Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Ormond’s Disease; Management Dilemma
*Corresponding author: Farrahin Sazale, Department of Surgery, Hospital Segamat, KM 6 Jalan Genuang, Segamat, Johor, Malaysia.
Received: February 02, 2022; Published: February 09, 2022
DOI: 10.34297/AJBSR.2022.15.002119
Abstract
Background: Retroperitoneal fibrosis (RPF) or Ormond’s disease is a rare and extensive fibroinflammatory condition of unknown cause involving the abdominal aorta, iliac arteries, ureters and inferior vena cava with infiltration to the surrounding structure.
Case Report: We report a case of an extensive benign retroperitoneal fibrosis (RPF) in a 62-year-old lady with the mass encasing abdominal aorta, common iliac, and inferior vena cava. There is a medialization and thickening of bilateral ureter causing obstructive uropathy. Patient was given a tapering dose of glucocorticoid treatment for three consecutive months. Percutaneous nephrostomy was constructed only for the left kidney. Repeated scan showed regression of the fibrosis with improvement of uropathy. The purpose of this case report is to highlight on the treatment approach of idiopathic RPF and to summarize the relevant literature.
Conclusion: To date, there is no established guideline for the management of idiopathic retroperitoneal fibrosis. The treatment of idiopathic RPF has been a debate since the past decades. There is still a lack of understanding of this rare condition and most reviews are of level I evidence which include case reports, small series, and retrospective studies.
Keywords: Ormond’s disease; obstructive uropathy; retroperitoneal fibrosis; surgery; hemorrhage
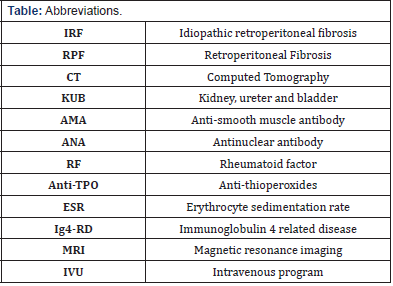
Abbreviations: IRF - Idiopathic retroperitoneal fibrosis; RPF- retroperitoneal fibrosis; CT - computed tomography; KUB - kidney, ureter and bladder; AMA - anti-smooth muscle antibody; ANA - antinuclear antibody; RF - rheumatoid factor; Anti-TPO - antithioperoxides; ESR - erythrocyte sedimentation rate; Ig4-RD - immunoglobulin 4 related disease; MRI - magnetic resonance imaging; IVU - intravenous program
Introduction
Retroperitoneal fibrosis (RPF) is a rare and extensive fibroinflammatory condition involving the abdominal aorta, iliac arteries and inferior vena cava with infiltration to the surrounding structure. To our knowledge, there is no established international consensus for diagnosing and managing RPF. The ultimate goal of treatment for retroperitoneal fibrosis is to preserve good renal function by relieving ureteral obstruction and reducing the size of the mass, as well as to prevent recurrence. It is important to determine the cause of RPF as the treatment options vary according to the disease. This report focused on the treatment planning of idiopathic retroperitoneal fibrosis (IRF).
Case Presentation
A 62-year-old lady with underlying hypertension went for her routine follow up and incidentally noted increasing serum creatinine level. Throughout the year, the patient claimed that she had frequent urination up to eight times each day and the urine appeared frothy than usual. Previously, she urinated about three to four times a day. She denies experiencing abdominal discomfort or pain. On examination, her abdomen is soft and scaphoid. There is no palpable mass. The renal profile shows elevated creatinine level from 87 pmol/L to 199 pmol/L over a few months. An ultrasound of kidney-ureter-bladder (KUB) revealed the presence of bilateral moderate to severe obstructive uropathy which was worse on the right. No echogenic renal calculus seen and was unable to visualize the entire bilateral ureter in the ultrasound. Subsequently, a nonenhanced computed tomography (CT) urography performed revealed irregular iso-attenuating soft tissue density encasing the aorta (Figure 1). Hence, proceeded with a contrast CT abdomen.

Figure 1: The Retroperitoneal Mass Is Seen to Encase the Distal Inferior Vena Cava Before the Bifurcation And Slightly Compressing Onto It.
