Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Primary Chronic Osteomyelitis of the Mandible: A 10 -Year Follow- Up
*Corresponding author: Touil D Jelassi K, Department of Dental, University of Monastir, Tunisia.
Received: December 06, 2021; Published: December 09, 2021
DOI: 10.34297/AJBSR.2021.15.002068
Abstract
The aim of this paper was to report the case of a healthy female patient with a 10- year- history of primitive chronic osteomyelitis of the mandible diagnosed at the age of 13. Clinical and radiographic features were reported. Treatment modalities were discussed.
Keywords: Osteomyelitis; Chronic; Mandible; Decortication; Hyperbaric Oxygen Therapy
Introduction
Primary chronic osteomyelitis of the jaw (PCO) is a nonsuppurative chronic inflammatory disease of the jawbone affecting mostly the mandible [1]. Its etiology remains unclear. This condition can be either isolated or related to other diseases, such as autoimmune diseases and syndromes, including SAPHO syndrome (synovitis, acne, pus Blister, bone hyperplasia, and osteitis)”, as well as Majeed syndrome or cherubism [1,2]. This condition is mainly seen in young adults, affecting both males and females [3]. Secondary chronic osteomyelitis of the jaw (SCO) is usually caused by bacterial infection of known origin, such as tooth extraction or pulp infection. It is much more common than PCO. However, diagnosis of primary chronic osteomyelitis is often challenging. It is often made based upon the clinical findings, including chronic swelling of the jaw, severe pain, and severe restriction of the mouth opening with no evidence of local infection, trauma or neoplasm [4]. Panoramic radiograph often reveals the presence of osteolytic radiolucent areas, combined with increased thickness of the alveolar lamina dura, and sclerogenic variation of the bone in the affected area and around the mandibular canal [5]. Computed tomography patterns of osteomyelitis can be lytic, mixed or sclerotic. However, sequestrum patterns are rare. Bacterial contamination of bone tissue is best determined by bone biopsy under radiographic guide [6]. The most frequently involved bacteria are Staphylococcus aureus, Gram negatives (Pseudomonas aeruginosa), and anaerobe bacteria (Bacteroides fragilis). Bone scintigraphy is highly sensitive to bone abnormalities. It is a useful method, especially in young patients with suspected inflammatory disease or malignant tumors [7]. Magnetic resonance imaging has many advantages thanks to its ability to detect early changes related to osteomyelitis, to evaluate the true extent of the disease, to depict extraosseous spread of the infection, and to help guide surgical management [8]. Treatment of this condition remains controversial, and it is often based on anti- inflammatory drug therapy such as corticosteroids, nonsteroidal anti- inflammatory drugs (NSAIDs), long term antibiotics, hyperbaric oxygenation (HBO), and more recently Biphosphonates therapy [9]. Surgical management is sometimes required, and it generally consists in decortication. However, in some severe cases, resection of the unhealthy bone remains the only therapeutic solution [10]. Thus, this condition is known as being debilitating and difficult to manage, thus having a severe impact on patient’s quality of life. Recurrence is common and it is reported even many years after the first onset [3]. We herein report the case of a healthy female young patient with a 10-year chronic primitive osteomyelitis of the mandible. The clinical and radiological findings as well as the disease evolution throughout the years are also reported. Treatment modalities are discussed.
Case Presentation
A 24-year-old healthy female patient was referred to the department of oral surgery and oral medicine by her endodontist for a severe limitation of her mouth opening which makes the conservative treatment of the tooth 36 impossible. The patient reported a history of primitive chronic osteomyelitis (PCO) of the left mandible that was diagnosed at the age of 13 years. According to the patient’s medical files, the history of the condition started when the patient was referred by her orthodontist to an oral surgeon for an “abnormal swelling of her left jaw and severe pain”. Panoramic radiograph showed an abnormal bone density of the mandible with small multiple lytic lesions in the left corpus and the area of the germ of the tooth 38 (Figure 1). Computed Tomography showed a heterogeneous pattern with expansion of the left ascending and angulo-mandibular ramus, sclerosis foci, and erosion of the adjacent cortical bone. Surgical curettage of the lesion and extraction of the germ 38 were performed.

