Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Pulmonary Barotrauma in COVID-19 Patients Under Non-invasive Ventilation Support: Case Series
*Corresponding author: Sérgio Renato da Rosa Decker, MD. Msc, Hospital Nossa Senhora da Conceição. No. 596 Francisco Trein Avenue, 91350-200, Porto Alegre, Brazil.
Received: February 22, 2022; Published: February 28, 2022
DOI: 10.34297/AJBSR.2022.15.002139
Abstract
Purpose: Pulmonary barotrauma (PBT) is a complication typically seen in intubated patients but is a rare event in those using non-invasive ventilation (NIV) support. In this case report, we identified five patients with COVID-19 who developed PBT on NIV support in a hospital of southern Brazil from March to April 2021.
Results: All the patients were non-smokers with no pre-existing lung disease. They required oxygen therapy which included escalation from nasal cannula to NIV. PBT was diagnosed later in the course of the disease (17.6 ± 4.3 days) and after a mean time of 6 days on NIV support.
Conclusions: We found high PBT rate in COVID-19 patients. The patients developed PBT without being subjected to high leves of EPAP. Therefore, clinicians should be aware of the high risk of PBT among COVID-19 patients, since barotrauma correlates with longer ICU stay and hospitalization
Keywords: Pulmonary barotrauma, COVID-19, Non-invasive ventilation
Introduction
The new coronavirus pandemic has been worrying the world since 2019. In order to improve clinical outcomes, early recognition of clinical deterioration and appropriate respiratory support are crucial in coronavirus disease-19 (COVID-19) patients. Most patients who become seriously ill with COVID-19 do so primarily due to an acute respiratory illness [1] and about 14% will require non-invasive ventilation (NIV) support [2].
Despite novel therapies and ventilation strategies, morbimortality remains high for COVID-19 patients, often due to complications associated with invasive mechanical ventilation (IMV) support, such as pulmonary barotrauma (PBT) [3]. On the other hand, barotrauma is a rare complication of NIV support and tends to be only seen in patients who are chronically using this therapy [4,5]. In the related viral epidemic of SARS in 2002, approximately 10% of patients on NIV were described to develop PBT, with diffuse alveolar damage as the suggested mechanism [6]. However, there is little data on the incidence of barotrauma in critically ill patients with COVID-19, especially in those using only NIV.
Herein, we describe five cases of PBT in patients with COVID-19 using NIV along with a brief literature review on the possible pathophysiologic mechanisms. The cases were selected from a cohort of patients who were hospitalized between March 10 and April 1 of 2021 in a semi-intensive care unit at a tertiary hospital in southern Brazil.
Patient 1
A 68-year-old male with a past medical history of hypertension presented to the hospital with 11-day-onset respiratory symptoms and progressively worsening dyspnea. He had a positive RT-PCR for SARS-CoV-2 at the third day of symptoms. At the emergency department, the patient received amoxicillin-clavulanate and completed a 7-day course of treatment. Dexamethasone was started on day 1, and intermittent bilevel positive pressure airway (BPAP) support was started on day 4. Due to lack of respiratory improvement, he underwent a CT scan, which revealed signs of organizing pneumonia (COP), and prednisone therapy at 1 mg/ kg/day was started. Throughout the following days, the patient progressively needed more aggressive ventilatory parameters to maintain targeted oxygen saturation. On day 13 of hospitalization, daily medical examination found crepitation under cervical skin which was not present on the previous day. A bedside chest X-ray found cervical subcutaneous emphysema and signs of pneumomediastinum [Figure 1]. After 2 days, he experienced a significant clinical deterioration, requiring IMV and was transferred to the ICU.
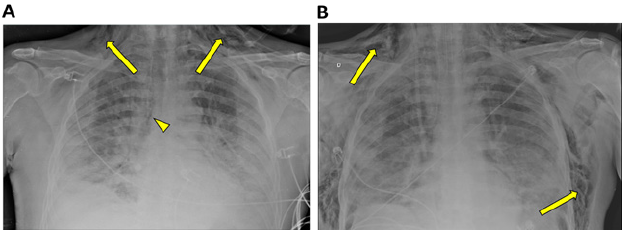
Figure 1A: Chest X-ray obtained on day 13 of hospitalization. The image shows cervicothoracic subcutaneous emphysema (arrow) and signs of pneumomediastinum (arrowhead). In addition, extensive bilateral consolidative opacities and small bilateral pleural effusion are also noted.
