Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Percutaneous Coronary Intervention for Left Main Stem Restenosis in a Patient with Tetralogy of Fallot after Bovine Pericardium Angioplasty: A Case Report
*Corresponding author: Wenzhong Zhang, The Affiliated Hospital of Qingdao University, China.
Received: January 10, 2022; Published: January 21, 2022
DOI: 10.34297/AJBSR.2022.15.002105
Abstract
Owing to the drug-eluting stents, percutaneous coronary intervention has become an increasingly acceptable treatment for patients with left main coronary artery disease. Rare reports of placing a drug-eluting stent in restenosis vassal which is made by bovine pericardium after surgical angioplasty have been described. We report a patient who performed operation due to Fallot, this patient’s left main coronary was injured accidentally during the operation. To rebuild left main coronary, we chose surgical angioplasty and bovine pericardium was chosen as patch. However, postoperative coronary angiography suggested restenosis of artificial left main coronary artery. We placed a drug-eluting stent in this stenosis successfully. Thus, this case demonstrates that placing drug-eluting stents in restenosis vassals which are made by bovine pericardium is feasible.
Keywords: Drug-eluting stents, Percutaneous coronary intervention, Pericardium, Angioplasty
Abbreviations: LMCAD: Left Main Coronary Artery Disease; CABG: Coronary Artery Bypass Grafting; PCI: Percutaneous Coronary Intervention; SA-LMCA: Surgical Angioplasty of the Left Main Coronary Artery; CAD: Coronary Artery Disease.
Introduction
Owing to the dominance of the left coronary circulation, left main coronary artery disease (LMCAD) usually predicts higher prognostic risk [1]. At present, the revascularization of LMCAD mainly includes coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI) and surgical angioplasty of the left main coronary artery (SA-LMCA). Contrasted with the well-documented CABG and PCI, the long-term results of SA-LMCA have rarely been reported [2]. Moreover, case reports concerning placing drug-eluting stents in restenosis vassals after surgical angioplasty are even less. This paper reports a successful case of PCI of a left main coronary bovine pericardial sheet for restenosis after Fallot tetralogy.
Case report
A 28-year-old female with tetralogy of Fallot presented with chest tightness despite accepted radical operation for tetralogy of Fallot. At age 5, she was diagnosed with tetralogy of Fallot and accepted radical operation for tetralogy of Fallot. However, one month ago, she developed crescendo chest tightness. Given that her syndrome had worsened in severity, the clinical concern was of failure of radical operation for tetralogy of Fallot.
Transthoracic echocardiography showed a left ventricular ejection fraction of 60%, and mitral valve, tricuspid valve, and pulmonary valve all have moderate to severe regurgitation. Following a multidisciplinary team dissociate patient was considered an appropriate candidate for surgery. Subsequently, this patient underwent surgery including mitral valvuloplasty, tricuspid valvuloplasty, pulmonary valvuloplasty and right ventricular outflow tract stenosis dredging. During the operation, severe adhesions around the heart were seen and left main coronary artery runs on the anterior wall of the right ventricular outflow tract and crosses the right ventricular outflow tract. To broaden the outflow better, we transected the LM. After that, to rebuild the Left Main Coronary, a 1cm×2cm Bovine Pericardium was temporarily rolled into a tubular structure and was anastomosed with the Left Coronary Artery at both broken ends. The result of intraoperative blood flow measurement was satisfactory.
