Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Multiple Causalities Due to Ethion Pesticide Poisoning: A Case Report
*Corresponding author: Phokedi Gothatamang Norma, Department of Chemical and Forensic Sciences, Botswana International University of Science and TechnologyPlot 10071, Boseja Ward, Private Mail Bag 016, Palapye, Botswana.
Received: February 02, 2022; Published: February 11, 2022
DOI: 10.34297/AJBSR.2022.15.002120
Abstract
Pesticide poisoning remains a serious health threat especially in developing regions such as sub-Saharan Africa. The excess pesticide poisoning related morbidity and mortality in low- and middle-income countries has been attributed to inadequate regulations governing the safe use of pesticides. The lack of regulations, along with inadequate enforcement, is related to increased risk of food, water and air contamination, and direct contact with pesticides or their residues. We hereby present a rare case, in which, an incident involving four (4) non-fatal and four (4) fatal occurred within 24hours of ethion pesticide poisoning. Ethion is available and widely used by farmers in Botswana. In this case, it was recovered from an herbal homemade mixture allegedly prepared to rid the victims of Sejeso (imaginary ailment claimed to arise from poisoning by sorcery). The information was gathered from a 20-year-old male who had also ingested the preparation but survived, medical cards and doctors from the concerned district hospital. Medico-legal autopsy findings for the 3 victims of paediatric-age were unremarkable while for the fourth, a 56-year-old male, revealed multiple co-morbidities. Toxicology analysis of the victims’ stomach contents, vomitus and blood samples confirmed the presence of ethion pesticide. The cause of death was determined as ingestion of a pesticide.
Keywords: Organophosphate pesticide poisoning, Ethion and medico-legal autopsy
Introduction
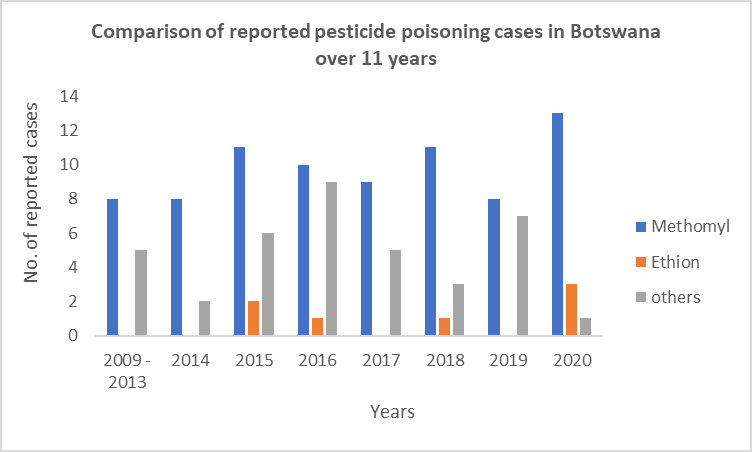
According to the World Health Organization (WHO) and Food and the Agriculture Organization (FAO), pesticide poisoning accounts for the highest numbers of poisoning morbidity and mortality worldwide [1]. Most pesticide poisoning occurs in Low and middle-income countries (LMICs) countries where these chemicals are extensively used in agriculture [1]. The global incidence of pesticide poisoning has been estimated at between 1 million and 5 million victims per year with 300,000 lethal cases [1]. The relative ease of accessibility to organophosphate based pesticides can be partly blamed for the high incidence of organophosphate poisoning in LMICs. For example, whereas in high-income countries access to organophosphate containing pesticides are mainly restricted to large-scale farming in low-and-middle income countries these chemicals are more easily accessible to subsistence farmers and are more likely to be kept in homes [2]. A recent study in China found that in 65% of suicides in which pesticides were used had been stored in the home [3]. Most African countries, including the Republic of Botswana, continue to face challenges in the effective prevention and control of pesticide poisoning due to lack of reliable epidemiological data [3]. In developed countries, data can be derived from many different sources, such as coroner’s office, hospital records and poison information centre (PIC) records, as these are considered the most reliable sources of information. However, these are limited by inherent biases and, PICs are nonexistent in most developing countries [3-5]. Episodes of mass poisoning due to organophosphates have been reported in Pakistan and India (25-27). The actual incidence and spectrum of acute poisonings in Botswana are unknown as no studies have been conducted. Attempts to deal with such cases are often sporadic and uncoordinated due to lack of data on which to base firm decisions that may reduce morbidity and mortality from poisoning. Information received from the Botswana Police Service on reported fatal cases of human pesticide poisoning show that methomyl is the most encountered pesticide (Figure 1). A few cases of poisoning by Ethion pesticide have also been reported. The information also reveals that accidental poisoning was reported more commonly than intentional poisoning and that poisonous exposures were more common in adults than children. We report a case of multiple casualties due to ethion pesticide poisoning in Botswana. Even though methomyl pesticide poisoning is the most reported cause of death, this case is unique due the high number of people who died in just one incident when compared to previous methomyl cases where, multiple casualties have never been reported per case (Figure 1).
