Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Thermogram Vs Mammography for the Detection of Breast Cancer
*Corresponding author: Roxana Rivera Valencia, General Physician, Universidad de Carabobo, Venezuela.
Received: November 30, 2021; Published: December 07, 2021
DOI: 10.34297/AJBSR.2021.15.002065
Summary
Breast cancer is among the leading causes of death in women between the ages of 25 and 65, with an expected incidence of 1 in 8 women in most countries. Research and early diagnosis remain the best way to reduce the number of deaths from breast cancer. However, there is some debate about the best method of screening patients for this disease. Mammography is currently the main screening study for the early detection of this disease. The USA. The Food and Drug Administration, along with many other national societies, still describe it as the most effective screening test for breast cancer. Yet some doctors have advocated using thermography as a diagnostic aid for the detection of breast cancer despite a lack of scientific evidence in their favor.
Keywords: Mammography; Thermography; Breast Cancer; Early Detection
Introduction
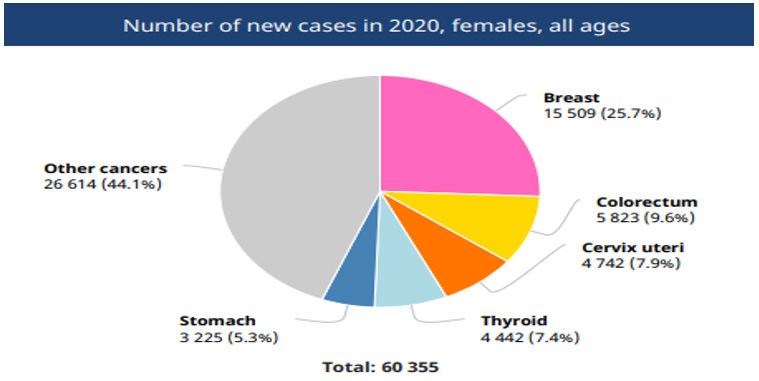
Cancer is one of the most deadly diseases in the world, according to the World Health Organization during 2020 almost 10 million deaths were registered, breast cancer being the most frequent and with the highest number of deaths among women with 2.26 million people affected, becoming one of the main causes of mortality in the world. (WHO, 2021)[1]. The World Health Organization (WHO) estimates that by 2030, an estimated 27 million new cases can be expected. According to the Globocan report, in 2020 25.7% of Colombian women are diagnosed with breast cancer, an alarming figure, since the best treatment must be decided between radiation, mastectomy and chemotherapy, so there is no at the moment a cure for this type of cancer, for this reason the early detection of cancer is of great importance to choose the best possible treatment [2].
For this reason, today, there are different techniques to carry out the diagnosis of this pathology (mammography, ultrasound, magnetic resonance, biopsies, and more recently thermography) [3]; Mammography being the most used method currently, however, it presents the risk of ionization, radiation and the discomfort of breast compression [4]. It is important to mention that the early detection of this disease plays an important role in reducing the mortality rate [5], since, if the tumor is detected before reaching a size of 10 mm, the patient has an 85% probability of cure [6].
At present there is a ground war between those who favor different early detection diagnostic methods, on the one hand there are those who defend thermography and those who prefer mammography for the early detection of breast cancer. The mammogram portion is supported by federal health agencies and nongovernmental organizations (NGOs), as well as the mammography industry [7].
For the most part, poorly supported thermography advocates are outnumbered and outnumbered by the mammogram crowd, which has declared a soft war, at least for now, on thermography to restrict or deny its independent use of screening for breast cancer [8]. In this section, the use of each of its advantages and disadvantages will be objectively analyzed.
Methodology
The study design was that of a systematic review of the evidence in the scientific literature on the usefulness of thermography vs mammography in the early detection of breast cancer.
The literature search took place between October and November 2021, delving into various bibliographic databases in order to obtain information and review previous studies on the exposed subject. The databases used were Pubmed-Medline, Web of Knowledge (WOK) and SCOPUS, in which the search strategies differed depending on the source used. The keywords and Boolean operators used were “thermography” OR “Mammography” “Breast cancer” AND “mortality” described through DeCS (Descriptors in Health Sciences). In order to obtain a greater update on the matter, the articles published in the last 10 years were set as a temporary filter for the search.
