Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Emergency Department Disposition Optimization
*Corresponding author: Muhammad Shahbaz Aziz, Air University Islamabad, Pakistan.
Received: December 14, 2021; Published: January 12, 2022
DOI: 10.34297/AJBSR.2022.15.002096
Abstract
Emergency department disposition process has changed a lot in recent years. To ensure the maximum public welfare and optimize the healthcare system, the emergency department disposition strategies should be updated regularly. This mini-review compiles the latest trends in emergency department disposition and suggests some improvements in context of COVID-19 pandemic.
Keywords: Emergency Department, ED Disposition, Healthcare System, COVID-19, Physician, Drug, Re-Assessment, Contingency Planning, Training of Personnel, Methodologies, Floods, Harmonise
Introduction
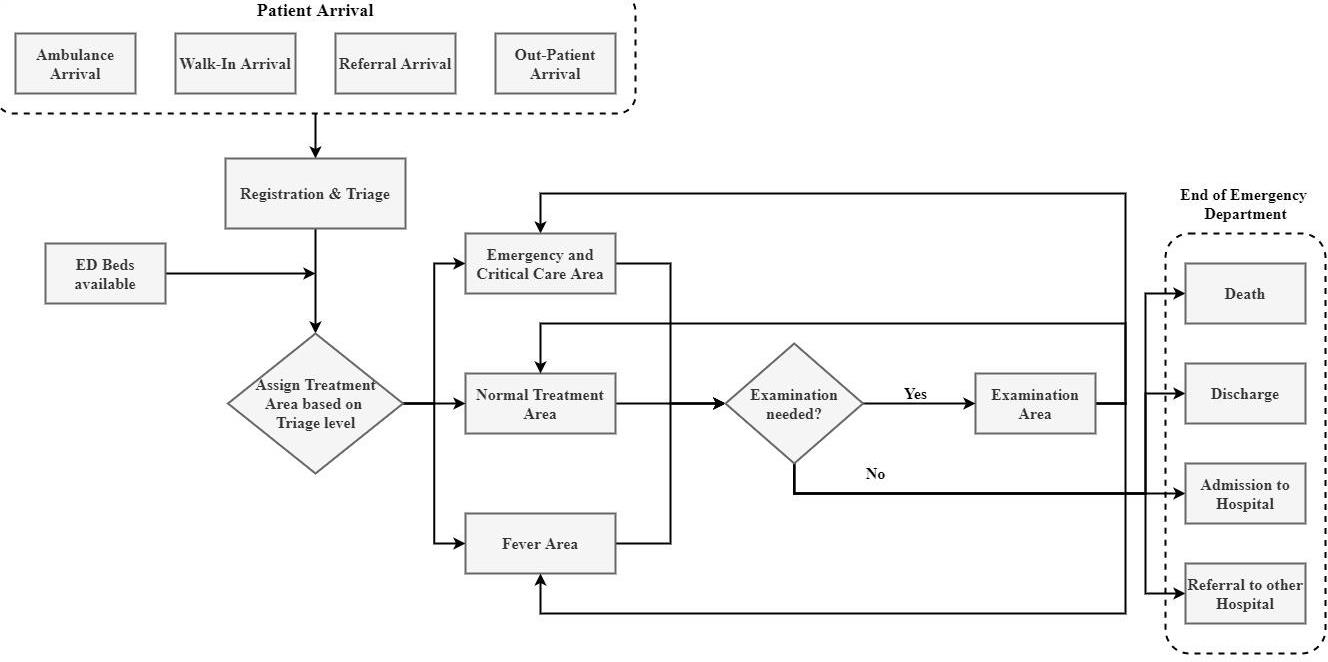
Emergency department serves the most crucial purposes within medical healthcare centres providing emergency care and treatment to patients needing instant medical attention [1]. It is a challenging task to acquire a clear overview and understanding of overall process involved in an Emergency Department (ED). This is due to the tempestuous work atmosphere and a large variation in specific patient processes [2]. Whenever a patient arrives at an emergency department of a hospital, he is examined and evaluated by the available physician. He is then given medication and an assessment is made based on drug therapy monitoring. Then, based on the re-assessment, comes the disposition decision in which it is decided whether the patient should be admitted for further medical care or whether the patient should be discharged. Figure 1 gives a descriptive representation of sequence of steps in the emergency department disposition (Figure 1) [1]. This paper is concerned with assessing the medication therapy for a patient and optimization of disposition decision for the patient to minimize the chance of a follow-up injury.