A local ambulance was dispatched to a rural cattle farming homestead where eight (8) people were reported to be in distress. A family of 8, composed of a 56-year-old male, a 20-year-old male, and 6 children of ages ranging from 2 to 12 years old, allegedly ingested a traditional mixture prepared by the 56-year-old male for sejeso. It was reported to be a colourless clear fluid, the scent of which was reminiscent of burnt drugs. Each member of the family was reported to have ingested approximately 350mL of the fluid. Approximately 10 minutes after the ingestion, all members of the family started experiencing nausea, vomiting, diarrhoea and had a white foamy substance emanating from the nose and mouth, along with extreme weakness. Two of the five children and the 56-yearold male were reportedly certified dead upon arrival at the local clinic while the fourth victim, also a child, demised at the hospital. Clinical notes for the remaining survivors including the 20-yearold male, revealed that they all presented with abdominal pains, nausea, vomiting, diarrhoea, and general body weakness. Further examinations elicited constriction of the pupils, sweating, tearing, and muscle tremor. Electrocardiogram (ECG) showed bradycardia and tall T-waves. The four were all administered with normal saline and atropine and was discharged five days later.
Past medical history was retrieved from outpatient medical records which showed that all affected individuals had an unremarkable background medical history except the 56-yearold victim, who attended the local clinic and reported to have complained of frequent chest pains, cough, and generalised body pains.
Autopsy Findings
The Botswana inquest Act, 1954 mandates that an autopsy for all unnatural, suspicious, and sudden unexpected deaths must be performed. As such, medico-legal autopsies were performed on all four victims. The autopsies performed on the three young victims did not reveal any gross pathological alterations or injuries in all organs. Of note, were the constrictions of the pupils (2mm in diameter), blueish nails, hyper-extensions of the ankle joints and copious froth in the trachea, nasal canals and orifices and covering the infra-nasal areas (Figure 2).
For the 56-year-old male, the autopsy revealed generalised marbling, cataract, hyper-extension of the ankle joints and cyanotic purple livor mortis on external examinations without any injuries. Internal examinations revealed copious froth in the trachea, bilateral hard pleural adhesions which were very difficult to strip using blunt dissections, heavy lungs with the right and left lung weighing approximately 870 grams and 720 grams, respectively. There was marked anthracnosis with peripheral bullaes and both lungs were firm on palpation in both upper lobes. Sectioning of both lungs revealed, upper lobes healed tuberculosis, fibrosis with evidence of chronic obstructive pulmonary disease (COPD), The lower lobes had massive oedema and haemorrhagic pulmonary diseases. There were also patchy mucosal haemorrhages of the oesophageal wall and the stomach (Figure 3). The stomach contents contained approximately 200 mL of a brown fluid. The rest of the organs appeared unremarkable. Other biological samples collected from all deceased persons included blood from the femoral artery, stomach contents, urine, bile, and vomitus. Also sent to the laboratory for analysis was an intensely foul smelling and eye irritating grey powder recovered from the scene. The powder was alleged to be the main ingredient of the ingested mixture (Figure 3).
Toxicology analysis and Results
All samples were extracted using the C18 solid phase extraction (SPE) cartridge. Methanol, acetonitrile, and ethyl acetate were used solvents in that order. The eluent was dried with nitrogen and reconstituted with methanol and analysed with the GC/MS. All post-mortem samples including those of the suspected greyish powder (from the scene) revealed the presence of ethion pesticide. Of note, due to lack of resources, serial plasma cholinesterase and RBC cholinesterase estimates were not performed.