Results
Breast cancer is defined as a pathology that involves the abnormal and accelerated growth of cells of the glandular epithelium, which is the thin layer of tissue that lines the mammary glands and is made up of cells specialized in secretion, which have greatly increased their capacity. reproductive tissue, these cells can spread through the blood or lymphatic vessels and reach other parts of the body, attaching themselves to tissues and growing, forming metastases [9].
According to studies by the organization BreastCancer.org (2015), after being diagnosed with breast cancer, the specialized professional must assign a category of the finding taking as a reference the distance that the cancer cells have reached. This process is called staging or determination of the stage, this is how the stage or state allows to relate the amount that is present within the body, which helps to determine the level of severity of this type of condition and the next step in the treatment [10] (Figure 1).
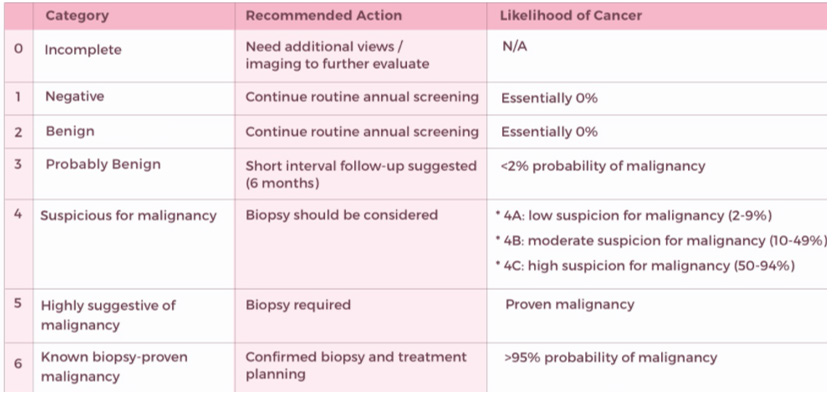
Being mammography the traditional and main screening method, thanks to this we will find the BI-RADS classification in the results of this, BI-RADS is defined as a standard system to describe the results and findings of mammograms. This system (called Breast Imaging Reporting and Data System or BI-RADS) classifies the results in categories numbered from 0 to 6 as shown in the following Figure 2.
Mammography
Mammography consists of a diagnostic X-ray image exploration of the mammary gland, using equipment called a mammograph, using a breast tissue exploration technique, which uses low-energy ionizing radiation (low kilovoltage) from 25 to 35 kv and low penetration power milliamperage (mA) of 100 Ma. In addition, X-ray generators for mammography units are usually high frequency, that is, they convert the input voltage of 50 or 60 hertz [Hz] into a frequency of up to 100 kilohertz [kHz] [10].
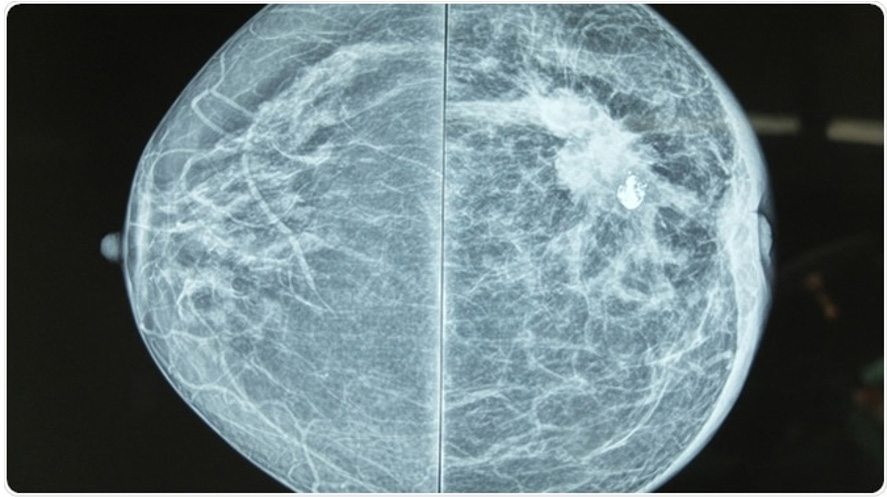
In a mammography image we can observe two types of densities, one of them is called “water” density that correspond to epithelial tissue such as skin, nipple, muscular, vascular and lymphatic structures. The other type of density is known as “fat” density that corresponds to the hilum of lymphatic structures and we can also visualize suspicious high density regions or unusual configuration such as microcalcifications suggestive of both benign and malignant neoplastic lesions [11] as we can see in Figure 3.