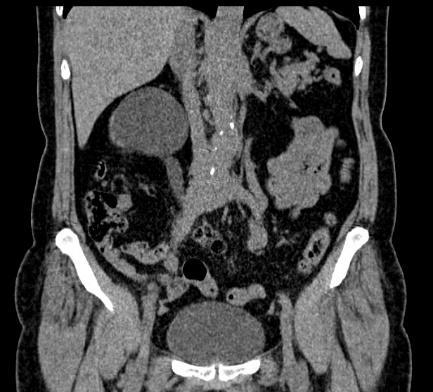
The contrasted study showed homogeneously enhancing periaortic soft tissue density iso-attenuating with the muscle. It is seen encasing the aorta from the level L1/L2 extending to the bifurcation of aorta, extending to the right common iliac, internal and the proximal external iliac arteries. Distally, the mass is also seen encasing the inferior vena cava extending to the right common iliac vein with loss of the plane of demarcation in between. There is also involvement of the middle third of bilateral ureters with associated medialization of the ureters (Figure2). The mass has caused obstruction of bilateral ureters evident by the gross hydronephrosis and hydroureter on the right side as well as mild left sided hydronephrosis and dilated proximal left ureter. We referred the case to the medical team for further evaluation and treatment. Rheumatological blood workup including immunoglobulin assay showed normal results. In addition, all the connective tissue tests including anti-smooth muscle antibody (AMA), antinuclear antibody (ANA), rheumatoid factor (RF), C3, C4, p-ANCA, c-ANCA, anti-thioperoxides (TPO), and serum protein electrophoresis are negative. Erythrocyte sedimentation rate (ESR) is seen raised twofold from the normal limit (Figure3).
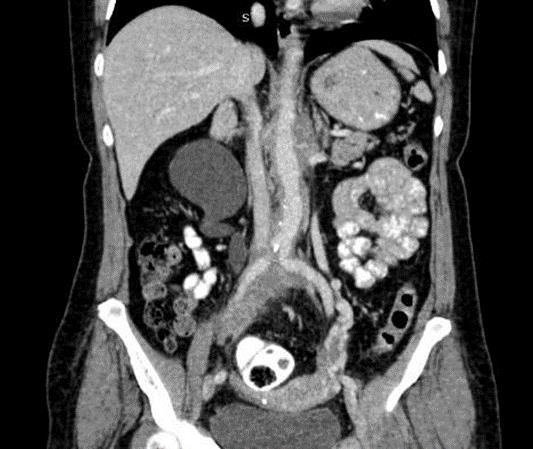
Figure 2B: Contrasted Coronal CT With the Mass Seen Encasing the Right Ureter Causing Right Gross Hydronephrosis and Hydroureter.
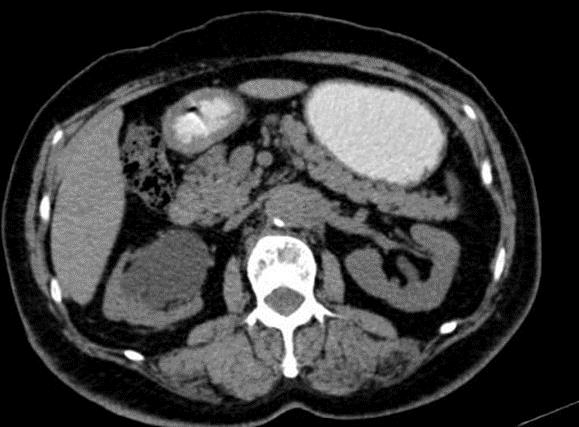
Figure 3: The Retroperitoneal Mass Is Seen to Encase the Distal Inferior Vena Cava Before the Bifurcation And Slightly Compressing Onto It.
Patient was treated with immunosuppression using oral prednisolone over a course of 3 months. The initial dose given was 30 mg daily for one month, then 20 mg daily for the next month and 10 mg daily in the third month, which was gradually tapered. Following therapy, we conducted an abdominal CT to reassess the size of the mass and ureteral obstruction. The mass seemed smaller than it had been. The length of the measurement has been shortened to 13.3 cm along the aorta and 5.5 cm along the right iliac arteries. Additionally, we observed a decrease in the degree of the right hydronephrosis and right renal pelvis dilatation. As a result, the percutaneous nephrostomy was only performed on the left kidney to treat the hydroureteronephrosis. We follow up the patient in the outpatient department to look at her progress of renal function and overall condition.