Figure 1B: Chest x-ray obtained after the patient was admitted to the ICU and orotracheal intubation and mechanical ventilation. The image shows an increase in subcutaneous emphysema (arrow), evolving with thoracic extension.
Patient 2
A 69-year-old male with an unremarkable prior medical history and a positive RT-PCR for SARS-CoV-2 was admitted to the hospital on the 7th day of respiratory symptoms. Prior to admission, he had used azithromycin, hydroxychloroquine, ivermectin and colchicine. Oxygen therapy with nasal cannula (NC) was started and dexamethasone was prescribed. A CT scan upon admission showed ground-glass opacities in both lungs and at least 40% of parenchymal impairment. Three days later, the patient was transferred to the ICU due to respiratory deterioration, and intermittent BPAP was started. On day 4, the patient was requiring longer periods under NIV support. A chest X-ray was performed [Figure 2] and identified cervical subcutaneous emphysema and a discrete pneumothorax area on the right lung. During ICU admission, the patient required IMV. In the follow-up, he was diagnosed with ventilator-associated pneumonia, evolving with lung abscess and septic pulmonary embolism, and was treated with multiple broad-spectrum antimicrobial regimens.
Patient 3
A male patient, 47 years old with no previous medical history, was admitted to the hospital with a 10-day history of high fever, dry cough and worsening respiratory symptoms. He also tested positive for SARS-COV-2. At the emergency room, he presented with low oxygen saturation and high respiratory frequency rate. On day 2 of hospitalization, the patient required escalation from NC to intermittent BPAP due to worsening of respiratory condition and was encouraged to self-prone. On day 4, due to neck subcutaneous crepitation, a chest X-ray was performed and found subcutaneous emphysema and signs of pneumomediastinum [Figure 3], without significant clinical repercussion, which were conservatively managed. After 2 days, he required IMV and was transferred to the ICU. Due to clinical deterioration, a CT angiography was performed and found pulmonary thromboembolism (PTE) signs, and anticoagulation was promptly started. On ICU, the patient evolved favorably and after 10 days was discharged to a non-intensive care unit.
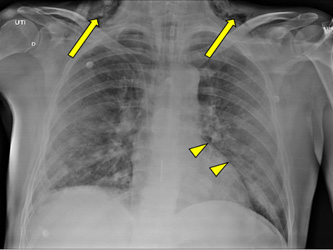
Figure 2: Chest X-ray performed on day 4 of hospitalization, after admission on ICU. The image showed bilateral infiltrative opacities, cervical subcutaneous emphysema (arrows) and signs of pneumomediastinum (arrowheads).
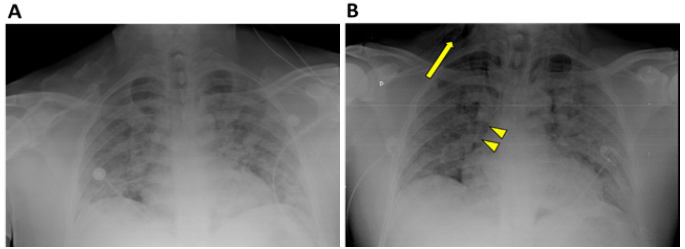
Figure 3A: Chest X-ray performed on admission, which found only extensive bilateral pulmonary opacities.
Figure 3B: Chest X-ray performed on day 4 of hospitalization. The findings include bilateral infiltrative opacities, cervical subcutaneous emphysema (arrow) and signs of pneumomediastinum (arrowheads), the last two which were not present on the previous X-ray.
Patient 4
A 49-year-old male patient with hypertension and in use of losartan was admitted to the hospital with a 12-day history of flu-like symptoms. RT-PCR was positive for COVID-19. He was treated previously to admission with ivermectin, hydroxicloroquin and azithromycin. The patient required oxygen therapy which included escalation from NC to intermittent BPAP due to worsening hypoxemia and was recommended to self-prone. CT scan performed short after admission found approximately 75% of pulmonary parenchyma impairment. BPAP was then changed to continuous positive airway pressure (CPAP) of 10cm H2O, still in intermittent use. On day 8 of hospitalization, while on CPAP of 12 cmH2O, the patient presented with respiratory deterioration. At bedside examination, he presented with cervical crepitation and was diagnosed with subcutaneous emphysema. Due to rapid respiratory failure, he immediately required intubation and was transferred to the ICU. A control bedside X-ray performed shortly after intubation observed not only subcutaneous emphysema, but also a pneumothorax on the right lung, requiring surgical chest tube placement [Figure 4]. Despite initial clinical improvement, with adequate pulmonary reexpansion, the patient evolved unfavorably and later succumbed to his illness.