Pre-Event Strategies
The continuous working of hospitals is vital for offering healthcare services to the injured, both in ordinary and in situations of disasters. In addition to affecting individual persons, disasters have drastic impacts on the functional, structural as well as non-structural constituents of hospitals. Hospital preparedness is an essential part of disaster management cycle. There are nine components of disaster management preparedness. Planning is the most essential component among them. It includes formulating policies and programs to reduce disaster consequences. Hospitals must stay functional during disasters, and the evaluation of hospital readiness is important to safeguard this issue. Substantial steps in the healthcare industry can be taken to prevent and neutralize the effects of disasters although they are often unforeseen. Response capacity of the communities can also be strengthened by making policies towards disaster management. Essential widespread methodologies are needed to be adapted in current Medicare industry to account for complications of emergency preparedness. In particular, the preceding regulations did not address the need for:
a) Communication to harmonise with other healthcare
systems within cities or states
b) Contingency planning
c) Training of personnel
Preparedness is important to secure the right to live in confidence and dignity. States withstand the primary accountability for protecting their populations and guaranteeing an honorable life but the up-to-date methodology to preparedness ranges well beyond those traditionally involved in relief efforts, such as civil protection forces, emergency offices and humanitarian organizations. Communities need to collaborate with concerned authorities and public organizations to fortify and strengthen their own capacities to prepare for and manage numerous threats [3]. In addressing these issues, the World Health Organization (WHO) has established a wide-ranging strategy for pre-event preparedness based on the metrics of past catastrophes. The response to the floods in Mozambique in 2000-the worst for over a century-was a great achievement. Media headlines celebrated the helicopter rescue of a mother who gave birth while taking shelter in a tree.
Fewer reported were the 45 000 lives saved, mostly by native rather than international saviors. More floods hit Mozambique a year later. Native teams saved over 7000 survivors. The floods hitting in 2001 had an insignificant effect in terms of loss of lives as the result of good practice of management of the floods in 2000 [4]. Mozambique well surpassed expectations in preparedness for a low-income country. 1997 Bangladesh cyclone is also another welldocumented case that affected Cox’s Bazaar region of southeast Bangladesh, leaving 1.5 million people homeless. There were only 127 fatalities in this incident although it was stronger than one in 1991 that killed 138,000 people [3]. The small death toll was low because the cyclone struck during the day and at low current. However, an active community based early-warning and emigration system and cyclone shelters for emigrant were critical issues in saving so many lives.
Major emergencies, disasters and other crises are social, economic, and political events. In the previous decade, the total number of disastrous events has almost doubled, presenting a trend mark from around 450 to 800 major emergencies per year [4]. The middle and low-income countries, where emergency preparedness is frequently insufficient, there is a noticeable increase in emergencies per year. Less people are dying from disastrous events because of established preparedness in many countries, but the amount of people affected by them is still cumulative, with significant long-term consequences. In 2005, an estimated 157 million people were directly affected by natural tragedies. In addition, complex emergencies and calamities are long long-term and are a source of a countless premature deaths and massive distress. The number of migrants and internally displaced individuals aided by the United Nations High Commission for Refugees (UNHCR) increased from 171 million at the beginning of 2004 to 208 million by the beginning of 2006 [5].
LWOT (Left Without Treatment)
LWOT (left without treatment) patients who are triaged but were unable to be assessed by a healthcare provider since they have left the emergency department. These patients are divided into 3 categories: LWBS (left without being seen), AMA (against medical advice) and elopement cases. The global LWOT rates are approximated at 6.14-11.26% [6]. ED methodologies can be redesigned to reduce the time to provider, ALOS (average length of stay) and hence LWOT rates can also be dramatically decreased [6]. Identification of potential LWBS patients is important to decrease the percentage of these events. Improvement in LWBS rates generally relate to improved patient satisfaction and decreased liability among health care organizations. It motivates healthcare professionals to deter patients from early exits from the emergency departments excluding the patients who are potentially dangerous for themselves or others. Nurses can take an active role in the process by observing patient condition and an improved awareness of the departure process and realization of the significance of discharge planning in nurses can empower the process significantly [7].
