Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Digital Dentistry: Where are We Now and Where are We Going?
*Corresponding author:Alejandro Lanis, Department of Restorative Dentistry and Biomaterials Science, Harvard School of Dental Medicine, Boston, MA, USA.
Received:December 21, 2022; Published:January 23, 2023
DOI: 10.34297/AJBSR.2023.17.002413
Abstract
The incorporation of virtual engineering and its application in dentistry is revolutionizing our profession. Nowadays, digital technologies are being applied in diverse processes in probably every dental specialty. The integration of digital information allows the combination of the radiographic, biologic, prosthetic, surgical and laboratory fields under a common virtual scenario, permitting innovative alternatives for dental treatment and optimizing patient’s healthcare. This article will briefly review the historical development of digital technologies in dentistry, discuss the current scope of possibilities for digitally driven patient care, and look ahead towards what’s coming next in our new digital reality.
Introduction
Given the digitization of our daily lives in the 21st century, it should come as no surprise that dentistry is digitizing as well. In fact, our profession is already much more digital than many practitioners realize. From the humble beginnings of niche technologies with limited applicability, digital workflows and applications have exponentially increased in the last fifteen years. While early manifestations of digital dentistry perhaps fell short of their analog counterparts, the same cannot be said of today’s reality. Not only have digital workflows contributed to optimizing dental diagnosis, planning and treatment; they are pushing to make conventional approaches and benchmarks obsolete. Even more, the incorporation of artificial intelligence and robotic assisted procedures are now pushing the boundaries further and what is expected in the following years will probably surpass our own predictions.
Origins of Digital Dentistry
The spark that lit the digital revolution in dentistry can be traced back to Europe in the 1970’s and early 1980’s. The desire to leverage on advances in computing and robotics with respect to limiting manufacturing errors for indirect restorations propelled Dr. Francois Duret and his team to introduce computer-assisted design and computer-assited manufacturing (CAD/CAM) technology to dentistry in 1971 [1]. Other innovators on the continent followed suit in patenting CAD/CAM technologies in 1979 and 1980 [1]. One of those European patents, filed by Drs. Mörmann and Brandestini, would lead to the development of the commercially available CEREC system. The initial goal in developing the CEREC system was to provide an esthetic, durable alternative to restoring teeth that overcame the deficiencies of resin composite in early 1980’s, which was lacking in resistance to wear and marginal degradation [2]. Two critical components for modern digital dentistry were introduced with these systems: digital data acquisition with an intraoral scanner (IOS), and digitally driven manufacturing (Figure 1).
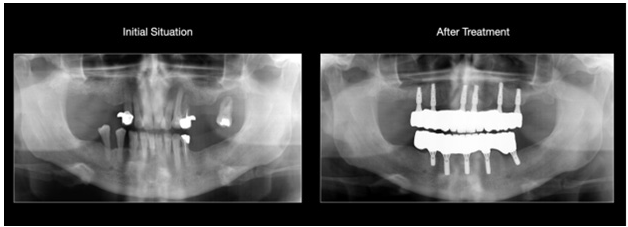
Another largely European-driven innovation that laid the groundwork for today’s digital workflows is known as cone-beam computed tomography (CBCT). Mozzo, et al. [3] and colleagues first published about the successful use of CBCT imaging for dental applications in 1998 [3]. Independently working in Japan with computerized tomography (CT) technology of Finnish origin, Arai and colleagues published successful outcomes in 1999 [4]. The development of accurate 3D imaging, lower radiation exposure and cost than traditional CT, is perhaps the most important development for diagnostic evaluation and treatment planning in dentistry since the dental x-ray in 1896 (Figure 2).