Discussion
We found only a few reports of cases of mass ethion pesticide poisoning resulting in high mortality caused by lung and respiratory disorder. Ethion is a moderately toxic organophosphate belonging to class II category by hazard (27). It is a small (MW 384), lipid-soluble molecule that can be absorbed into the body by inhalation of its aerosol, through the skin and by ingestion (7,8). Absorption is rapid by the oral and dermal routes. In the case we are reporting, all victims were reported to have initially presented with nausea, vomiting, diarrhoea, and general body weakness. These symptoms are consistent with those described in the literature for ingestion and inhalation of ethion pesticide [7-16]. Additional symptoms indicative of severe poisoning with ethion also presented by victims, including excessive production of saliva and mucous, pinpoint pupils, and hyper extension of ankles due to uncoordinated muscle activity, are consistent with those previously reported in the literature [17]. Acute poisoning by ethion and subsequent death resulting from respiratory disorders have also been reported [18, 19]. In our case report, the rapid absorption of ethion can be inferred from the onset of the clinical features which were within approximately 10 minutes after ingestion, and the 3 deaths reported within the first 3 hours. Interestingly, the youngest 3 deaths and oldest (56 years old) occurred within 6 hours; this can be due to large exposure considering the body weight of the children and for the adult, comorbidities could have also aggravated the effects of ethion. It is of note that the hyper extension of ankles, which was observed in all the four victims, has never been reported in all the literature we reviewed. Therefore, we report it as a new finding for ethion poisoning.
The bluish fingertip and nail discolouration observed in all victims indicated that they may have experienced low oxygen levels and acute failure of the lungs, and as a result died. Respiration disorders are a consequence of bronchoconstriction and hypersecretion of mucus in the bronchi consequent to the muscarinic effect [19]. Atropine is normally used to treat victims of organophosphate poisoning [20-24]. In this case, all survivors reacted well to the treatment, which supports that the victims were likely to have been poisoned with ethion pesticide. The cause of death for all victims was ruled as the ingestion and subsequent poisoning with ethion pesticide. There was no evidence of suicidal intent associated with pesticide ingestion.
Conclusion
We presented a case of ethion organophosphate poisoning in rural Botswana. Unlike in other reports the poisoning was because of herbal medication ingestion. It is unclear how the family accessed the ethion. This case in which four lives were lost add to the literature advocating for tighter control of organophosphates in LMICs such as Botswana.
Recommendations
This case and other worldwide studies present strong evidence that acute pesticide poisoning is a global public health challenge. There is need to improve public education regarding the safe use, safekeeping, and possible poisoning by pesticides to avoid loss of human lives. All these may be achieved through media campaigns, and clear labelling of product containers to reduce risks. Developing countries need to devise measures to restrict the availability of pesticides by either banning, requiring licences for use or prescriptions, or through the promotion of practices that minimize their use. Above all, developing countries need to establish their own National Poison Centres, and build national pesticide poisoning databases. These would help in the monitoring and management of epidemiology and risk factors of pesticide poisoning.
Acknowledgements
This work was supported by the Botswana International University of Science and Technology. We would like to thank the Botswana Police Forensic Pathology North Branch for their support and input.
We would also like to show our gratitude to Dr Janes Mokgadi, a forensic scientist in the Chemical, Biological, Nuclear and Radiological Weapon Management Authority, Ministry of Defense, Justice and Security, Botswana, and Sara Solomon, MPH, RD, Deputy Director, Penn Injury Science Center (PISC) of University of Pennsylvania for their comments on an earlier version of the manuscript. Any errors in the manuscript are our own and should not tarnish the reputations of this esteemed individual.
Conflict of Interest
The authors declare that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Credit Author Statement
Gothatamang Norma Phokedi: Conceptualisation, Visualisation, Resources, Funding acquisition, Investigation, Writing - Original draft preparation, Writing- Reviewing and Editing, Supervision
Shathani Mugoma: Conceptualisation, Visualisation, Resources, Funding acquisition, Investigation, Writing - Original draft preparation, Reviewing and Editing, Supervision
Dr Patlakwe: Conceptualisation, Visualisation, Resources, Investigation, Editing
Mmaabo Tsenang: reviewing and editing
References
- (2016) World Health Organization & Food and Agriculture Organization of the United Nations., 2016. International code of conduct on pesticide management: guidelines on highly hazardous pesticides.
