Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Superior Mesenteric Venous Thrombosis - The Impact of Inflammation and Hypercoagulability
*Corresponding author: Leonard Ranasinghe, California Northstate University, 9700 W Taron Dr, Elk Grove, CA, USA.
Received: January 31, 2022; Published: February 09, 2022
DOI: 10.34297/AJBSR.2022.15.002118
Abstract
Superior mesenteric vein thrombosis (SMVT) often presents with abdominal pain out of proportion to physical exam findings but can also be asymptomatic. If left untreated, the thrombosis can cause bowel ischemia, multisystem organ failure, and eventually death. Therefore, while rare, superior mesenteric vein thrombosis should be considered as a differential diagnosis especially in cases with abdominal inflammation and hypercoagulability. Since SMVT can present as abdominal pain, a common reason for ED admission, or show up asymptomatically on CT, rapid diagnosis and anticoagulant administration is crucial to successful management. In this case report, a 78-year-old woman presents with abdominal cramping and bloody loose stools. The diagnosis was made using CT. This report reviews the CT image findings and hypercoagulability work- up. Management included anticoagulants in both the emergency department and on hematology follow-up.
Keywords: Superior Mesenteric Venous Thrombosis, Hypercoagulability, Epigastric Pain, Abdominal Pain, Inflammation
Abbreviations: AMI: Acute mesenteric ischemia; SMV: Superior mesenteric vein; SMVT: Superior mesenteric venous thrombosis; EGD: Esophagogastroduodenoscopy; CRP: C Reactive Protein; INR: International normalized ratio; vWF: von Willebrand factor
Introduction
Acute mesenteric ischemia (AMI) is caused by inadequate blood flow through the mesenteric vessels that can lead to end organ damage of the bowel wall. AMI can present as arterial (occlusive or nonocclusive) or venous etiologies [1]. Blockage of the superior mesenteric vein (SMV) is rare as it accounts for 1 in 1000 emergency department admissions, and 6% to 9% of all cases of acute mesenteric ischemia. [2] Delayed intervention is often lethal. Superior mesenteric venous thrombosis (SMVT) may be embolic, thrombotic, primary vasoconstrictive, or secondary to venous thrombosis. [3] Thrombosis presents with abdominal pain out of proportion to endoscopic findings in 91- 100% of cases and occult blood in 50% of cases. [4] Many diseases can lead to SMVT through inflammation of the surrounding tissues. The most common is due to recent abdominal surgery, while other causes include hypercoagulability, malignancy, polycythemia vera, portal hypertension, protein C deficiency, or sepsis. [5] SMV traumatic injuries are associated with a 45-52.7% mortality rate even though they are rare causes of trauma admissions. The most important factors influencing mortality rate according to recent studies are hemodynamic stability, vascular injury severity, and degree of comorbid injuries. [6] Widely accepted management, despite no optimal, definite treatment, of SMVT includes anticoagulation, thrombolysis, or surgery depending on hemodynamic stability. [5] Although SMVT may not be a common cause of emergency department admission, it is important to consider or recognize SVM thrombosis due to the high mortality rate and because early detection may improve outcome.
Case Presentation
A 78-year-old female with a past medical history of diabetes, epigastric hernia, gastric ulcer, hyperlipidemia, hypertension, and hypothyroidism presents to the emergency department with abdomen cramping and bloody loose stools. The patient’s vital signs on physical examination were blood pressure of 134/61 mmHg, pulse 84 beats per minute, respiratory rate 18 breaths per minute, temperature 97.3 degrees Fahrenheit, and pulse oximetry 94% on room air. The abdominal physical exam was significant for the lack of abdominal tenderness with no guarding or rebound and a soft abdomen with no masses. The genitourinary exam showed a positive Guaiac test. The rest of the physical exam was unremarkable.
Initial labs showed an initial white blood cell count was 16,000 uL (4,500-11,000/uL), hemoglobin 16 g/dL (12-16g/dL), platelets 241 x 10^9/L (150-450x10^9/L), INR 1.9 (<1.1), and lactic acid 1.3 mEq/L (0.7 to 2.1 mEq/L). GI diarrheal panel was negative and C-reactive protein was 11.2 mg/dL (≤ 0.8 mg/dL) . On repeat examination, white blood cell count was 8,700 (4,500-11,000/ uL), hemoglobin 12 g/dL (12-16g/dL), platelets 196 x 10^9/L (150-450x10^9/L), and lactic acid 0.7 mEq/L (0.7 to 2.1 mEq/L).