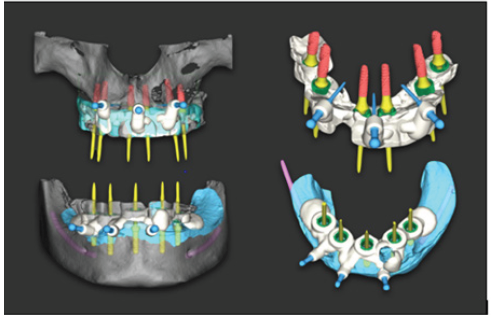
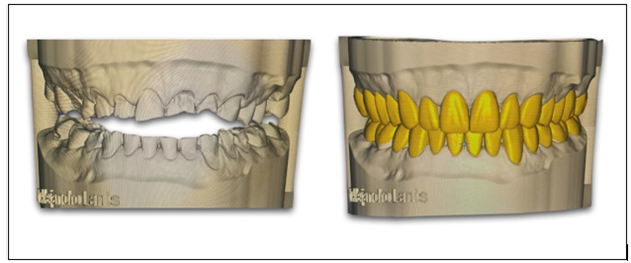
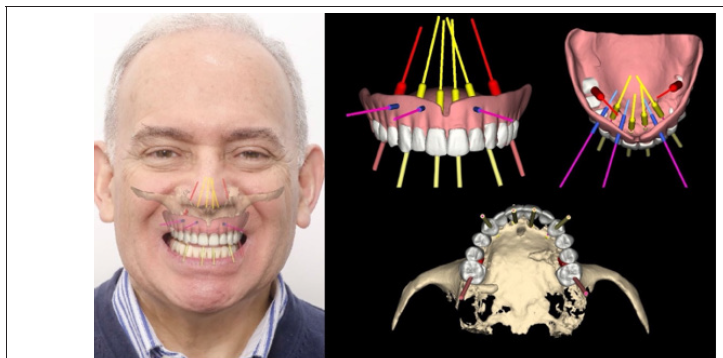
Figure 1:Digital planning for Static-Computer Assisted Immediate Implant Placement and Immediate Loading in a Full Mouth Recosntruction.
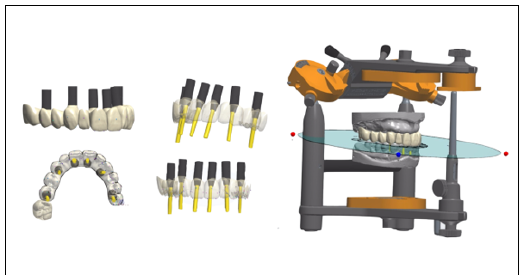
A final historical component of the modern digital dental revolution is the adoption of digital workflows by dental laboratories. The first implementation of laboratory-specific CAD/ CAM applications is also of European origin, thanks to Dr. Matts Andersson’s development of the Procera System for alumina crown copings in the 1980’s [5]. Until recently, CAD/CAM has been the predominant type of manufacturing for dental applications and has greatly expanded in recent years. To reduce manufacturing time, associated costs, and human-induced errors, laboratories have become increasingly reliant on digital technologies. In fact, milling units and 3D printers are nowadays common work equipment for daily basis production. The shift has also involved restorative materials and their indications. Clinicians are leaning towards monolithic structures and personalized abutments, making this reliance unavoidable. These factors, combined with a decreasing number of trained technicians and increasing demand for services in many countries, have led to new business models where traditional laboratories are now called milling centers or digital dental labs (Figure 3)..
Current State of Digital Workflows
To successfully meet patient needs, clinicians are required to acquire data, make a diagnosis, create a treatment plan, and then execute it to fulfill patient’s expectations. Until recently, each of these facets of patient care have been completed using traditional approaches. Even today, most dental students continue to learn the practice of dentistry using conventional solutions. It is truth that many dental principles are based in biological and physiological processes that are kept stable during time and will probably stay like that forever. However, the way we are facing and integrating them is changing dramatically. Diagnosis, planning, and treatment execution are being transformed by innovative software and hardware solutions.