- Gunnell D, Eddleston M (2003) Suicide by intentional ingestion of pesticides: a continuing tragedy in developing countries. International Journal of Epidemiology 32(6): 902-909.
- Veale D, Wium C, Müller G (2012) Toxicovigilance I: A survey of acute poisoning in South Africa based on Tygerberg Poison Information Centre data. S Afr Med J 103(5): 293-297.
- Hoffman RS (2006) Poison information centres and poison epidemiology. In: Flomenbaum NE, Goldfrank LR Hoffman RS, Howland MA, Lewin N, Nelson L, Eds. GoldfTank's Toxicologic Emergencies. 8th Edn. New York: McGraw-Hill, 2006:1826-1828.
- Kamaruzaman NA, Leong YH, Jaafar MH, Mohamed Khan HR, Abdul Rani NA, et al. (2020) Epidemiology and risk factors of pesticide poisoning in Malaysia: a retrospective analysis by the National Poison Centre (NPC) from 2006 to 2015. BMJ open 10(6): e036048.
- (1989) Pesticide factsheet number 209: Ethion. Office of pesticides and toxic substances. EPA (U.S. Environmental Protection Agency) pp. 5-64.
- (2019) Pocket Guide to Chemical Hazards CAS No. 563-12-2: Ethion. CDC- NIOSH Pocket Guide to Chemical Hazards - Ethion. National Institute for Occupational Safety and Health.
- (2021) PubChem Compound Summary for CID 3286, Ethion. National Center for Biotechnology Information.
- Smulders CJ, Bueters TJ, Vailati S, van Kleef RG, Vijverberg H P (2004) Block of neuronal nicotinic acetylcholine receptors by organophosphate insecticides. Toxicol Sci 82(2): 545-554.
- (1986) Organophosphorus Insecticides a General Introduction. Geneva: World Health Organization (WHO). Metabolism and mode of action pp. 39-48.
- Adeyinka A, Kondamudi NP (2021) Cholinergic Crisis. In StatPearls.
- Colović MB, Krstić DZ, Lazarević Pašti TD, Bondžić AM, Vasić VM (2013) Acetylcholinesterase inhibitors: pharmacology and toxicology. Curr Neuropharmacol 11(3): 315-335.
- (1986) In: Organophosphorus Insecticides a General Introduction. Geneva: World Health Organization (WHO). Effects of organophosphorus insecticides on the nervous system pp. 58-69.
- Aldridge W, Reiner E (1975) Enzyme inhibitors as substrates: Interactions of esterases with esters of organophosphorus and carbamic acids. Amsterdam; Oxford: North-Holland.
- Costa L (2006) Current issues in organophosphate toxicology. Clin Chim Acta 366(1-2): 1-13.
- Dewan A, Patel AB, Pal RR., Jani UJ, Singel VC (2008) Mass ethion poisoning with high mortality. Clin Toxicol (Phila) 46(1): 85-88.
- Mishra A (2012) Epidemiological Study of Medicolegal Organophosphorus Poisoning in Central Region of Nepal. Journal of Forensic Research 03(09).
- Mlayeh S, Annabi K, Daly A, Jedidi M, Dhiab M (2020) Pesticide poisoning deaths: a 19-year retrospective study of medicolegal autopsies in Centre Tunisia. Egyptian Journal of Forensic Sciences 10(1).
- Mostafalou S, Abdollahi M (2016) Pesticides: an update of human exposure and toxicity. Arch Toxicol 91: 549-599.
- Robenshtok E, Luria S, Tashma Z, Hourvitz A (2002) Adverse reaction to atropine and the treatment of organophosphate intoxication. Isr Med Assoc J 4(7): 535-539.
- Bowls BJ, Freeman JM, Jr Luna JA, Meggs WJ (2003) Oral treatment of organophosphate poisoning in mice. Acad Emerg Med 10(3): 286-288.
- Joy M. Radhakrishnan B. Sekar M, David S (2019) Organophosphate poisoning: Overview, management, and nursing care. Indian Journal of Continuing Nursing Education 20(2): 131.
- Eddleston M, Chowdhury F (2015) Pharmacological treatment of organophosphorus insecticide poisoning: the old and the (possible) new. Br J Clin Pharmacol 81(3): 462-470.
- Kartz K (2020) Organophosphate Toxicity Medication: Anticholinergic agents, Antidotes, Organophosphate poisoning, Benzodiazepines.





 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.