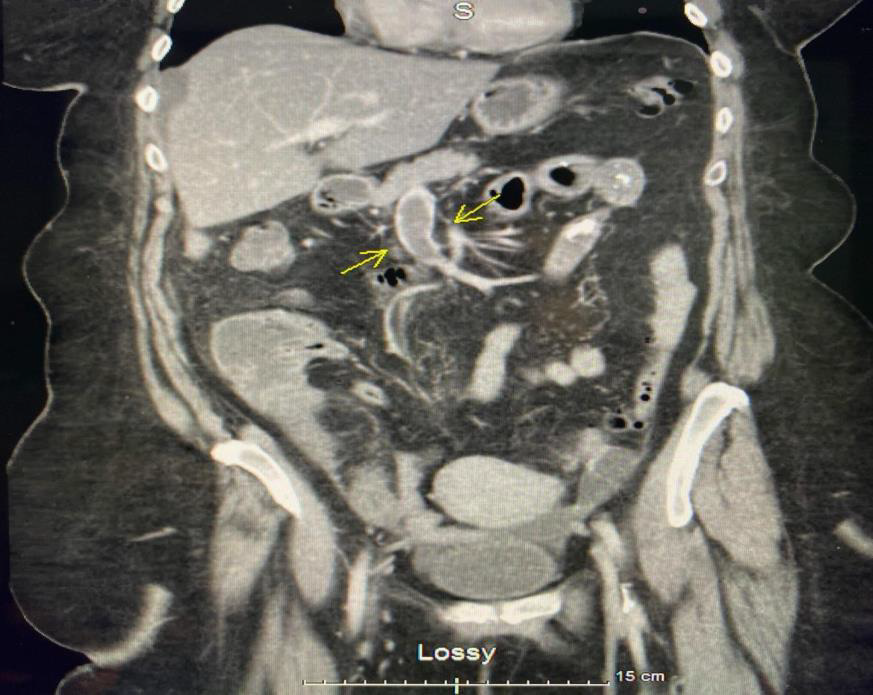
Figure 1: Coronal computed tomography with intravenous contrast showing superior mesenteric venous thrombosis (yellow arrows).
The CT with contrast of abdomen and pelvis showed a proximal SMV with a large clot that extended into part of the distal branches, but celiac and superior mesenteric artery branches remained patent (Figure 1). Pelvic small bowel loops had wall thickening and edematous changes with stranding extending into mesenteric fat planes. Ascites were evident around the liver and in the low pelvis (Figure 2 & 3). Scattered diverticulosis was present on the colon without definite acute diverticulitis. The terminal ileum was seemingly spared. The cecum demonstrated some fluid without wall thickening. The ascending colon was partially collapsed along the transverse colon. Also noted was prominent atherosclerosis of aorta and first-order vessels. Chest x-ray showed no significant or consolidating infiltrates and ECG demonstrated normal sinus rhythm. Esophagogastroduodenoscopy (EGD) findings showed a small hiatal hernia in the gastroesophageal junction 35 cm from incisor. No gross lesions and no lesions in stomach and duodenum.

Figure 2: Coronal computed tomography with intravenous contrast showing Ascites (yellow arrows) between the properitoneal fat and the colon.
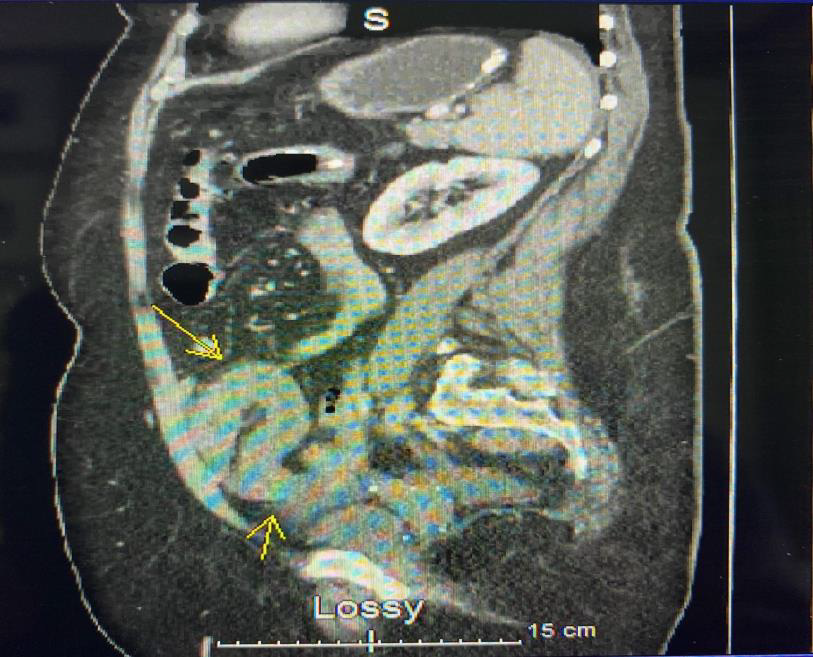
Figure 3: Sagittal lateral computed tomography with intravenous contrast showing Ascites (yellow arrows) between the properitoneal fat and the colon.