There is perhaps no component more critical to providing patient care than quality data acquisition. The diagnosis, planning and outcome for a patient can only be as good as the information gathered and integrated to provide a personalized treatment. While 2D digital radiographs with intraoral sensors were an improvement over their analog counterparts with respect to data storage and radiation exposure, they were just a replacement solution. The introduction of Cone Bean Computed Tomography (CBCT) and tridimensional imaging were a giant leap forward in diagnostics and planning. Implementation and usage of CBCT technologies continues to grow, as improvements in hardware and software over the last decade have greatly increased their utility value. Practitioners have enhanced diagnostic and treatment planning abilities for endodontics [6], dental implant therapy, periodontics, prosthodontics [7], oral and maxillofacial surgery [8], TMJ treatment [9], and orthodontics [10]. While quite a heterogeneity exists in the market relative to machine capabilities, some CBCT machines are even able to capture diagnostic quality extra-oral bitewing X-rays [11] as well as facial 3D scanning. The fact that this data is integrable with files coming from intraoral scan files makes it even more useful, allowing for direct virtual treatment planning. Another reason for increased utilization in recent years is the reduction of probably the two biggest barriers to CBCT usage in the past: cost and radiation exposure [12] (Figure 4).
Impressions have long been the other critical data input source for dentists and dental laboratories. Quality impressions (and resultant cast models) are necessary not only for diagnostic purposes, but for the transference of treatment plans into reality and for the fabrication of patient prosthetic structures. Intra Oral Scanners (IOS) have been in clinical use since the 1980’s with the introduction of the CEREC system. Vast improvements were made in scanner technologies and software in the first twenty or so years, with improved fit outcomes of single unit restorations [13-15], multi-unit fixed partial structures on natural teeth and implants [16,17], and full arch implant supported restorations [18] reaching equivalence with or exceeding those fabricated with conventional methods. IOS still lagged in accuracy when compared to polyvinylsiloxane (PVS) for certain clinical applications [19], however in the last five years, these discrepancies have been eliminated for dentate impressions and largely minimized for edentulous impressions by the latest generation of IOS units and photogrammetry technology [20]. As with CBCT machines, there is also heterogeneity amongst IOS from differing manufacturers. In any case, digital impressions permit patient’s entrance to the digital world [21] and provide significant advantages over physical impressions, especially given that they don’t have a limited window of usability, don’t require any physical storage space, and integrate seamlessly into today’s digitally driven laboratory workflows [22,23] (Figures 5 & 6).

Figure 6:Extraoral photographs. Before and after treatment. Complex oral reconstruction based on osseontegrated implants. Full digital workflow
Clinical data is usually acquired in dental practice with the expressed purpose of facilitating a restorative solution for a patient. It is especially in this area that practitioners may fail to realize that some solutions are either only fabricated digitally or have the possibility for digital fabrication that meets or exceeds analog outcomes. For example, the only available workflow for monolithic zirconia crowns is a digital one, necessitating digitization of models before the crown can be designed and milled. In the future, even if these crowns are 3D printed, the workflow will stay digital. But monolithic zirconia is not the only material that can be fabricated using digital workflows. Glass ceramic restorations can be milled with comparable outcomes to pressed restorations, with some mills even able to produce a more accurate fitting than conventional pressing [24-26]. Even when laboratories still choose to press a ceramic restoration, they often do so with a 3D printed or milled castable resin wax pattern. This allows them to take advantage of the convenience of digitalization, allows for quicker recovery if there is an error in the pressing process, and leverages the cost savings of pressing several restorations out of a single ingot, as opposed to milling one restoration per block [27]. Removable partial dentures are also benefiting from the implementation of digitally fabricated frameworks [28]. For complete dentures, milling [29] and 3D printing [30] is quickly emerging as the way of the future, as it eliminates many of analog steps prone to creating error in traditional denture fabrication. Patient-specific implant solutions, from single units to full arch restorations, are most often manufactured via CAD/CAM technology in 2022. These solutions fit better than their analog counter parts [31,32], are quicker to manufacture, and less error prone than traditional fabrication methods (Figures 7 & 8).