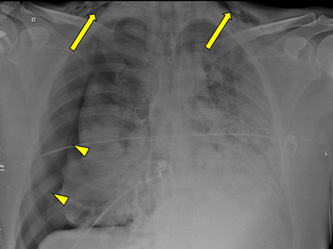
Figure 4: On day 8, a control chest X-ray performed short after intubation found cervical subcutaneous emphysema (arrows) and a large pneumothorax on the right with subtotal lung collapse (arrowehads), requiring surgical chest tube placement.
Patient 5
A 62-year-old female patient, with previous medical history of hypertension and in use of losartan, was admitted to the hospital with worsening dyspnea and hypoxemia. She was on the 7th day of symptoms and had a positive RT-PCR for COVID-19. She was treated with 5 days of azithromycin and dexamethasone 6 mg was also prescribed. She initially required oxygen therapy with NC and later needed escalation to CPAP of 10cm H2O due to worsening dyspnea. CT scan with 50% of pulmonary parenchyma impairment. On day 7 of hospitalization, she changed ventilatory support from CPAP to BPAP due to CO2 retention and began to self-prone. A new CT scan was performed to investigate the respiratory worsening and signs of COP were observed. Dexamethasone was then suspended, and prednisone at 1 mg/kg/day was prescribed. She continued requiring increasing ventilator parameters and was under BPAP support with inspiratory positive airway pressure (IPAP) of 20cm H2O and expiratory positive airway pressure (EPAP) of 12cm H2O. After 3 days on continuous NIV, the patient developed respiratory failure and daily routine examination found cervical crepitation. Due to stablished respiratory insufficiency, intubation was required, but she rapidly evolved with cardiopulmonary arrest. Adequate cardiopulmonary resuscitation was performed by the medical team, without success.
Discussion
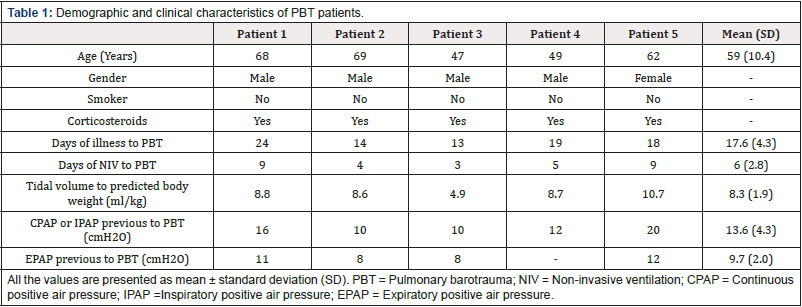
In our study, 56 patients were admitted to the semi-intensive care unit with severe respiratory disease due to COVID-19 infection. Out of these, 21 were women and 35 were male patients. Virtually every patient used NIV at some point during hospitalization. All the case-patients were non-smokers with no pre-existing lung disease, both considered risk factors for barotrauma [7]. The ventilator parameters and demographic characteristics of these patients are summarized in [Table 1].
The patients developed PBT later in the course of the disease (17.6 ± 4.3 days) and after an average time of 6 days using NIV support. The most recent guidelines recommend a target tidal volume (Vt) < 9 ml/kg when using NIV, since high volumes (> 9.2 or 9.5 mL/kg) under NIV are associated with increased mortality [8]. In our case, the mean Vt was 8.3 ± 1.9 ml/kg.
Barotrauma is seen in 5-12% of patients with acute respiratory distress syndrome (ARDS) receiving IMV but is a rare event in patients receiving NIV [9]. A recent study found that the rates of barotrauma in COVID-19 patients receiving IMV are significantly higher than the observed in other ARDS causes (15% vs. 5%) [10]. In our cohort, the incidence of PBT in patients under NIV support was approximately 9%, probably demonstrating that even in nonmechanically ventilated patients this rate is still high.
One possible explanation for the association between high incidence of PBT and COVID-19 is that the virus-induced ARDS could be a unique disease entity with a novel pathophysiology [11,12]. Kahn et al. suggested that the COVID-19 probably causes a heightened inflammatory response, even more intense than other infectious diseases due to our lack of prior immunity, manifested as diffuse alveolar damage [13]. Gattinoni et al. [11] have recently described that patients with COVID-19 ARDS present an atypical form of the syndrome. In this study, the most important observation was a dissociation between the patient’s relatively well-preserved lung mechanics (high compliance) and the severity of hypoxemia [11]. The standard of ARDS management is the use of lung-protective strategies that combine low tidal volume and relatively high PEEP [14]. However, high levels of PEEP may lead to lung overdistension associated with an increase of alveolar dead space [15].