After diagnosis of SMVT, the consultant surgeon started her on a heparin drip. No surgical interventions were planned since she showed improvement. Initial lactic acid trend was normal and white blood cell count improved to normal. The patient was switched to Apixaban before discharge. She was given Piperacillin and Tazobactam for possible enteritis which improved her symptoms and then was given a 7-day course of Amoxicillin and Clavulanic acid upon discharge. Dark stools resolved itself before discharge, which was likely old blood because she was hemodynamically stable. Patient was advised to arrange additional blood tests for hypercoagulation done by the hematologist as an outpatient. Patient was seen by Hematology 2 months later for her hypercoagulable work up. Blood studies taken included Prothrombin (F2), Factor V Leiden (F5), Phospholipid antibody IgM which all returned negative. Phospholipid Ab IgG was elevated at 17.5 GPL. It was also discovered that she has a family history of thromboembolism in her mother, niece, and brothers. Patient was advised to continue Apixiban for at least the next 6 months.
Results and Discussion
Superior mesenteric venous thrombosis (SMVT) is rare but can have deadly consequences if left untreated. Blockage of superior mesenteric veins can lead to bowel ischemia and necrosis which ultimately causes multiple organ dysfunction and death. [7] While abdominal pain may be a nondescript symptom, SMVT commonly has abdominal pain out of proportion to the physical exam findings [3]. Early use of contrast enhanced CT scans and aggressive anticoagulant therapy has helped reduce the mortality rate of SMVT from 44% to around 10-20%. [4,8] Recognition of inflammation and hypercoagulable risk factors were two potential drivers of the patient’s SMVT. The patient showed clear inflammation with elevated C Reactive Protein (CRP) and white blood cell count which likely reflects their suspected enteritis. Interestingly, measures of coagulation like the international normalized ratio (INR) and platelet count remained in normal ranges in the emergency department. On hematology follow-up, the patient was found to have elevated phospholipid antibody IgG meaning she has elevated antiphospholipid antibodies, placing her at increased risk for thrombosis. Antiphospholipid antibodies are thought to increase coagulation by inhibiting the anticoagulant protein C pathway and upregulating the expression of Tissue Factor, a high-affinity receptor and cofactor for factor VII/VIIa that precipitates normal blood coagulation and has been shown to trigger thrombosis. [9] When taking into account the patient’s laboratory tests, family history of thromboembolism, and her diagnosis of SMVT, antiphospholipid syndrome should be considered as a possible etiology for her symptoms. Antiphospholipid syndrome is an autoimmune disorder often associated with other autoimmune disorders, such as systemic lupus erythematosus (40% of all antiphospholipid syndrome cases have this association), that can affect multiple systems of the body due to continuous presence of antiphospholipid antibodies. [10] In addition to venous and arterial thrombosis, such as DVTs, strokes, and TIAs, this syndrome is also known to cause recurrent pregnancy loss, thrombocytopenia, and other manifestations, which were not found to be present in this patient’s medical history. Along with the patient’s lack of clotting history prior to her current thrombosis at her older age and lack of diagnosed autoimmune disease, a diagnosis of antiphospholipid syndrome for this patient becomes less likely. Additionally, the baseline of the antiphospholipid antibody test is known to increase with age and the phospholipid antibody IgG in antiphospholipid syndrome patients is usually found to be >40 GPL as opposed to the slight elevation found in this patient at 17.5 GPL (Normal range: <15).10 Although antiphospholipid syndrome is less likely in this patient, the presence of elevated antiphospholipid antibodies and her medical history do put her at increased risk for thrombosis, especially in the setting of infection.
The patient’s history of hypertension and hyperlipidemia are both well-known risk factors for the development of atherosclerosis, which was found to be prominent in her aorta and first-order vessels on the Abdominal CT. These risk factors may have led to thrombosis in her SMV. The findings of ascites around the patient’s liver and lower pelvis on the CT scan, along with the findings of fatty liver and melena, means portal hypertension is potentially undiagnosed in this patient. Portal hypertension accounts for 75% of all ascites patients and some studies have shown evidence of increased portal venous pressure in the early stages of fatty liver disease despite little to no fibrosis present. [11,12] However, the ascites may have developed after the SMVT formed and the other findings are not conclusive enough to make a clear diagnosis of portal hypertension. There are reports of an association between diabetes and venous thromboembolism due to enhanced coagulation in the form of raised concentrations of fibrinogen, von Willebrand factor (vWF) and other endothelium-derived mediators, which increase blood viscosity and promote platelet activation and adhesion, and reduce fibrinolytic potential via raised concentrations of PAI-1. [13] There are reports of acceleration of atherosclerosis by diabetes drives inflammation and slows down blood flow, but other reports have refuted a true association between venous thromboembolism and diabetes mellitus. [14] Regarding the patient’s hypothyroidism, a 2019 study showed a significant association between hypothyroidism and venous thromboembolism and deep vein thrombosis events if the patient is not taking Levothyroxine. [15] In this patient’s case, it appears the risk factors for thrombosis and inflammation were sufficient to cause a SMVT, however, further progression to a hypercoagulable state could have been deadly.