PDCA Methodology
PDCA methodology is a very strong suit in nursing and healthcare services to deal with complicated medical situations. It is so effective that one of the most brutal recent pandemics, COVID-19 is being mostly dealt by application of PDCA methodology worldwide [8,9].
PDCA refers to Plan, Do, Check, Action into methodology. The current outstanding problems facing the management of hospital care generally has four aspects:
a) New changes are needed to meet the general healthcare
requirements and to deliver better healthcare facilities.
b) A more patient centric approach to deepen the overall
healthcare needs.
c) Better healthcare quality management and standardization.
d) Gradual replacement by public health insurance, with low
medical expenses for the patient needs.
Nursing management should adapt cross-century concept of change and strategic choices, calling for new thinking, new ideas, new strategy, and new methods of nursing management. These changes should not only reflect in better overall healthcare services but a more satisfied and quickly recovered patient [10]. PDCA promote the theoretical knowledge in nursing staff in the hospital. People, who can master the use of PDCA theory work in healthcare, develop good work habits, have rigorous style of work, systematically carry out every task, and develop a sense of mutual inspection. The integration of individual ring in PDCA loop and small departments snowballed to promote the hospital’s large PDCA loop ladder rise repeatedly [11]. Four stages of PDCA cycle are not separate, but closely co-coordinated fused, having a certain amount of cross phenomenon between stages. The specific workflow is as follows: present the goals; understanding the problem; analyse the reasons; develop measures; implement the measures; check the effect and learn lessons for the next PDCA.
Planning phase P(Plan)
Firstly, a clinical nursing path group is formed from existing staff, which is controlled by the department management. An indepth literature review is carried out regarding clinical pathway by ministry of health. Then particular needs of patients are tracked and are matched with specific departmental circumstances. In this way, a clear pathway is formed to enact upon. Essential measures are developed to prevent any further loss. Operating standards and procedures are made clear to involved staff and everything is systematically planned. A clear roadmap is very important to avoid blunders and to achieve pre-set targets, which is not possible to have a clear roadmap without proper strategic planning. Administrative decisions in budget determination and resource management are mostly guided by these pre-planned roadmaps. This results in fulfilling the targets and increase in operational efficiency. Planning before enacting is very crucial in order anticipate any unfavourable circumstances and it increases sense of responsibility in the healthcare staff. Prediction of natural disasters or a pandemic is very difficult because of the extremely complex nature of the healthcare industry. A long-lasting foundation, focus and anticipation is needed for healthcare organizations to compete with status of medical needs.
Implementation phase D (Do)
In implementation phase, specialized healthcare techniques are adopted best suited to current circumstance. Market and stakeholder analysis play very important role in implementation process. Firstly, important data is gathered and a team is engaged to find solutions. Implementation studies often employ multifaceted or complex interventions aimed at different levels of the health system. Then, applicability of solutions and policies are tested in the given environment. Lastly, the policies are implemented following a pre-planned pathway and it is ensured that proper methods are enacted to sustain the new policy use. The implementation phase is a substantial step towards successful PDCA methodology as it ensures proper action on the proposed policies and methods during the planning phase.