Discussion
Ormond’s disease or commonly known as retroperitoneal fibrosis (RPF) is a rare fibroinflammatory disease that develops around the abdominal aorta, iliac arteries, vena cava and surrounding retroperitoneal structures. The pathogenesis of RPF involved chronic inflammation, fibroblast proliferation, and extracellular matrix deposition in the retroperitoneum. In 1948, John Ormond was first to postulate that the presence of retroperitoneal inflammation would cause bilateral ureteral obstruction and it is described as an independent clinical entity. [1] Hence, RPF is known as Ormond’s disease. Other names given include periarteritis fibrosa, plastic periarteritis, chronic periarteritis, sclerosing retroperitoneal granuloma, and fibrous retro peritonitis. The etiology of RPF is unknown, but it has many causes, including infection, radiation, drugs, malignant tumor, and trauma. In the last decade, an autoimmune mechanism involving infiltration of IgG4-positive plasma cells has been considered to be a possible cause of idiopathic RPF. Although IgG4 related disease (IgG4-RD) is known to have a multiorgan involvement, there are cases reported as IgG4 unrelated idiopathic RPF with only single organ affected. [quotes] In the literature, despite having classical histopathological and immunochemical findings, about 30% patients were reported to exhibit normal serum IgG4 levels. [2] RPF is usually found incidentally from computed tomography (CT), magnetic resonance imaging (MRI) and intravenous urography (IVU) while investigating for causes of obstructive neuropathy or renal failure. Lali et. al reported that about 87% of patients with retroperitoneal fibrosis have developed obstructive uropathy during their early presentation. [3] Features of RPF that are suggestive of malignancy may warrant biopsy to aid in providing the patient with the most appropriate and effective treatment. Anterior displacement of the aorta and IVC is more likely suggestive of a malignant entity. They frequently caused lateral ureteral deviation rather than medial. [4] Other features include evidence of local bone destruction and large bulky lesions. The presence of sub centimeter reactive lymphadenopathy is more related to a benign RPF. [5] In our present case, the CT findings are suggestive towards benign RPF. We could not undertake a biopsy to further confirm our diagnosis due to technical limitations in the hospital. Furthermore, in view of its anatomical location, it is very risky to biopsy as the tissue is close to the aorta. Treatment of idiopathic RPF aims at relieving ureteral obstruction and inducing the regression of fibrosis. This includes the use of glucocorticoids, combined with or without immunosuppressant drugs with concomitant urological procedures such as ureterolysis or nephrostomy. In case of chronic presentation complicated with end stage renal failure, options of treatment may include open surgery or renal auto transplant. Based on standard protocol, prednisolone is given at 40-60 mg/d tapered to 10 mg/d within 2-3 months and discontinued after 12-24 months. The first treatment algorithm was introduced in 2006 by Vagile et. al. who suggested that a stent or nephrostomy be constructed first prior to commencing corticosteroid treatment.[6] Later in 2018, an updated algorithm by Biryani et. al emphasized on looking at the degree of hydronephrosis before predisposing the patient to risks and complications of urological procedure or surgery.[7] Ruya et. al reported a complete resolution of mild hydronephrosis post steroid therapy for idiopathic RPF and recommended the treatment to begin earlier as to avoid complications such as renal dysfunction. [8] For moderate to severe hydronephrosis, it is preferable to do surgical intervention at an early phase. Several treatment options have been described in the literature. In 1987, Downey et. al reported that the use of percutaneous balloon dilatation for ureteral blockage in idiopathic RPF resulted in a long-term occlusion alleviation.[9] A prospective analysis conducted in the United Kingdom showed that about 94-96% of patients with ureteric obstruction secondary to RPF, became stent- or nephrostomy-free following open ureterolysis. [10] Although effective, open definitive surgical management for RPF carries a significant morbidity and even mortality burden. Common complications of open ureterolysis include prolonged ileus, surgical site infection, urinary tract infection, deep-venous thrombosis, pulmonary embolism, prolonged urine leakage, and glomerulonephritis. Hamad et al reported the first case of ureteral intraperitonealization which eventually complicated with bilateral hydronephrosis and hydroureter. The renal function became normal after being treated with steroids and a right nephrostomy tube. [11].
