-128.
- Klok FA, Kruip MJHA, Van der Meer NJM, Arbous MS, Gommers DAMPJ, et al. (2020) Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 191(1): 145-147.
- Maestre Peiró A, Gonzálvez Gasch A, Monreal Bosch M (2017) Update on the Risk Stratification of Acute Symptomatic Pulmonary Thromboembolism. Rev Clin Esp 217 (6): 342-350.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.