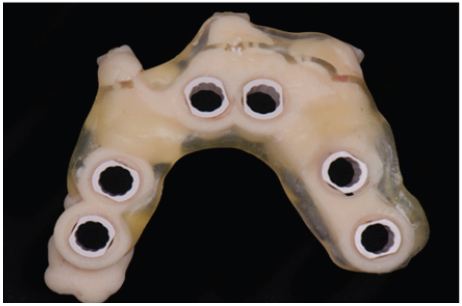
With regards to implant workflows, creating the restorative solution is far from the only thing driven by technology. By integrating CBCT and IOS data through software, implant cases can now be accurately planned virtually prior to surgery. This planning can then be transferred directly to the patient using 3D printed or milled surgical templates (Static-Computer Assisted Implant Surgery (S-CAIS)), by Dynamic Surgical Navigation (D-CIAS) or even by Robotic surgery. While guided implant therapy still has some margin of error [33], it’s already much closer to ideal than free hand implant placement [34]. The ability to integrate implant planning with a prosthetic software now allows for patientspecific restorations to be fabricated prior to surgery, facilitating the delivery of anything from a customized healing abutment, provisional restoration, or a full arch provisional restoration in a much more precise and time efficient manner than conventional chairside fabrications and denture conversions at the time of surgery (Figure 9).
Another specialty area significantly benefiting from the digital dental revolution is orthodontics [35]. 3D visualization of the TMJ, positioning of the teeth relative to the alveolar housing, and the ability to make 3D cephalometric measurements has made CBCT technology indispensable. Software developments have led to enhanced treatment planning capabilities, allowing practitioners to not only to visualize their treatment plan from start to finish, but also to see where movements take teeth relative to their bony support, transfer that treatment plan to patient-specific clear aligners or pre-shaped wires, and allows them to visually share the predicted outcome with the patient. As diagnostic models and treatment modalities become digitized, the “orthodontic lab” is also digitizing, with 3D printed models replacing plaster when a physical model is needed. With respect to the use of IOS and digital models for diagnosis and treatment planning, orthodontists already consider them the new gold standard in practice, given their accuracy and ease of storability [36].
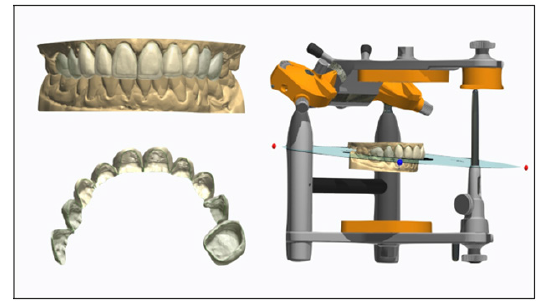
Digital workflows for esthetic smile design are not only benefiting orthodontic patients, but restorative patients as well. The ability for the patient and practitioner to “preview” a new smile before starting treatment greatly enhances communication. There are several different protocols already developed for 2D/3D smile design, all with similar goals [37-40]. While the workflow varies depending on which protocol one uses, the desired end result of digital smile design is to have a face integration to communicate to the patient and lab technician the possible treatment outcome, as well as a CAD designed mockup, which can be 3D printed to create a physical mock up to preview in the patient’s mouth prior to treatment. If the patient and clinician approve of the try in, it can be utilized as an essential tool for prep guidance. Moreover, the CAD-generated design can be directly copied to design the final restorations. If alterations are required, the patient’s arch can be re-scanned once the desired changes are made, and again that design can be directly copied to the patient’s outcome. Since all this information is gathered in a virtual platform, functionality of future restorations can also be considered and analyzed in a virtual articulator. Thanks to these techniques, it has never been more predictable to communicate and meet patient’s functional and esthetic demands and desires (Figure 10).

Figure 10:Extraoral photographs. Before and after treatment. Complete mouth reconstruction. Full digital workflow.