Checking phase C (Check)
All healthcare workers are accounted for random checks on quarterly basis by management and board of members. Common issues are identified and rectified by live scoring and relevant guidance by senior administration and unified training by PDCA audits. Inspection and supervision personnel than identify the individual problems within individual departments and notify the relevant authority. Department head nurse assess the undergraduate nursing group once a month to resolve the issues. All healthcare personnel participate in a unified examination, unified scoring, and nurse’s mutual evaluation process. Then the important matters and issues identified are discussed to implement improvement measures. Nurses and other crucial staff members are passed through appraisal process, which focuses on strengthening humanistic care of the staff and motivates them to respect the needs of patient. It focuses on patient-centred approach to enhance communication with patients. Quality of healthcare is drastically improved through this progression, where patients can practice their right to information and right to choose therefore, patient satisfaction is highly revamped. Execution of PDCA methodology in healthcare and emergency departments can result in improved efficiency and better healthcare services:
a) The healthcare industry cannot bear the expense of huge
errors and a slight error can cost us lives. These errors can
be substantially reduced by effective planning. In this way,
major mishaps can also be avoided in emergency department.
The quality of services is also improved and operations are
organized better in a hospital or medical facility.
b) Many unforeseen circumstances can be prevented by
implementation of the PDCA cycle in the healthcare industry.
Adequate stocks and resources for keeping a healthcare facility
functional can be guaranteed by the PDCA methodology.
c) Common malfunctions can be avoided successfully just by
implementing PDCA cycle in daily healthcare processes. These
malfunctions are eliminated while planning phase of PDCA
cycle.
d) Operational efficiency is optimized by further altering the
process with the help of different phases of PDCA methodology.
Healthcare industry is needed to be updated and modified to
stay relevant with respect to technological advances.
e) PDCA helps in minimizing the medical effluents to a huge
extent. Managing the medical effluent is main concern in
healthcare industry. For example, expired medicines, used
cotton, needles that need right environment for disposal. PDCA
technique implementation can help clearing such waste.
f) The do phase of PDCA cycle can hugely contribute to testing
process in healthcare industry. This vigorous testing result in
some efficient techniques for the administration to follow.
g) Apart from human serving, healthcare industry also has profit
targets in its agenda. PDCA cycle can ensure a good business
market if patients are observed as a customer perspective. It
brings in more profit if the patient’s confidence in the services
sustain.
Assessment
Patients are initially unclassified and unspecified upon their arrival on the facility. Followed by a pre-hospital evaluation, some are directed to see a clinician and others are referred to various departments on case-to-case basis. Having a reliable and efficient procedure to sort out patients according to their clinical needs is very essential for a healthcare organization. These practices differ widely among urgent and emergency healthcare systems due to wide variety of functionality each one offer based on the location. Therefore, we cannot adapt same assessment approach for every healthcare system. There are three main objectives of good quality initial assessment:
a) Better safety aspects
b) To ensure that the most serious patients are treated within right time frame by relevant service provider. This is done by identifying acuity and setting prioritization.
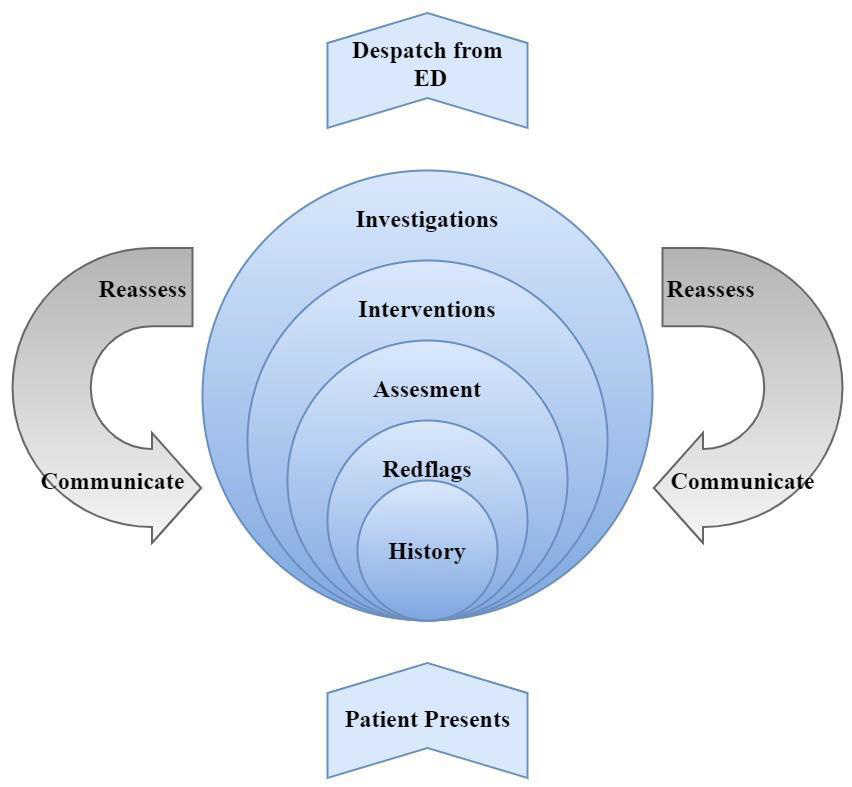
c) Lowering the length of stay by minimizing unnecessary wait that patient suffer for diagnostics and availing other services. The following steps are involved in a proper assessment of the condition of admitted patient [12] (Figure 2).