The sensitivity of mammography is approximately 63% in very dense breasts and 87% in breasts with higher fat content; its specificity is between 87% and 99% [11] (Figure 3).
Thermography
Thermography is a non-invasive technology (it does not produce pain or emit radiation), which obtains images associated with changes in the human body’s temperature by means of a thermographic camera.In essence, this technique is based on the fact that every living being emits a high amount of infrared radiation due to your own body heat [12] .
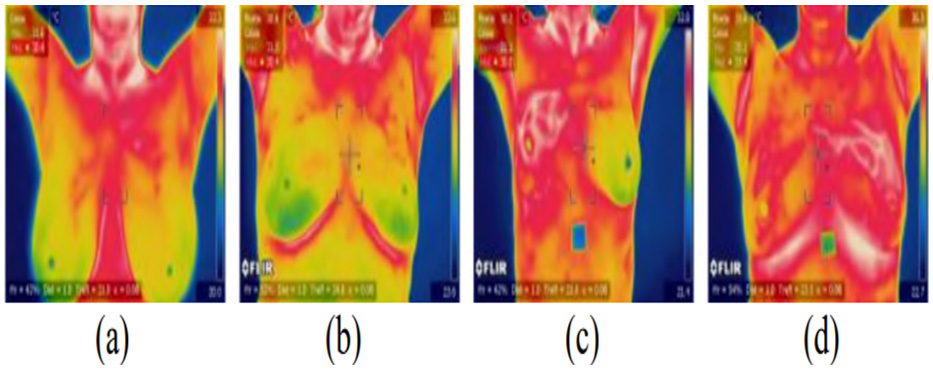
According to the American Academy of Thermology (AAT) Infrared imaging of the breast (thermology) is a physiological study that can assess changes in breast tissue by providing accurate and reproducible high-resolution images of skin temperature. To detect minimal changes in the heat emission of the skin. Figure 4 Malignancies are generally warmer than normal tissue due to nitrous oxide production which produces local vasodilation first, and then increases blood vessel growth, leading to increased blood flow through the tumor, as well as the rate of metabolism more high in cancer cells [13].
Thermography is an ideal diagnostic tool not only for women over 40, but also for young women. Breast thermography has been investigated for more than 30 years, having an average sensitivity and effectiveness of 90% (Thermology, 2019) [14] (Figure 4).
Discussion
Mammography equipment is high maintenance and expensive. Sensitivity is reduced when exploring dense breasts, or in young women. False positives occur in about 10% of cases, causing unnecessary tests, increased costs, significant mental, emotional and physical damage [15].
Mammography can also lead to overtreatment of small tumors that do not require further testing or treatment, since there is no way to distinguish them from those tumors that do. False negatives occur in about 20% of screening mammograms, especially in very dense breasts and in younger women [16].
Mammograms also cause radiation exposure, which is most dangerous for women under 40 years of age. In this group, a diagnostic mammogram is valuable if it helps to identify breast cancer early, but not a screening mammogram because of the high number of false positives. Above this age, the risk of failing to diagnose breast cancer is higher [17].
On the other hand, thermography, or digital infrared thermal imaging, was probably a good choice to mammography. In fact, many studies reported it to be as sensitive as 97%, especially when it comes to younger women. However, this has not been confirmed by large meta-analysis, as well as by subsequent studies [18]. Currently, the detection rate for thermography is only 42% to 80% of cancers, compared with 82% to 93% with mammography. His false positive rate is 25%, more than double that of mammography. No tests exist that can safely detect breast cancer as sensitive as mammography [19].
Also, according to Helen Barr, the head of the FDA’s quality standards division for mammography, “A lot of evidence shows that mammography is still the most effective screening method for finding breast cancer early, in most treatable scenarios [20]. You should not rely solely on thermography for breast cancer research or diagnosis” [18].
Conclusion
It can be concluded with the investigation of the articles in this work, that infrared thermography is an innovative proposal for the diagnosis of physiological changes (cancer). In young patients who have a family genetic history with this disease. Taking into account the density of your breasts, it is not possible to do periodic followup, even more so because of the high costs of the exams that we traditionally use today (mammography, ultrasound and resonance).