That is not to say that current digital technologies and workflows are perfect and without need of further development. As mentioned, several times previously in this article, a great amount of heterogeneity exists amongst digital technologies, not only with IOS and CBCT, but with software, milling machines and 3D printers. Some systems offer better accuracy, more functionality, and/or more value for dollars than others. Some digital ecosystems allow for the transference and usage of data from other platforms, aka open architecture systems, while others function only with what is generated within a particular brand, known as closed systems. While it is true that digital workflows offer several benefits, there are still plenty of instances in which digital workflows are limited in one way or another. All these variables create a challenging decision-making process for clinicians, especially given that many practitioners did not receive training in the application of digital technologies as part of their formal education. The everincreasing number of options makes it more difficult for novice and experienced clinicians alike to make the right choice regarding what technologies and digital ecosystem(s) best fit their needs [41] (Figure 11).
Emerging Technologies
Where will the profession go from here? While it would be impossible to accurately predict every development in the next 10-20 years, one thing is for certain: digital technologies will absolutely supplant the traditional workflows we as dentists have trained and practiced with for the last century. As noted above, “digital dentistry” is already providing the profession with a level of predictability and capabilities unmatched by analog workflows. Given the current scope of possibilities and existing evidence base supporting its use, it is undeniable that digital dentistry will be the new standard of care for dental patients.
When digital dentistry first emerged in the form of chairside CAD/CAM procedure, one of the biggest paradigm shifts was the condensing of a several weeks long process into a single day. The “same day crown” had obvious benefits to both the patient and practitioner. Patients received treatment in a drastically reduced time and with less opportunities for complications, while practitioners benefited from the same minimization of possible complications while improving practice efficiency and increasing future production time. This same type of workflow consolidation and improvement in efficiency is already a possibility for other types of digitally driven treatments. Given the easier access to CBCT, improvements in planning software and the ever-increasing speed of 3D printers, it is totally feasible to diagnose, plan, and provide dental implant therapy in a single visit, whether one chooses to use dynamic or static approaches. While software is still somewhat lacking for endodontic-specific applications, the same workflow (and software for that matter) could be used to access a tooth needing endodontic therapy in a guided way. Interdisciplinary cases, such as management of congenitally missing laterals postorthodontic treatment in a growing patient, can be managed with interim resin bonded fixed partial dentures, fabricated before the patient ever has brackets removed. A digital smile design mockup, once approved by the patient, could be 3D printed and tried in the same day, without the need to come back for a subsequent visit. Soon, orthodontic planning software will be robust and fast enough to plan orthodontic treatment and start a patient’s treatment the very same day, instead of needing multiple appointments to get started. As more materials are developed, 3D printers may also be used to fabricate permanent restorative solutions for patients. In summary, time, that is probably our most asset (as well as for the patient) is being considerably optimized.
Emerging technologies will eventually connect the few areas that are still with one foot in the 2D realm and one in the 3D world. Facial scanning technology, combined with existing digital formats, will make true 3D treatment planning a possibility, whether for full mouth rehabilitations or elective smile enhancement [42]. Advances in CBCT-based 4D jaw motion tracking [43,44] will truly personalize the evaluation and treatment of TMD, as well as ensure that orthodontic and restorative treatments are patient-specific for joint health and function. Non-ionizing technologies such as optical coherence tomography (OCT), ultrasound and magnetic resonance imaging (MRI) have the potential to provide 3D views of the dentition and periodontium that would greatly enhance the evaluation and monitoring of oral health [45] Artificial intelligence (AI) is also utilized now for detect and predict oral pathologies and enhance treatments outcomes based on self-learning software algorithms. The way AI will impact healthcare is still incommensurable. It seems that the virtual patient and the fully digital healthcare approach is just around the corner (Figure 12).
