Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Minimal Deviation Adenocarcinoma of The Cervix: Still A Gynecologist Oncologist’s Nightmare
*Corresponding author: Marco Marinaccio, Interdisciplinary Department of Medicine, University Medical School of Bari, Apulia, Italy.
Received: February 14, 2022; Published: February 24, 2022
DOI: 10.34297/AJBSR.2022.15.002131
Abstract
Minimal deviation adenocarcinoma (MDA) is a rare neoplasm characterized by difficult diagnosis, no standard treatment and poor prognosis. This neoplasm accounts for 1 to 3% of all cervical adenocarcinoma, and the mean age of the patients at the time of diagnosis is 45 years old. It has a characteristic endophytic growth pattern; conventional methods for cervical cancer screening frequently fail. Here we report the case of a 44-year-old woman that underwent only medical therapy, pointing out the problems we met during the diagnosis path and the treatment planning. She came to our attention for vaginal bleeding and with pap smear that showed no cytological alterations. MRI showed polycystic and solid component enhancement, and we performed conoid biopsy twice, because the first one was not decisive. She died twenty-one months after the diagnosis.
Keywords: Minimal Deviation Adenocarcinoma, Cervical cancer
Introduction
Minimal deviation adenocarcinoma (MDA) was described for the first time by Gusserow in 1870 such as adenoma malignum because of its rapid evolution. In 2003 WHO described this rare neoplasm as a “very well-differentiated endocervical-type mucinous adenocarcinoma composed mostly of lobular endocervical glandular hyperplasia (LEGH)-looking glands but with the characteristics of obviously invasive adenocarcinoma” [1]. This neoplasm accounts for 1 to 3% of all cervical adenocarcinomas [2]. MDA represents a challenging diagnosis due to the cytological benign appearance. Ishii et al. showed that the presence of “yellowish-orange” intracytoplasmic mucin with Papanicolau staining of the smear is an important diagnostic sign, but its significance remains unclear [3]. It has a characteristic endophytic growth pattern. Conventional methods for cervical cancer screening frequently fail. Diagnosis must be histologically confirmed. Only cervical conization has shown a detection rate of 100% [4].
The mean age of the patients at the time of diagnosis is 45 years old, and the most common clinical manifestations are non-specific such as watery or mucoid vaginal discharge and irregular or contact bleeding. In most patients the cervix appears hypertrophic [1]. MDA could look similar to benign lesions such as Nabothian cysts also on transvaginal ultrasonography [4]. MRI plays an important role in MDA diagnosis [5]. MDA is more aggressive than HPV-related adenocarcinomas and is capable of metastasizing to ovaries, abdomen and omentum [6]. Surgery is the main treatment for early stages, as is the case for common adenocarcinoma of the uterine cervix, while chemoradiation therapy is recommended for advanced stages. The difficulties in providing early diagnosis remain the principal factor affecting the prognosis [1]. In this paper we present a case of MDA in a 44-year-old woman diagnosed and treated in our center.
Case Report
A 44 old Caucasian woman came to our attention from another Institution in May 2020 for AUB. The patient is gravida 1, para 1, BMI 23 kg/m2, with an absence of risk factors for inherited malignancies, in good health, and underwent regular clinical check-ups. No sign of Peutz-Jeghers syndrome was found. Clinical assessment showed the presence of an enlarged and easily bleeding portio with crumbly consistency, despite MRI showed no alteration (Figure 1-2).

Figure 1: The MRI image above was considered normal, although polycystic and solid component enhancement should be alert to MDA.
Figure 2: Sagittal section of the cervix, with multicystic lesion and solid component. No invasive tumour mass was found.
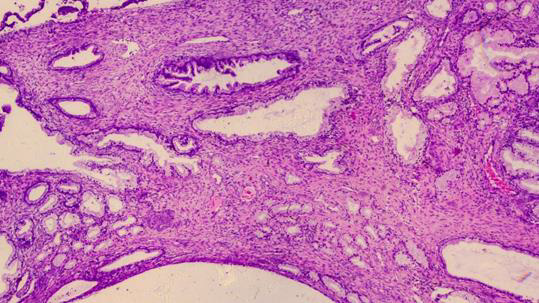
Figure 3: Gastric-type adenocarcinoma”: Histological preparation in which the presence of endocervical-type glands of different size and shape is appreciated, with lumens of various.