Figure 1: The first panoramic radiograph of the patient taken at the age of 13 showing abnormal bone density of the mandible with small multiple lytic lesions in the left corpus and the area of the germ of the tooth 38.
Histological examination predominantly showed chronic inflammatory infiltration and medullary fibrosis. Based on the findings, diagnosis of primary chronic osteomyelitis of the mandible had been made. Complementary scintigraphy was indicated to search any possible extra-oral lesions. No other scintigraphic abnormality of radiotracer fixation on the rest of the osteoarticular system was revealed. Thus, diagnosis of recurrent multifocal osteomyelitis was ruled out (Figure 2). Follow-up was marked with pain, swelling, and mouth opening limitation despite medication including non-steroidal anti-inflammatory drugs: Iboprofen 400mg (twice a day), levofloxacin (Tavanic 500 3 times/day), and paracetamol (Panadol 3g/day). A second surgical intervention was indicated12 months later because of the persistence of symptomatology, especially pain and trismus. The patient underwent decortication of the mandible (the corpus). Pharmaceutical management was based on anti-inflammatory drugs (Iboprofen 500mg), antibiotics: Clindamycin (Dalacine 600mg 2 tab 3 times / day), Levofloxacin (Tavanic 500mg twice a day) and Paracetamol (1g 3 times a day). The patient also received 40 HBO sessions. The patient reported an improvement marked with a decrease in pain and mouth opening restriction despite the persistence of a small and firm swelling of her left mandibular angle and the occasional onset of mild pain that was efficiently relieved with paracetamol. The consultation day, extra-oral examination revealed a firm swelling of the patient’s left jaw extending to the mandibular as well as the temporal areas. Mild pain was present at palpation. The patient had a severe limitation of the mouth opening (1cm). Intra-oral examination revealed a deformation of the corpus in both the vestibular and lingual sides, with gingival fibrosis (Figure 3). Computed tomography showed diffuse sclerosis and an important thickening of the mandibular bone extending to the homolateral condyle. The emergence of the mandibular canal was also involved. Muscular hypertrophy of the masseter muscle and the lateral pterygoidien muscle were evident, too (Figure 4a & 4b). The 3D reconstruction revealed with great precision the extent of the lesion involving the entire left mandible. (Figure 4c). Moreover, periapical radiolucent images were noticeable on the teeth 37 and 36 with evidence of root resorption. Vitality tests on the teeth 36 and 37 were negative.
Given the severity of the condition, steroids injections (prednisone 8mg 1inj/d for five days), Antibiotics (Dalacine 600mg, 2.4g/day) and paracetamol (Doliprane1g, 4g/day) were prescribed. Ten days later, the patient reported a significant improvement in the mouth opening and a decrease of pain; however, the swelling remained unchanged. Endodontic treatment of both teeth 36 and 37 was possible and it was performed under antibiotic therapy: Levofloxacin: Tavanic 500mg (twice a day) in addition to Dalacine 600mg (4tab/d). At the 6-month follow-up, the patient reported an improvement in all the clinical symptoms, especially pain and swelling, and showed no signs of local infection.
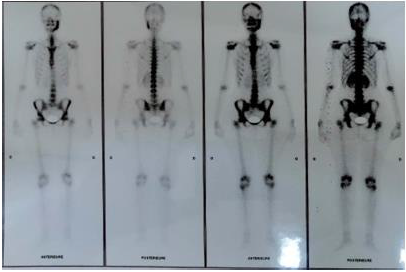
Figure 2: Bone scintigraphy revealing No other scintigraphy abnormalities of radiotracer fixation on the rest of the osteoarticular system.

Figure 4: Recent CBCT of the patient.
a) Axial slice showing severe bone erosion of the left mandible.
b) Coronal slice showing an important thickening of the mandibular bone extending to the homolateral condyle. Muscular hypertrophy of the
masseter muscle and the lateral pterygoidien muscle.
c) The 3D reconstruction comparing the left and the right side and showing the extend of the lesion to the entire Ramus on the left mandibular
side.