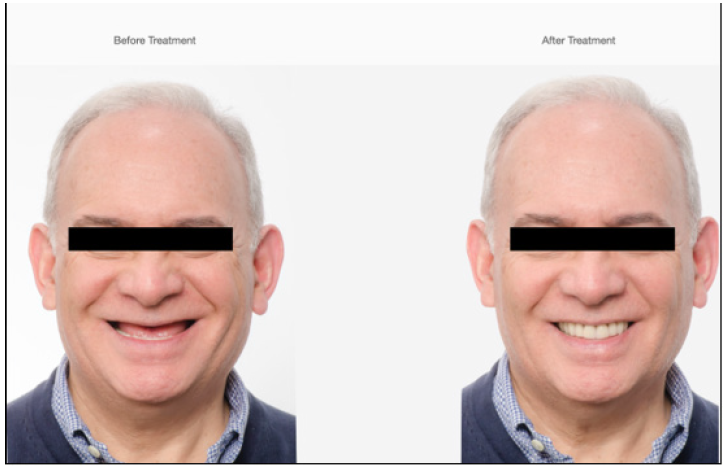
Figure 12:Extraoral photographs. Before and after treatment. Complete Mouth Reconstruction based on Osseontegrated implants. Full digital
Dentistry already is digital and will continue to fully digitize over the next 10-20 years. It will change the way we care for our patients, how our practices operate, how we communicate with colleagues and laboratories, and how we monitor our patients’ oral health over time. This situation could be based mainly on a famous statement recognized as the Moore’s Law [Gordon Moore, 1965]. In simple words, every two years technological capabilities are doubled meanwhile their price is reduced by half. Therefore, access to more powerful technology is every day easier.
However, it’s critical to remember, though, that the digital armamentarium is just that: a collection of tools and workflows to diagnose, treatment plan, and create solutions. It is not, and never will be, a replacement for well-trained, critical thinking clinicians and technicians. Digital dentistry will provide the best possibilities for patient outcomes in the history of our profession, but those outcomes will only be realized with the involvement of discerning clinicians and their teams (Figure 13).
Clinical Relevance
The most recent developments in dentistry over the last ten years ask it a question of when, not if, practitioners will adopt digital workflows and technologies. Understanding the current state of capabilities and limitations, as well as likely opportunities for future growth and development are critical in helping clinicians to decide which digital technologies and workflows are and will be necessary for their practice.
Implications for Research
Until now, most research regarding digital technologies and outcomes has centered around comparing them to conventional analog technologies and outcomes. This trend will soon be replaced by digital dentistry-related research in all facets of the profession replacing and redefining older analog approaches. There is still much work to be done to best define and refine a coherent, comprehensive set of workflows, armamentarium, and best practices for the digital workspace (Figures 14 & 15).
Conflict of Interest
No conflict of interest.
Acknowledgements
None.
References
- Duret F, Bouin JL, Duret B (1988) CAD-CAM in dentistry. J Am Dent Assoc 117(6): 715-720.
- Mörmann WH (2006) The evolution of the CEREC system. J Am Dent Assoc 137 Suppl: 7S-13S.
- Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA (1998) A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol 8(9): 1558-1564.
- Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K (1999) Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol 28(4): 245-248.
- Miyazaki T, Hotta Y, Kunii J, Kuriyama S, Tamaki Y (2009) A review of dental CAD/CAM: current status and future perspectives from 20 years of experience. Dent Mater J 28(1): 44-56.
- Patel S, Brown J, Pimentel T, Kelly RD, Abella, F, et al. (2019) Cone beam computed tomography in Endodontics - a review of the literature. International Endo J 52(8): 1138-1152.
- Rios HF, Borgnakke WS, Benavides E (2017) The Use of Cone-Beam Computed Tomography in Management of Patients Requiring Dental Implants: An American Academy of Periodontology Best Evidence Review. J Periodontol 88(10): 946-959.
- Assouline SL, Meyer C, Weber E, Chatelain B, Barrabe A, et al. (2020) How useful is intraoperative cone beam computed tomography in maxillofacial surgery? An overview of the current literature. Int J Oral Maxillofac Surg 50(2): 198-204.
- Larheim TA, Abrahamsson AK, Kristensen M, Arvidsson LZ (2015) Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol 44(1): 20140235.