The occurrence of subcutaneous emphysema and pneumomediastinum is generally related to diffuse alveolar damage causing rupture and air leakage. Patients with a longer duration of illness have more diffuse alveolar damage, with a greater extent of pulmonary impairment, which, added to alveolar overdistension by using high PEEP, could lead to an increased risk of developing barotrauma.
Conclusion
In patients who are being treated with NIV and who present with clinical signs of respiratory failure, intubation should be prioritized to avoid excessive intrathoracic negative pressures and self-inflicted lung injury [11,16]. However, regardless of the underlying mechanism, our case report indicates that clinicians should be aware of the high rate of barotrauma seen among patients with COVID-19 using NIV, since it correlates with poor outcomes [17]. Moreover, it also encourages clinicians to have a low threshold to suspect PBT in COVID-19 patients.
Disclosure statement
The authors have no conflicts of interest to declare.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Nicholson TW, Talbot NP, Nickol A, Chadwick A J, Lawton O (2020) Respiratory failure and non-invasive respiratory support during the covid-19 pandemic: an update for re-deployed hospital doctors and primary care physicians. BMJ 369: m2446.
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323(13):1239-1242.
- Wang D, Hu B, Hu C, Fangfang Zhu, Xing Liu, et al. (2020) Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 323(11): 1061–1069.
- Simonds AK (2004) Pneumothorax: an important complication of non-invasive ventilation in neuromuscular disease. Neuromuscul Disord 14(6): 351-352.
- Xu XP, Zhang XC, Hu SL, Xu JY, Xie JF, et al. (2017) Noninvasive Ventilation in Acute Hypoxemic Nonhypercapnic Respiratory Failure: A Systematic Review and Meta-Analysis. Crit Care Med 45(7): e727-e733.
- Pattupara A, Modi V, Goldberg J, Ho KS, Bhatia K, et al. (2020) Pulmonary Barotrauma During Noninvasive Ventilation in Patients With Covid-19. Chest Infections 158(4): A337.
- Noppen M (2010) Spontaneous pneumothorax: epidemiology, pathophysiology and cause. Eur Respir Rev 19(117): 217-219.
- Pfeifer M, Ewig S, Voshaar T, Randerath WJ, Bauer T, et al. (2020) Position Paper for the State-of-the-Art Application of Respiratory Support in Patients with COVID-19. Respiration 99(6): 521-542.
- Anzueto A, Frutos Vivar F, Esteban A, Alía I, Brochard L, et al. (2004) Incidence, risk factors and outcome of barotrauma in mechanically ventilated patients. Intensive Care Med 30(4): 612-619.
- McGuinness G, Zhan C, Rosenberg N, Azour L, Wickstrom M, et al. (2020) Increased Incidence of Barotrauma in Patients with COVID-19 on Invasive Mechanical Ventilation. Radiology 297(2): E252-E262.
- Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, et al. (2020) COVID-19 Does Not Lead to a "Typical" Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med 201(10): 1299-1300.
- Gattinoni L, Chiumello D, Rossi S (2020) COVID-19 pneumonia: ARDS or not?. Crit Care 24(1): 154.
- Kahn MR, Watson RL, Thetford JT, Wong JI, Kamangar N (2021) High Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019. J Intensive Care Med 36(6): 646-654
- Jabbari A, Alijanpour E, Amri Maleh P, Heidari B (2013) Lung protection strategy as an effective treatment in acute respiratory distress syndrome. Caspian J Intern Med 4(1): 560-563.
- Ramin S, Charbit J, Dagod G, Mehdi Girard, Samir Jaber, et al. (2020) Transpulmonary pressure in SARS-CoV-2-associated acute respiratory distress syndrome: a single-center observational study. Crit Care 408 (2020).
- Brochard L, Slutsky A, Pesenti A (2017) Mechanical Ventilation to Minimize Progression of Lung Injury in Acute Respiratory Failure. Am J Respir Crit Care Med 195(4): 438-442.
- Schnapp LM, Chin DP, Szaflarski N, Matthay MA (1995) Frequency and importance of barotrauma in 100 patients with acute lung injury. Crit Care Med 23(2): 272-278.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.