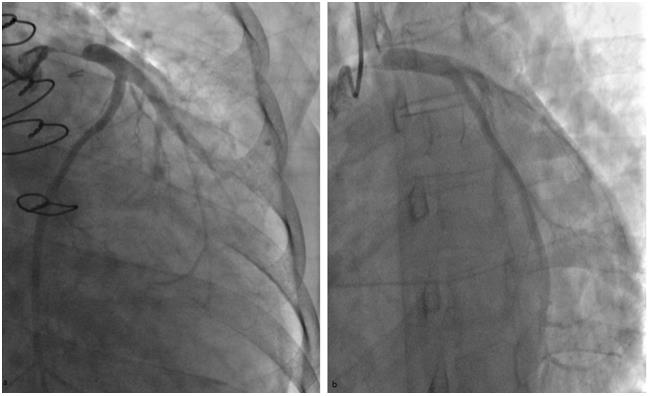
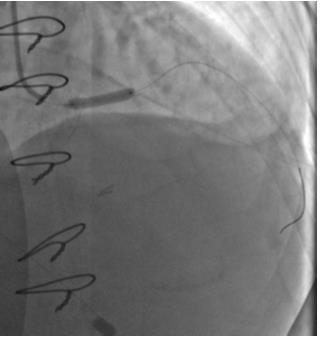
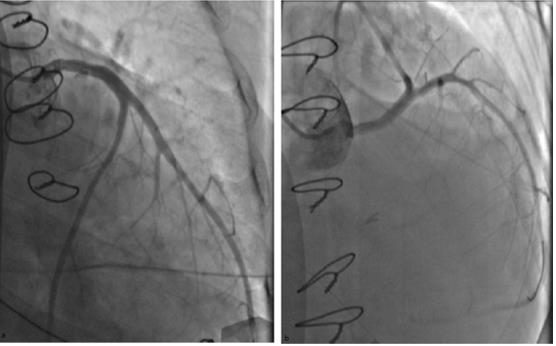
However, three months late, she was readmitted to the hospital because of chest pain. During the hospitalization, the patient experienced ventricular fibrillation and Asthma episodes repeatedly. Because of the possible restenosis of the artificial aorta, Coronary Angiography was performed with the assistance of IABP. The Coronary Angiography results demonstrated 99% of Left Main Coronary Artery Stenosis (Figure 1a, b). Accordingly, we decided to carry out the PCI in this narrow spot. A 2.5×15mm compliant balloon was used to pre-expand the stenosis, and a 4.0 × 20mm drug-eluting stent was placed (Figure 2). And a 4.5×20mm NC TREK non-compliant balloon was applied to expand the residual stenosis, and the residual stenosis was <10% (Figure 3a, b). After the PCI, the patient’s chest pain was gradually relieved. With Clopidogrel and Aspirin dual antiplatelet the patient’s condition gradually stabilized. However, the patient suffered from sudden upper gastrointestinal bleeding. With a series of treatments such as somatostatin, PPI, blood transfusion etc., the patient’s condition became stable. However, her family decided to stop treatment and asked for against-advice discharge. Unfortunately, we lost contact with the patient after she was discharged.
Discussion
Coronary artery disease (CAD) is mostly caused by single or multiple atherosclerotic plaques that block the coronary arteries and cause a decrease in coronary blood flow. Usually, it leads to angina pectoris and ischemic myocardial ischemia, and more seriously, it can cause myocardial infarction. Patients with evidence of moderate-to-severe coronary ischemia present an annual rate of 4%-6% risk of cardiogenic death or non-fatal myocardial infarction, and hence, coronary revascularization is necessary for such patients [3]. Owing to the dominance of the left coronary circulation, LMCAD predicts higher prognostic risks. Current clinical practice guidelines from both the American College of Cardiology/American Heart Association and the European Society of Cardiology recommend revascularizations for all patients with ≧50% stenosis of the left main coronary artery (LM) regardless of symptomatic status or associated ischemic [4].
The revascularization of the LM includes CABG, PCI and SALMCA. SA-LMCA has been advocated for years to be applied to restore the physiologic flow of LM. Compared with CABG, SA-LMCA aims to restore more physiologic flow of LM. In addition, it wouldn’t interfere with the vessels for PCI later. Although there are relatively few data about long-term outcome in these patients, a study indicates most of these patients show an excellent anatomic and physiologic result after direct surgical angioplasty of the left main coronary artery [5].