- Kapila SD, Nervina JM (2015) CBCT in orthodontics: assessment of treatment outcomes and indications for its use. Dentomaxillofac Radiol 44(1): 20140282.
- Chan M, Dadul T, Langlais R, Russell D, Ahmad M (2018) Accuracy of extraoral bite-wing radiography in detecting proximal caries and crestal bone loss. J Am Dent Assoc 149(1): 51-58.
- Ludlow JB, Timothy R, Walker C, Hunter R, Benavides E, et al. (2015) Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol 44(1): 20140197.
- Chochlidakis KM, Papaspyridakos P, Geminiani A, Chen CJ, Feng IJ, et al. (2016) Digital versus conventional impressions for fixed prosthodontics: A systematic review and meta-analysis. J Prosthet Dent 116(2): 184-190.
- Tsirogiannis P, Reissmann DR, Heydecke G (2016) Evaluation of the marginal fit of single-unit, complete-coverage ceramic restorations fabricated after digital and conventional impressions: A systematic review and meta-analysis. J Prosthet Dent 116(3): 328-335.
- Ahlholm P, Sipilä K, Vallittu P, Jakonen M, Kotiranta U (2018) Digital Versus Conventional Impressions in Fixed Prosthodontics: A Review. J Prosthodont 27(1): 35-41.
- Lo Russo L, Caradonna G, Biancardino M, De Lillo A, Troiano G, et al (2019) Digital versus conventional workflow for the fabrication of multiunit fixed prostheses: A systematic review and meta-analysis of vertical marginal fit in controlled in vitro studies. The J Prosthet Dent 122(5): 435-440.
- Su TS, Sun J (2016) Comparison of marginal and internal fit of 3-unit ceramic fixed dental prostheses made with either a conventional or digital impression. J Prosthet Dent 116(3): 362-367.
- Wulfman C, Naveau A, Rignon Bret C (2020) Digital scanning for complete-arch implant-supported restorations: A systematic review. J Prosthet Dent 124(2): 161-167.
- Ender A, Attin T, Mehl A (2016) In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J Prosthet Dent 15(3): 313-320.
- Mennito AS, Evans ZP, Nash J, Bocklet C, Lauer Kelly A, et al. (2019) Evaluation of the trueness and precision of complete arch digital impressions on a human maxilla using seven different intraoral digital impression systems and a laboratory scanner. J Esthet Restor Dent 31(4): 369-377.
- Lanis A, Llorens P, Alvarez del Canto O (2017) Selecting the appropriate digital-planning pathway for computer guided implant surgery. Int J Comput Dent 20(1): 75-85.
- Lanis A, Alvarez Del Canto O (2015) The combination of digital surface scanners and cone beam computed tomography technology for guided implant surgery using 3 Shape Implant Studio Software: a case history report. Int J Prosthodont 28(2): 169-178.
- Stevens CD (2020) Impression-Making in 2020: How Long Before Analog Methods Are Obsolete?. Compend Contin Educ Dent 41(3): 178-179.
- Alfaro DP, Ruse ND, Carvalho RM, Wyatt CC (2015) Assessment of the Internal Fit of Lithium Disilicate Crowns Using Micro-CT. J Prosthodont 24(5): 381-386.
- Anadioti E, Aquilino SA, Gratton DG, Holloway JA, Denry IL, et al. (2015) Internal fit of pressed and computer-aided design/computer-aided manufacturing ceramic crowns made from digital and conventional impressions. J Prosthet Dent 113(4): 304-309.
- Elrashid AH, AlKahtani AH, Alqahtani SJ, Alajmi NB, Alsultan FH (2019) Stereomicroscopic Evaluation of Marginal Fit of E.Max Press and E.Max Computer-Aided Design and Computer-Assisted Manufacturing Lithium Disilicate Ceramic Crowns: An In vitro Study. J Int Soc Prev Community Dent 9(2): 178-184.