Discussion
Primary chronic osteomyelitis of the jaw (PCO) is an aseptic bone inflammation, mostly affecting young patients with a peak incidence between the age of 10 and 20 years. PCO exclusively affects the mandible [7]. The clinical features are marked by swelling, pain and trismus. Labiomental hypoesthesia is also reported [8]. In the present case, the patient presented with severe trismus and firm swelling of the left jaw with no sensory deficit despite the lesion extension to the mandibular canal. The various subtypes of PCO include adult onset, early onset and syndrome associated. However, in all the cases, it is characterized by a strictly chronic nonsuppurative inflammation of the jaw bones with no of suppuration, extra- or intra-oral fistula, or sequestration. In this case, PCO was diagnosed at the age of 13 years based on the clinical and radiological findings and on the absence of a local cause that could explain the etiology. In fact, dental examination did not reveal inflammatory dental foci in both the first and second episodes. Although the teeth 36 and 37 showed signs of root resorption with a negative vitality test during the second episode, a dental origin could not be retained since no signs of infection (suppuration, fistulae) were noticed. Root resorption and aseptic pulp necrosis of the teeth 36 and 37 could be considered as a complication of the inflammatory bony lesion. Conservative endodontic treatment of these teeth was performed in order to avoid any possible periapical complication that can further complicate the course of the disease. With regard to the radiological features of PCO, Computed tomography (CT) is known to be the most effective tool for the evaluation of bony changes, such as cortical bone lesion, sequestra, and subperiosteal bone deposition. However, Magnetic resonance imaging examination would be effective to differentiate osteomyelitis from malignancy (osteosarcoma) and other diseases with similar clinical symptoms, such as fibrous dysplasia, cementoma, paget’s disease etc. Magnetic resonance imaging of osteomyelitis are characterized by changes in SI of the bone marrow, such as decrease in T1-weighted images and increase inT2-weighted images [9]. PCO are known as being debilitating and difficult to manage, with a tendency to recurrence and relapse [10.11]. Many treatment protocols have been proposed. Antibiotics are often used empirically to prevent any bacterial invasion in both acute and secondary chronic osteomyelitis although chronic infection remains an unproven theory for primary chronic osteomyelitis. Non-steroidal anti-inflammatory drugs and corticosteroids are used as first-line options and they are reported to have beneficial effects in reducing symptoms, such as extra-oral swelling and trismus [11]. In the present case, the patient had a long course of antibiotics. She received Dalacine (2.4g/d) and NSAID, which only helped in reducing the clinical symptomatology. Decortication and removal of necrotic bone tissue in primary chronic osteomyelitis of the mandible have been investigated by several authors. However, the outcome of surgical intervention in the treatment of patients with primary chronic osteomyelitis of the jaw is uncertain [13].
Our patient underwent decortication of the left mandible (corpus) one year after the disease onset, followed by hyperbaric oxygen therapy (HBOT) as an adjunct to the anti-inflammatory and antibiotic therapy. In fact, higher levels of available oxygen are proven to induce capillary formation and to increase leukocytes activity [14]. HBOT also stimulates the release of growth factors and stem cells, thus promoting bone healing. However, although the patient was symptom-free for years, exacerbation marked by a severe pain and trismus took place many years later. Two treatment options were proposed to the patient: a conservative approach involving Bisphosphonate therapy or surgical resection of the lesion as a whole. Bisphosphonates have been used for pain relief and control of the disease progression and it is reported to have promising results [15]. However, given the high toxicity of this drug and the reported risk of developing Bisphosphonate- related necrosis of the jaw, the patient refused this treatment. In fact, data with regard to the long-term safety of using these compounds in young patients is still lacking. Concerns have been raised about the possible increased risk of osteonecrosis of the jaw. However, 95% of all the reports investigating this problem involved elderly adults, most of whom had an underlying malignancy, particularly myeloma. According to Dale el al. [14] the removal of the diseased segment is the essential component of the treatment. The segment extent should be determined by evaluating both the radiographic and clinical findings. The resection margins should be designed to include a normal trabecular bone pattern on imaging and to clinically confirm the presence of bleeding bone. However, the patient refused to undergo surgical resection as well. Surgical manipulation of this region may cause facial asymmetry as well as severe aesthetic damage. In this context, Bevin et al. reported that conservative surgical management of PCO not only leads to multiple recurrences but also to significant morbidity and subsequent need for reconstruction [15]. Effective antibiotic treatment in association with steroids and/or HBO was therefore the treatment of choice. It was safe and it could lead to the stabilization of the condition.