The choice of the patch material is the most important issue to prevent acute thrombosis and restenosis of the LMCA. At present, internal mammary artery, saphenous vein, and bovine pericardium are commonly used in surgical angioplasty. Bovine pericardium enjoys the advantage of reliable consistency, satisfactory biocompatibility, and ease of handling. Also, it has the reliable strength to allow a tight-fitting closure, which yields less suture line bleeding and prevents aneurysmal dilatation [6]. On the other hand, bovine pericardium heralds the possibility of restenosis, even though a study reports a low incidence of restenosis over 12 in patient who underwent CEA with bovine pericardial patch angioplasty [7]. The main cause of restenosis is related with intimal hyperplasia in the area at or near the bovine pericardial patch. However, the fundamental molecular and cellular mechanisms is still unclear.
As the most widely used method for CAD, PCI has undergone continuous improvement over the past few decades, especially with the advent of drug-eluting stents. Drug-eluting stents can inhibit the formation of vascular neointimal tissues by releasing anti-angiogenic drugs (such as rapamycin), significantly reducing the occurrence of intravascular restenosis (ISR). Owing to the drugeluting stents, PCI becomes an increasingly acceptable treatment for patients with LMCAD. A study indicates that there is no significant difference between PCI and CABG in patients with LMCAD of low or intermediate anatomical complexity [8].
For this patient, the left main coronary artery is accidentally injured, the consideration about graft in the young patient and the intention to restore more physiologic flow steer us away from CABG. Instead, we choose SA-LMCA to rebuild the LM. As for the patch materials, we are unable to resort to the internal mammary artery and autologous pericardium as a patch material because the patient’s previous surgery has caused adhesions around the heart. Moreover, considering that the patient’s cardiac arrest is too long, choosing saphenous vein as patch would have prolonged the operation time and increased the unnecessary surgical risk. Consequently, bovine pericardium with good biocompatibility is chosen as the patch. However, the postoperative coronary angiography suggests restenosis of the artificial left main coronary artery. Finally, we place a drug-eluting stent in the stenosis of left main coronary. Chest pain and other symptoms are relieved significantly after PCI, and no malignant events such as ventricular fibrillation occur, which prove that this treatment scheme is effective and worthy of clinical reference.
Acknowledgements
We wish to thank all participants and investigators for their involvement.
Disclosure of interest
The authors report no conflict of interest.
References
- Ramadan R, Boden WE, Kinlay S (2018) Management of Left Main Coronary Artery Disease. J Am Heart Assoc 7(7): e008151.
- Jeong JH, Lee WY, Kim EJ, Cho SW, Kim KI, et al. (2015) Long-term results of surgical angioplasty for left main coronary artery stenosis: 18-year follow-up. J Cardiothorac Surg 10: 6.
- Shaw LJ, Berman DS, Picard MH, Matthias GF, Raymond YK, et al. (2014) Comparative definitions for moderate-severe ischemia in stress nuclear, echocardiography, and magnetic resonance imaging. JACC Cardiovasc Imaging 7(6): 593-604.
- Levine GN, Bates ER, Blankenship JC, Steven RB, John AB, et al. (2012) 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv 79(3): 453-495.
- Botman CJ, Arnoudse W, Penn O, Pijls N (2006) Long-term outcome after surgical left main coronary angioplasty. Annals Thorac Surg 81(3): 828-834.
- Li X, Guo Y, Ziegler KR, Model LS, Sammy DDE, et al. (2011) Current usage and future directions for the bovine pericardial patch. Ann Vasc Surg 25(4): 561-568.
- Papakostas JC, Avgos S, Arnaoutoglou E, Christos N, Michalis P, et al. (2014) Use of the vascu-guard bovine pericardium patch for arteriotomy closure in carotid endarterectomy. Early and long-term results. Ann Vasc Surg 28(5): 1213-1218.
- Stone GW, Kappetein AP, Sabik JF, Stuart JP, Marie CM, et al. (2019) Five-Year Outcomes after PCI or CABG for Left Main Coronary Disease. N Engl J Med 381(19): 1820-1830.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.