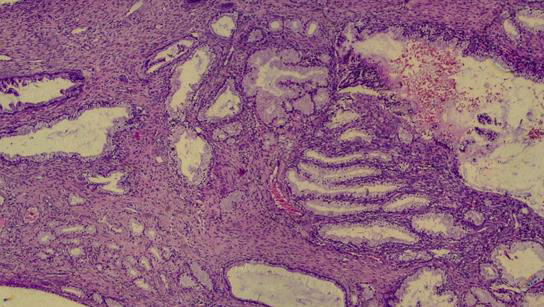
Figure 4: “HE 10X”: Photomicrograph showing the presence of glands of different sizes and shapes, with different cytokaryological characteristics: bottom and right at the top mucus-secreting glands with mild cytology and nuclei located at the base of the cells; in the center the presence of glands with more evident cytological atypia and hyperchromatic nuclei.
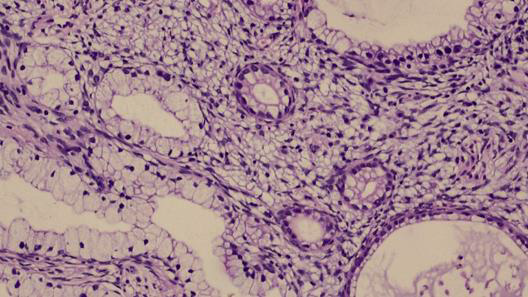
Figure 5: HE 20X”: morphological detail of irregularly shaped mucus-secreting glands that invade the fibromuscular stroma of the uterine cervix.
Despite the MRI being negative, actually guided only by the clinical data, we performed conoid biopsy twice: the first did not highlight any pathological findings, whereas the second one indicated “adenocarcinoma gastric-type minimal deviation of cervix. Vascular peritumoral permeation. Ki-67 40%; negative immuno-histochemistry for p53” (Figure 3-7). From June 2020 to July 2020 the patient was administered 2 courses of neoadjuvant chemotherapy based on Taxol (120 mg) and Carboplatinum (250 mg); she did not experience toxicities except for alopecia. MRI performed in August 2020 highlighted “a cervical bulky neoplasm of 6 cm that reaches the upper III of vagina. Parameters, bladder and rectovaginal septum appears free from infiltration. Absent lymphadenopathy.
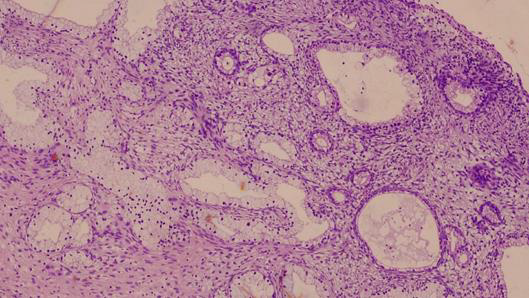
Figure 6: HE 40X” detail at 40X of the two different degrees of cytological atypia coexisting in the same neoplastic lesion.
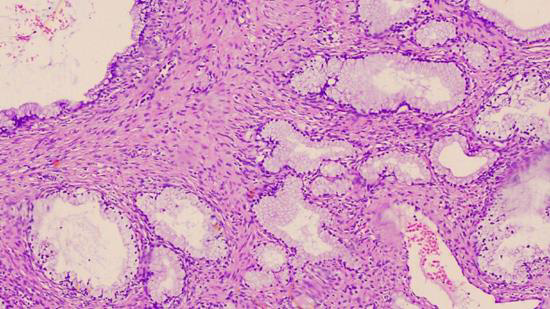
Figure 7: HE 60X”: photomicrograph showing characteristics of the two degrees of cytological atypia consisting of a low degree (to the right and left of the field) and a high degree (small glands, formed, in the center)
Stage IIA FIGO.” (Figure 8). At this point, the patient was advised to undergo radiochemotherapy, but she decides to apply to another Institution, where the case was newly assessed. Thus the patient underwent radiochemotherapy with EBRT on pelvis (45 Gy tot) and on cervical-vaginal region (31 Gy tot) with daily IGRT associated to 5 courses of Cisplatinum plus 5 sessions of brachytherapy. MRI carried out in December 2020 showed a neoplasm with 5cm in diameter, that infiltrated vaginal fornixes and likely the posterior side of bladder. In order to assess the possibility of eviscerative surgery, the patient underwent diagnostic laparoscopy, that highlighted multiple peritoneal lesions positive for metastasis, and peritoneal washing including malignant cells. Considering this findings, the option of eviscerative surgery was excluded.