- Johnson R, Verrett R, Haney S, Mansueto M, Challa S (2017) Marginal Gap of Milled versus Cast Gold Restorations. J Prosthodont 26(1): 56-63.
- Campbell SD, Cooper L, Craddock H, Hyde TP, Nattress B, et al. (2017) Removable partial dentures: The clinical need for innovation. J Prosthetic Dent 118(3): 273-280.
- Lo Russo L, Salamini A (2018) Removable complete digital dentures: A workflow that integrates open technologies. J Prosthet Dent 119(5): 727-732.
- Cristache CM, Totu EE, Iorgulescu G, Pantazi A, Dorobantu D, et al. (2020) Eighteen Months Follow-Up with Patient-Centered Outcomes Assessment of Complete Dentures Manufactured Using a Hybrid Nanocomposite and Additive CAD/CAM Protocol. J Clin Med 9(2): 324.
- Abduo J (2014) Fit of CAD/CAM implant frameworks: a comprehensive review. J Oral Implantol 40(6): 758-766.
- Abduo J, Yin L (2019) Fits of Implant Zirconia Custom Abutments and Frameworks: A Systematic Review and Meta-Analyses. Int J Oral Maxillofac Implants 34(1): 99-114.
- Tahmaseb A, Wu V, Wismeijer D, Coucke W, Evans C (2018) The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin Oral Implants Res 29(Suppl 16): 416-435.
- Chen CK, Yuh DY, Huang RY, Fu E, Tsai CF, et al. (2018) Accuracy of Implant Placement with a Navigation System, a Laboratory Guide, and Freehand Drilling. Int J Oral Maxillofac Implants 33(6): 1213-1218.
- Jheon AH, Oberoi S, Solem RC, Kapila S (2017) Moving towards precision orthodontics: An evolving paradigm shift in the planning and delivery of customized orthodontic therapy. Orthod Craniofac Res 20(Suppl 1): 106-113.
- Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL (2016) Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review. Am J Orthod Dentofacial Orthop149(2): 161-170.
- Brenes C, Jurgutis L, Babb CS (2018) Digital face-bow transfer technique using the dentofacial analyzer for dental esthetics and 2-D, 3-D smile design: A clinical report. Journal of Oral Science and Rehabilitation 4(2): 22-30.
- Coachman C, Calamita MA, Sesma N (2017) Dynamic documentation of the smile and the 2D/3D digital smile design process. Int Journal Periodontics Restorative Dent 37(2): 183-193.
- Silva BP, Mahn E, Stanley K, Coachman C (2019) The facial flow concept: an organic orofacial analysis-the vertical component. J Prosthet Dent 121(2): 189-194.
- Zimmermann M, Mehl A (2015) Virtual smile design systems: a current review. Int J Comput Dent 18(4): 303-317.
- Stevens CD (2020) Impression-Making in 2020: How Long Before Analog Methods Are Obsolete? Compend Continuing Educ Dent 41(3): 178-179.
- Mangano C, Luongo F, Migliario M, Mortellaro C, Mangano FG (2018) Combining Intraoral Scans, Cone Beam Computed Tomography and Face Scans: The Virtual Patient. J Craniofacial Surg 29(8): 2241-2246.
- Aslanidou K, Kau CH, Vlachos C, Saleh, TA (2017) The fabrication of a customized occlusal splint based on the merging of dynamic jaw tracking records, cone beam computed tomography, and CAD-CAM digital impression. J Orthod Sci 6(3): 104-109.
- Kwon JH, Im S, Chang M, Kim JE, Shim JS (2019) A digital approach to dynamic jaw tracking using a target tracking system and a structured-light three-dimensional scanner. J Prosthodont Res 63 (1): 115-119.
- Elashiry M, Meghil MM, Arce RM, Cutler CW (2019) From manual periodontal probing to digital 3-D imaging to endoscopic capillaroscopy: Recent advances in periodontal disease diagnosis. J Periodontal Res 54(1): 1-9.








 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.