In cases without peritonism or perforation, anticoagulation or thrombolysis is widely used and accepted even though there is no optimal, definitive management plan. In cases involving peritonism or perforation, which this patient did not experience, surgical intervention may be considered. Surgical intervention may be indicated if there is evidence of ischemia rather than used for diagnosis as in the past. Antibiotics are not shown to improve outcome but should be included if perforation or sepsis is suspected. In our patient, antibiotics were administered for enteritis. As is for any thrombosis or embolism - recanalization is key. Anticoagulants administered as early as possible helped with recanalization. [16] Our patient had no evidence of ischemia, showed improvement upon administration of heparin (white blood cell counts and lactic acid trends), and was hemodynamically stable. No surgery was indicated in our patient and this method seems to be less favorable compared to non-invasive strategies. Rather, surgery should only be considered when there is CT imaging of perforation or hematologically unstable condition as justification.
Conclusion
This case demonstrates how an inflamed state and hypercoagulable risk factors can culminate into SMVT. The workup for clinically suspected SMVT should include prophylactic anticoagulation or thrombolysis as early as possible, in addition to CT scan for diagnosis. If there are signs of ischemia, peritonism, or perforation, consider surgical intervention. Although rare, the potential for SMVT to cause multisystem organ failure and death make it critical to identify.
Acknowledgements
None
Conflict of Interest
There are no conflicts of interest to disclose.
References
- Dang v Chat (2020) Acute Mesenteric Ischemia: Background, Anatomy, Pathophysiology. Medscape.
- Singal AK, Kamath PS, Tefferi A (2013) Mesenteric Venous Thrombosis. Mayo Clin Proc 88(3): 285-294.
- Al-Zahrani HA, Lindsay T (2014) Principles of Critical Care. McGraw- Hill Education 1036 - 1104.
- Bashar Hmoud, Ashwani K. Singal, Patrick S. Kamath (2014) Mesenteric Venous Thrombosis. J Clin Exp Hepatol 4(3): 257-263.
- Broussard A, Wehrle CJ, Samra NS (2021) Anatomy, Abdomen and Pelvis, Superior Mesenteric Vein. StatPearls (Internet), StatPearls Publishing.
- B Phillips, S Reiter, E P Murray, D McDonald, L Turco, et al. (2018) Trauma to the Superior Mesenteric Artery and Superior Mesenteric Vein: A Narrative Review of Rare but Lethal Injuries. World J Surg 42(3): 713-726.
- W Andrew Oldenburg, L Louis Lau, Thomas J Rodenberg, Hope J Edmonds, Charles D Burger (2004) Acute mesenteric ischemia: a clinical review. Arch Intern Med 164(10): 1054-1062.
- Andrew Samoyedny, Sai Sajja, Asanthi Ratnasekera (2020) Idiopathic acute mesenteric venous thrombosis causing ischemic enteritis: A case report. Int J Surg Case Rep 74: 247-250.
- Mary Katherine Farmer-Boatwright, Robert A S Roubey (2009) Venous Thrombosis in the Antiphospholipid Syndrome. Arterioscler Thromb Vasc Biol 29(3): 321-325.
- Jean G Bustamante, Amandeep Goyal, Pankaj Bansal, Mayank Singhal (2021) Antiphospholipid Syndrome. StatPearls.
- Said A Al-Busafi, Julia Mcnabb-Baltar, Amanda Farag, Nir Hilzenrat (2012) Clinical Manifestations of Portal Hypertension. Int J Hepatol.
- Gyorgy Baffy (2018) Origins of Portal Hypertension in Nonalcoholic Fatty Liver Disease. Dig Dis Sci 63(3): 563-576.
- V Petrauskiene, M Falk, I Waernbaum, M Norberg, J W Eriksson (2005) The risk of venous thromboembolism is markedly elevated in patients with diabetes. Diabetologia 48(5): 1017-1021.
- Jones EW, Mitchell JRA (1983) Venous thrombosis in diabetes mellitus. Diabetologia 25: 502-505.
- Wei Ting (2019) Association between hypothyroidism and venous thromboembolism and the effect of levothyroxine in the adult: a nationwide Cohort study. Endocrine Abstracts 63: 344.
- Phoenix E, Beck J, Patterson TJ, Spence RAJ, Taylor MA, et al. (2020) A systematic review of the management of acute superior mesenteric vein thrombosis in adults. J Pancreatol 3(3): 111-120.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.