References
- D Schulze, M Blessmann, P Pohlenz, KW Wagner and M Heiland (2006) Diagnostic criteria for the detection of mandibular osteomyelitis using cone- beam computed tomography. Dentomaxillofacial Radiology 35(4): 232-235.
- M Baltensperger, K Gratz, E Bruder, R Lebeda, M Makek, et al. (2004) Is primary chronic osteomyelitis a uniform disease? Proposal of a classification based on a retrospective analysis of patients treated in the past 30 years. Journal of Cranio Maxillofacial Surgery 32(1): 43-50.
- GKH Eyrich, MM Baltensperger, E Bruder, KW Gratz (2003) Primary chronic osteomyelitis in childhood and ¨ adolescence: a retrospective analysis of 11 cases and review of the literature. Journal of Oral and Maxillofacial Surgery 61(5): 561-573.
- JT Mader, ME Shirtliff, S Bergquist, JH Calhoun (2000) Bone and joint infections in the elderly: practical treatment guidelines. Drugs and Aging 16(1): 67-80.
- Marx RE (1991) Chronic osteomyelitis of the jaws. Oral Maxillofac Clin North Am 3: 367-381.
- CH Idahosa, W Boggess, LM Levin, F Alawi (2014) Primary chronic osteomyelitis of the mandible in a child. Oral Surgery, Oral Medicine, Oral Patology and Oral Radiology 117(5): 342.
- Agarwal N Kumar, A Tyagi, N De (2014) Primary chronic osteomyelitis in the mandible: a conservative approach. Case Reports.
- Pugmire BS, Shailam R, Gee MS (2014) Role of MRI in the diagnosis and treatment of osteomyelitis in pediatric patients. World J Radiol 6(8): 530-537.
- Ariji Y, Izumi M, Gotoh M, Naitoh M, Katoh M, et al. (2008) MRI features of mandibular osteomyelitis: practical criteria based on an association with conventional radiography features and clinical classification. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105(4): 503-511.
- Baur DA, Altay MA, Flores-Hidalgo A, Ort Y, Quereshy FA (2014) Chronic osteomyelitis of the mandible: diagnosis and management an institution's experience over 7 years. J Oral Maxillofac Surg 73(4): 655-656.
- JPR Van Merkesteyn, RH Groot, J Bras, RS McCarroll, DJ Bakker (1990) Diffuse sclerosing osteomyelitis of the mandible: a new concept of its etiology. Oral Surgery, Oral Medicine, Oral Pathology 70(4): 414-419.
- G Obel, A Krogdahl, T Thygesen, C Godballe (2013) Juvenile mandibular chronic osteomyelitis: 3 cases and a literature review. Journal of Oral and Maxillofacial Surgery 71(2): 305-309.
- N Theologie Lygidakis, O Schoinohoriti, I Iatrou (2011) Surgical management of primary chronic osteomyelitis of the jaws in children: a prospective analysis of five cases and review of the literature. Oral & Maxillofacial Surgery 15(1): 41-50.
- S Lentrodt, J Lentrodt, N Kubler, UM Odder (2007) Hyperbaric oxygen for adjuvant therapy for chronically recurrent mandibular osteomyelitis in childhood and adolescence. Journal of Oral and Maxillofacial Surgery 65(2): 186-191.
- F Dore, L Filippi, M Biasotto, S Chiandussi, F Cavalli, et al. (2009) Bone scintigraphy and SPECT/CT of bisphosphonate-induced osteonecrosis of the jaw. Journal of Nuclear Medicine 50(1): 30-35.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.