In the current era, robotic laparoscopic ureterolysis is considered to be the most appealing alternative. The first successful case of robotic ureterolysis and laparoscopic omental ureteral wrapping was reported in 2006 by Patrick et. al. The outcomes were compared with previous Fujita and Brown laparoscopic series and showed reduction in operative time, estimated blood loss, and length of hospital stay.[12] The RPF in our patient regressed following steroid therapy which was given 3 months before placing the percutaneous nephrostomy. Although the treatment given does not exactly follow the current standard, it renders our patient from having bilateral ureteral drainage. Generally, in idiopathic RPF causing ureteral obstruction, a good outcome for renal function is expected, although long-term steroid therapy along with urinary drainage is often required. Patients with idiopathic RPF need an eternity follow up as the disease may relapse and even be life threatening to the patient. A routine renal profile and ultrasound imaging may be adequate to assess disease progression during clinic visit.
Conclusion
RPF has low prevalence but high morbidity. The establishment of a concise and systematic approach to management of idiopathic retroperitoneal fibrosis by experienced experts in the field is of great desire. It is crucial for all physicians to be able to identify this rare entity and provide the best management for the patients.
Acknowledgements
We would like to thank Dr Lee SZ and Dr Yamuna Devi for providing us with the best quality image of the radiological findings for the case report.
Conflict of Interest
The author declares that no conflict of interest exists.
References
- Ormond JK (1948) Bilateral ureteral obstruction due to envelopment and compression by an inflammatory retroperitoneal process. J Urol 59(6): 1072–1079.
- Niaz A, Ahmad AH, Khaleeq-ur-Rahman, Saeed MA, Sabir O, et al. (2016) IgG4-related retroperitoneal fibrosis: A case report and review of literature. J Pak Med Assoc 66(2): 220–222.
- Lalli AF (1977) Retroperitoneal fibrosis and inapparent obstructive uropathy. Radiology 122(2): 339-342.
- Umehara H, Okazaki K, Masaki Y, Mitsuhiro Kawano, Motohisa Yamamoto, et al. (2012) A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol 22(1): 1-14.
- Van Bommel EFH, Jansen I, Hendriksz TR, Aarnoudse A L H J (2009) Idiopathic retroperitoneal fibrosis: prospective evaluation of incidence and clinicoradiologic presentation. Medicine (Baltimore) 88(4): 193-201.
- Vaglio A, Maritati F (2016) Idiopathic Retroperitoneal Fibrosis. J Am Soc Nephrol 27(7): 1880-1889.
- Biyani CS (2016) Retroperitoneal Fibrosis. Medscape Reference.
- Watanabe R, Ozawa A, Iseda T (2017) A case of retroperitoneal fibrosis responding to steroid therapy. Int Braz J Urol 43(6): 1185-1189.
- Downey DB, O'Connell D, Smith J, et al. (1987) Percutaneous balloon dilatation of a mid-ureteric obstruction caused by retroperitoneal fibrosis. Br J Urol 60(1): 84-85.
- O'Brien T, Fernando A (2017) Contemporary role of ureterolysis in retroperitoneal fibrosis: treatment of last resort or first intent? An analysis of 50 cases. BJU Int 120(4): 556-561.
- Hamad J, Monzer M, Bruce P, et al. (1994) Ureteral Encasement and Medial Deviation Demonstrated by Ultrasound in a Case of Retroperitoneal Fibrosis. Journal of Diagnostic Medical Sonography 10(4): 213-216
- Mufarrij PW, Stifelman MD (2006) Robotic ureterolysis, retroperitoneal biopsy, and omental wrap for the treatment of ureteral obstruction due to idiopathic retroperitoneal fibrosis. Rev Urol 8(4): 226-230.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.