Therefore, the patient returns to our Institution to begin chemotherapy based on Epirubicin. She was administrated 9 courses of Epirubicin, 140 mg for 5 courses, then decreased to 115 mg, because of severe neutropenia resistant to therapy with pegfilgrastim. The MRI scan showed that the lesion was reduced in diameter (3x3x3, 5cm). The patient had a good performance status until she began to complain severe rectorrhagia in September 2021, thus we prescribed a colonoscopy that revealed iatrogenic colitis. Consequently, we were forced to terminate Epirubicinbased chemotherapy. Patient general status started to deteriorate, with abundant ascites and cachectic state. At this point, patient underwent Gemzar-based chemotherapy (1200 mg) facing anaemia as collateral effect. She died in January 2022.
Discussion
MDA represent 1 to 3% of all cervical adenocarcinomas [2]. Unlike common cervical cancer, MDA is not HPV-related. Some authors hypothesize an association between MDA and Peutz-Jeghers syndrome but in our case there was no sign of this association. The mean age at diagnosis is 45 [5]. The clinical features are similar to those of common cervical adenocarcinoma such as watery vaginal discharge and vaginal bleeding [7]. The patient came to our attention for vaginal bleeding and with pap smear that showed no cytological alterations.
On MRI, MDA appearance may be similar to that of deep Nabothian cysts [8]. In our case the first MRI investigation showed no alteration but the clinical assessment already highlighted an enlarged portio with an increased consistency. Only the second MRI, performed four months later, showed a cervical bulky tumor of 6 cm. The definitive diagnosis is histological. We performed two conization and only the second one was diagnostic and this demontrates the endophytic growth pattern of this neoplasm [4]. Altough MDA is a very well differentiated neoplasm, it has aggressive clinical features and the diagnosis is tipically performed at a higher stage than HPV-related adenocarcinomas. It has a typical metastasis pattern that involves the ovaries, the abdomen, the omentum and other distant sites [6].
Hichimura et al. demonstrates that MDA cells contains gastric mucin and are negative for p53 protein [9].
Due to lack of studies and because of the rarity of this neoplasm, there is no standard treatment. Literature shows that treatment for MDA is similar to other common adenocarcinomas of the cervix. At the early stages surgical treatment is recommended, at more advanced stages an adjuvant chemoteraphy is offered but the efficacy is low [2]. Prognosis of MDA remain poor because of the delay in diagnosis, often performed at advanced stages when surgical tratment is not advised.
Conflicts of Interest
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
Acknowlwdgement
None.
References
- Li G, Jiang W, Gui S, Xu C (2010) Minimal deviation adenocarcinoma of the uterine cervix. Int J Gynaecol Obstet 110(2): 89-92.
- Sui M, Pei Y, Li D, Li Q, Zhu P, et al. (2016) Misdiagnosis Analysis of Cervical Minimal Deviation Adenocarcinoma: A Report of Three Rare Cases and Literature Review. Ann Clin Lab Sci 46(6): 680-690.
- Ishii K, Katsuyama T, Ota H, Watanabe T, Matsuyama I, et al. (1999) Cytologic and cytochemical features of adenoma malignum of the uterine cervix. Cancer Cytopathol 87(5): 245-253.
- Lee MH, Kim ES, Choi MC, Heo JH, Jang JH, et al. (2018) Minimal deviation adenocarcinoma (adenoma malignum) of the uterine cervix: clinicopathological analysis of 17 cases. Obstet Gynecol Sci 61(5): 590-597.
- Itoh K, Toki T, Shiohara S, Oguchi O, Konishi I, et al. (2000) A comparative analysis of cross-sectional imaging techniques in minimal deviation adenocarcinoma of the uterine cervix. BJOG 107(9): 1158-1163.
- Karamurzin YS, Kiyokawa T, Parkash V, Jotwani AR, Patel P, et al. (2015) Gastric-type Endocervical Adenocarcinoma: An Aggressive Tumor with Unusual Metastatic Patterns and Poor Prognosis. Am J Surg Pathol 39(11): 1449-1157.
- Guo F, Hu Y, Xu X, Li R, Ru T, et al. (2013) Diagnostic challenges in minimal deviation adenocarcinoma of the uterine cervix: A report of two cases and review of the literature. Mol Clin Oncol 1(5): 833-838.
- Doi T, Yamashita Y, Yasunaga T, Fujiyoshi K, Tsunawaki A, et al. (1997) Adenoma malignum: MR imaging and pathologic study. Radiology 204(1): 39-42.
- Ichimura T, Koizumi T, Tateiwa H, Yamaguchi S, Takemori M, et al. (2001) Immunohistochemical expression of gastric mucin and p53 in minimal deviation adenocarcinoma of the uterine cervix. Int J Gynecol Pathol 20(3): 220-226.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.