Taking History
During identification of the acuity of the patient’s condition, it is vital to discover the patient’s health history with reference to present illness. It is very important to know about any allergies and past medication before any treatment or medication. Some of the key points should be noted while taking a patient’s history:
a) Associated symptoms
b) Significant events in past 24h/mechanism of injury
c) Past medical history/past surgical history
d) Allergies
e) Current treatment for the presenting problem
f) Social history
g) Pain history
h) Medication
i) Last menstrual period
These key points should be inquired from the patient to obtain a comprehensive understanding of the present illness and any precautions that should be taken under account during the treatment. Making assumptions about clinical history of the patient should be avoided until an ample data is collected and final evaluation is ready. A good example is that, for a case of a patient with pleuritic chest pain, cardiac pathology cannot be ignored without leading an in-depth evaluation. The pleuritic chest pain may be masking other symptoms, or the patient may have two medical conditions [13].
Step 2: Potential ‘red flags’
Determination of the degree of threat to life is the priority in medical intervention. In many cases, emergency nurse can determine severity of the case within seconds of encounter with the patient. Some examples of this may be an adverse central crushing chest pain, major accident, or a cardiac arrest. However, there are some exceptions. Consider a 35-year-old asthmatic diaphoretic male with a case of shortness of breath who needed intensive care 1 year ago and a 70-year-old with a fever. Both patients may be characterized as severely ill and might require immediate medical attention. It will be a lot more difficult to prioritize these two cases but an emergency nurse must be able to identify the potential severity of illness of both the patients and thus, serve them with appropriate healthcare services within a busy emergency department.
The need of immediate medical intervention and determination of acuity of the illness is based on combination of symptoms, clinical signs, and medical history of the patient. For example, abnormal vital signs, medical history of cardiac disease or time sensitive characteristics can lead to a potential cardiac arrest. These historical and medical indications are termed as ‘red flags’ and are often very helpful in initial assessment of the patient. Patient medical history can lead to determination of historical red flags and clinical red flags are obtained through various medical instruments and apparatus. For example, a patient with chest pain and a medical history of diabetes, renal failure or cardiac disease can be classified as a high-risk patient based on these red flags. Final assessment should not be assumed until all high mortality conditions have been completely ruled out. Each patient should be observed with respect to worst case scenario possible and this approach is called ‘worst first’. For example, life threatening conditions should be identified and ruled out first for a patient with severe chest pain [13]. Emergency department nurses often use pattern recognition to evaluate the urgency of healthcare needed. This together with information gathering and probability judgement can guide the nurse to a probable diagnosis, which may change with further assessment and reassessment.
Clinical examination
The clinical examination is the next step in process of assessment. Generally, ABCD (Airway, Breathing, Cardiac and Disability) mnemonics are followed in clinical examination in emergency nursing facility. This methodology can assess potential life threats by evaluation of basic vitals such as breathing, blood circulation, cardiac rhythms, and neurological functions. If a major threat to life is discovered during clinical examination than immediate medical intervention may need to be taken. Following the ABCD assessment, the emergency department nurse can continue with a fixated assessment, generally guided by the vital signs, presented symptoms, or the mechanism of injury [14]. For example, initially a patient will be assessed for ABCD threats after presenting a painful ankle following an accidental fall, followed by a focused assessment of distal limb. Collection of patient’s data through laboratory test and diagnostics are also an important part of clinical examination. In cases with psychological disorders, problems related to environmental and social factors are also considered during examination.