Thus achieving that every day, the mortality figures of young women increase in the world. However, this diagnostic method does not replace or substitute mammography as the main screening method for the early detection of breast cancer, influenced mainly by large mammogram companies and by the FDA, which only approves the use of thermography with a complementary tool. Referring to its use in conjunction with a primary screening test such as mammography, due to its little scientific evidence to support it, its sensitivity and specificity not yet established.
Its high number of false positives. Thus leaving mammography as the main screening study for the early detection of breast cancer. Taking into account that thermography in a few years with more studies, scientific evidence could accept its participation along with mammography.
Interest Conflict
The authors have declared no conflict of interest.
References
- (2019) What is breast cancer? Obtained from Where does breast cancer start? American Cancer Society.
- Bautista N (2020) Ministry of Health and Social Protection. Obtained from Minsalud.
- J H Vasconcelos, W P dos Santos, R C F Lima, (2018) Analysis of Methods of Classification of Breast Thermographic Images to Determine their Viability in the Early Breast Cancer Detection. IEEE Latin Am Trans 16(6): 1631-1637.
- M A Díaz Cortés, N Ortega Sánchez, S Hinojosa, D Oliva, E Cuevas, et al. (2018) A multi-level thresholding method for breast thermograms analysis using Dragonfly algorithm. Infrared Phys Technol 93: 346-361.
- M C Araújo, R C Lima, R M De Souza, (2014) Interval symbolic feature extraction for thermography breast cancer detection. Expert Syst Appl 41(15): 6728-6737.
- N Cruz Ramirez, M M Efrén, A A María Yaneli, M D C M Enrique, A M Héctor Gabriel, et al. (2013) Evaluation of the diagnostic power of thermography in breast cancer using bayesian network classifiers. Comput Math Methods Med 2013: 264246.
- L A Bezerra, M M Oliveira, T L Rolim, A Conci, F G S Santos, et al. (2012) Estimation of breast tumor thermal properties using infrared images. Signal Process 93(10): 2851-2863.
- Tiago B Borchartt, Aura Conci, Aida Aguilar, Angel Sanchez, Victor H Andaluz (2013) Breast thermography from an image processing viewpoint_ A survey. Sciencedirect 93(10): 2785-2803.
- Mondragón C Y (2021) Diagnostic Thermography as Support in Breast Cancer Screening. Institutional Repository UNAD.
- Maria G Perez, Aura Conci, Angel Sanchez, Victor H Andaluz, Aida Aguilar (2014) Early detection of breast cancer by thermography in Ecuador.
- Lopez, R J, (2016) In R J, Lopez, Manual of Mammary Radiology. Pan Ame p. 1-4.
- Omranipour R, Ali Kazemian, Sadaf Alipour, Masoume Najafi, Mansour Alidoosti, et al. (2016) Comparison of the accuracy of thermography and mammography in the detection of breast cancer. Breast care (Basel) 11(4): 260-264.
- Kennedy D A, Tanya Lee, Dugald Seely (2009) A Comparative Journal of Thermographyas a Breast Cancer Research Technique. Integr cancer ther 8(1): 9-16.
- Diana Morales Venegas, Santiago Tello Mijares (2020) Identification of breast cancer in thermographic images using convolutional neural networks. Tec Lerdo Sci Eng Dev Magazine 1(6).
- Cancer gov. (https://www.cancer.gov/types/breast/mammograms-fact-sheet)
- E Mahmoudzadeh, M A Montazeri, M Zekri, S Sadri, (2015) Extended hidden Markov model for optimized segmentation of breast thermography images. Infrared Phys Techn 72: 19-28.
- M EtehadTavakol, V Chandran, E Y K Ng, R Kafieh, (2013) Breast cancer detection from thermal images using bispectral invariant features. Int J Therm SCI 69: 21-36.
- L F Silva, D C M Saade, G O Sequeiros, A C Silva, A C Paiva, et al. (2014) A New Database for Breast Research with Infrared Image. J Med Imaging Health Inform 4(1): 92-100(9).
- E Y K NG, U RajendraAcharya, Louis G Keith, Susan Lockwood, (2009) Detection and differentiation of breast cancer using neural classifiers with first warning thermal sensors. Inform Sciences 177(20): 4526- 4538.
- (2021) Breast Cancer Research: Thermogram no replacement for mammogram. Fda gov.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.