Nursing interventions
During nursing assessment, several steps might be taken under consideration at a same time due to highly nonlinear and interactive nature of the nursing process. For example, a patient might be asked about his medical history while a healthcare personnel taking their vitals and taking note of his body mobility at the same time. During this rigorous assessment of the patient, you might get an opportunity to initiate simple but effective medical interventions according to the patient’s needs. For example, taking blood pressure readings, application of oxygen therapy and collection of blood for laboratory examination can be performed concurrently. The reassessment of patients is also carried out through verbal or written communication after nursing interventions, to check for any allergies or reactions.
Pre-Implementation
Pre-implementation is preparing the staff members and teams related to the project for upcoming phases. Following major steps are considered in this step:
Education: The healthcare staff should be educated and trained individually for the designated protocol. Every healthcare executive should know his or her duties and respective response for specific circumstances.
Scripting: Scripting is the next step to be carried out. Scripting provides the basis for initiating or redirecting a conversation as well as work towards improving patient satisfaction. Scripting can establish a sense of empathy and respect for the patients, which are two very important aspects of healthcare ethics and interaction. Some healthcare systems utilize scripted patient satisfaction survey questionnaire as the foundation for improving customer satisfaction and healthcare metrics
Policy review: Regularly visiting your policies for reviewing based on feedback you get is an essential step towards providing more efficient and better healthcare services. It ensures that the policy follows different regulations and standards.
Marketing: Communication with target audience plays a crucial role in establishing a healthy stakeholder relationship. Modern marketing techniques should be practiced regularly to close the gap between patients and healthcare organizations.
Waiting room or patient flyers: Patient education brochures and flyers can break-down various symptoms, simplify complicated medical procedures and help in spreading awareness about a particular contagious disease. They enable patients to remember important information through visual stimulus before leaving the healthcare facility.
Communication with stakeholders: Communication and exchange of information between different stakeholder play an important and strategic role in proper functioning of a healthcare regulatory environment. Relationship with stakeholders can be strengthened significantly through effective.
Implementation
Implementation of the policies is actual practical work to do and it needs personal attention at micro level. Implementation of personalized schedules and shift management for healthcare staff is the first step in this regard. Awareness of duties and appropriate response according to the situation is second step. This process can be made much efficient by keeping track of issue log and proper documentation. Effective clinical communication also needs proper nursing documentation. Appropriate documentation and record keeping help in formulating a precise and accurate methodology for nursing assessments [15]. A shift assessment should be performed before start of each shift to keep the nursing process in compliance with the guidelines. The information for this assessment can be gathered from documentations, records, patient introductions, safety checks, clinical observations, and an Electronic Medical Records (EMR) review. EMR uses latest technology to keep patient information and deliver an overview of patient’s condition. Specific tabs are used in EMR which are used to meet specific requirements of patient group. It helps each ward to regulate the activities based on the patient population. Following tabs and information can be recorded in EMR:
a) Storyboard-age, gender, FYIs, infections, allergies, length of
stay, weight etc.
b) IP Summary-Medical problem list, treatment team, orders to
be acknowledged.
c) ViCTOR Graph-observations trends, zone breaches
d) Notes- e.g., admission, ward round, any other useful details
(mark all as not new)
e) Results Review-recent and pending results (time mark)
f) MAR- overdue medications, discontinued, adjust due times for
medications
g) Fluid Balance-input/output and balance
h) Avatar-review lines/drains/airways/wounds, including,
location, size, date inserted
Complete Information about the event occurred along with details of impact, plan to deal with concerned patient and family should be describes by the progress note entries. Non-specific details should be avoided only the relevant data to the individual patient should be listed accurately. Duplication of information should also be strictly avoided. In this process, other activities related information on the EMR are not useful. All entries should use professional designated nursing language. Use of abbreviations should be minimal, and if used, they must comply with RCH standards [16].
Post-Implementation
In the process of post implementation, we are mainly concerned with the patient reviews and using them to track any potential issues or problems. Emergency department work group work closely with stakeholders to improve the existing policies in the department. Daily management board and senior leadership also plays an important role in the process. Following tasks are carried out in this phase.
a) Reassessment of patient after medical intervention.
b) Reviewing and revising the initial nursing plan to meet the
present complications and nursing needs.
c) Anticipating and preventing any potential complications
during and after treatment.
d) Identifying the week areas of nursing and providing assistance
to improve those areas.
e) Assessment of the skills of the healthcare professionals and
utilizing them, where needed the most.
Conclusion
This paper confines and represents a detailed study on modern day emergency department disposition techniques and sequence of processes involved in the policy formulating for providing better healthcare services within the board. Pre-event strategies for disaster management and PDCA methodology for aggressive approach towards emergency department management are discussed in detail. Previous metrics for past catastrophes are being used as a reference for developing a more consistent approach towards the policies. Finally, an assessment methodology for patients and policy review are explained and final implementation steps are listed.
References
- Chen TL, Wang CC (2016) Multi-objective simulation optimization for medical capacity allocation in emergency department. J Simul 10(1): 50-68.
- K Bengtsson, E Blomgren, O Henriksson, Pettersson M (2016) Emergency department overview-Improving the dynamic capabilities using an event-driven information architecture.
- World Health Organization (2007) Risk Reduction and Emergency Peparedness. WHO Doc Prod Serv Geneva Switz Pp.20.
- United Nations (2005) World Conference on Disaster Reduction: List of Participants. pp.18-22.
- UNHCR (2006) 2005 Global Refugee Trends Statistical Overview of Population of Refugees, Asylum-seekers, Internally Displaced Person, Stateless Persons, And Other Persons of Concern to UNHCR. pp.1-105.
- Sharieff GQ, Lori Burnell, Matt Cantonis, Valerie Norton, Juan Tovar, et al. (2013) Improving emergency department time to provider, left-without-treatment rates, and average length of stay. J Emerg Med 45(3): 426-432.
- Vierheller CC (2013) Evaluating Left Without Being Seen and Against Medical Advice Departures in a Rural Emergency Department. J Emerg Nurs 39(1): 67-71.
- W Wei, S Wang, H Wang, H Quan (2020) The application of 6S and PDCA management strategies in the nursing of COVID-19 patients. Crit Care 24(1): 443.
- Y Chen, J Zheng, D Wu, Y Zhang, Y Lin (2020) Application of the PDCA cycle for standardized nursing management in a COVID-19 intensive care unit. Ann Palliat Med 9(3): 1198-1205.
- Y Wang, S Zheng (2016) Research on the Application of PDCA Theory in Nursing Quality Management. 63 Amahs pp.84-87.
- L Ma, X Hu, C Hao, F Liu, T Tian (2017) Impacts of PDCA circle’s clinical nursing path on the postoperative recovery and life quality of gastric patients. Int J Clin Exp Med 10(2): 3669-3676.
- K Curtis, M Murphy, S Hoy, MJ Lewis (2009) The emergency nursing assessment process-A structured framework for a systematic approach. Australas Emerg Nurs J 12(4): 130-136.
- Breen LM, Trepp R, Gavin N (2020) Lean Process Improvement in the Emergency Department. Emerg Med Clin North Am 38(3): 633-646.
- S Saghafian, G Austin, SJ Traub (2015) Operations research/management contributions to emergency department patient flow optimization: Review and research prospects. IIE Trans Healthc Syst Eng 5(2): 101-123.
- ER Allanson, Özge Tunçalp, Joshua PV, Dina NK, Olufemi TO, et al. (2017) Implementation of effective practices in health facilities: A systematic review of cluster randomised trials. BMJ Glob Heal 2(2): 1-12.
- AK Exadaktylos, DS Evangelopoulos, M Wullschleger, L Bürki, H Zimmermann (2008) Strategic emergency department design: An approach to capacity planning in healthcare provision in overcrowded emergency rooms. J Trauma Manag Outcomes 2(1): 11.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.