Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Research progress of the Vessel-Collateral Theory and Organ Fibrosis
*Corresponding author: Da-Peng Wang, Department of Nephrology, the first affiliated Hospital, Dalian Medical University, Dalian, China.
Received: August 23, 2022; Published: August 29, 2022
DOI: 10.34297/AJBSR.2022.17.002304
Abstract
The Vessel-Collateral Theory is a kind of disease model theory in Traditional Chinese Medicine, that describes changes in the vascular microenvironment and microcirculatory disorders. According to this theory, the body’s qi and blood run through the channels of meridians to infuse all organs and tissues of the body. And when this channel is affected by various pathological factors, its function is impaired. Fibrosis is a common pathological pathway for liver, kidney, lung and other organs to progress to end-stage diseases. Microcirculation is a place where blood, material metabolism and energy exchange are carried out by microvessels as the main structure; at the structural level, modern medicine considers microcirculation as having the characteristics of network structure, diffuse distribution, mutual penetration and fluid flow. A number of studies have confirmed that organ fibrosis is associated with sclerosis, rarefaction and decreased perfusion of the capillary network. This alteration in the vascular microenvironment is similar to the Vessel-Collateral Theory, which is called Accumulation in category of traditional Chinese medicine. The formation of accumulation is closely related to the Qi and Blood in the meridians. A variety of pathogenic factors affect the transit of Qi and Blood, causing collateral disease and eventually the accumulation of organ fibrosis. Many herbal prescriptions formed under the guidance of Vessel-Collateral Theory all work by activating blood circulation and are related to improving microcirculation, so we do an overview to dig more single and compound prescriptions to improve organ fibrosis.
Keywords: Chinese medicine, Herbal prescriptions, Chinese herbal monomer, the Vessel-Collateral Theory, Organ fibrosis.
Introduction
The Vessel-Collateral Theory first originated in the Qing Dynasty, when Ye Tianshi proposed this concept in Linzheng Zhinan Yi’an. Professor Yiling Wu inherited the traditional meridian theory and systematically constructed the Vessel-Collateral Theory to guide the prevention and treatment of vasculopathy [1]. He also proposed the concept of “vessel-vascular system diseases” based on the close correlation between collaterals and micro vessels. The collateral, as the main pathway for the transmission of qi, blood and fluid to realize the basic function and biochemical at the end of the veins, has the characteristics of network structure, diffuse distribution, bi-directional flow, and slow movement. Corresponding to collateral, the microcirculation theory under modern medical research believes that the microvessel is the main structure to carry out blood operation, material metabolism and energy exchange. According to the Vessel-Collateral. Theory, the tangible vessels of the internal organs form the vessel collaterals (blood), while the neuroendocrine immune regulation function formed by the cell signaling in the internal organs constitutes the invisible meridian collaterals (qi), and both qi and blood collaterals together complete the physiologic functions of “circulating qi and blood as well as nourishing yin and yang.” In modern medical theory, organ-specific microvascular endothelial cells, pericytes and surrounding blood cells in multiple organs including kidney constitute a relatively independent microcirculatory whole, forming a guiding microenvironment called vascular niche, and the destruction of vascular niche is closely related to organ fibrosis. Therefore, the concept of “callateralmicrovessel” was proposed based on the similarity of functions and structures of callaterals and microvessels, the treatment of fibrosis according to this theory is to treat the collateral-qi stagnation or deficient stagnation, as well as the pathological products such as phlegm, stasis and heat through the vessel-vascular system diseases by using the herbs and prescriptions, which is a combination of Chinese and Western medicine to study the theory of microvascular lesions.
Fibrosis is a protective mechanism that follows inflammation and tissue injury by cells invading the injured area secrete large amounts of extracellular matrix to reconstruct and strengthen the damaged tissue to accelerate the healing process [2]. Based on this, we propose that the vascular niche is the basic structure of organ ligaments including the kidney and is a good entry point for modern research in ligamentology. Common mechanisms involved in fibrosis include the TGF/Smads pathway [3], some inflammatory signaling pathways such as Wnt/β-catenin, MAPK, NF-κB, PI3K/Akt, and JAK-STAT pathways [4-8], the CXCL12-CXCR4/CXCR7 pathway [9], the endothelial-to-mesenchymal transformation(EMT), and the epithelial mesenchymal transition(EMT) [10,11], as well as the regulation of some inflammatory mediators and cytokines such as hypoxia-inducible factor-1 (HIF-1),peroxisome proliferatoractivated receptors (PPAR-γ), IL-10,IL-13, IL-21, TGF-β1, chemokines (MCP-1, MIP-1beta), angiogenic factors (VEGF), growth factors (PDGF), acute phase proteins (SAP), caspases, and components of the renin-angiotensin-aldosterone system (ANG II) [12-15]. The cells involved in these mechanisms include parenchymal cells of organs, vascular endothelial cells, pericytes, epithelial cells, myofibroblasts, and various immune cells [16-18].
According to current studies on the pathogenesis of organ fibrosis, the development of fibrosis is accompanied by a series of vascular changes, such as the rarefaction of peritubular capillaries [19], the defective repair of capillaries after injury [20], and divergent angiocrine signals from vascular niche [21], these factors result the proliferation of fibroblasts around blood vessels. During the progression of fibrosis, as changes in vascular tone, endothelial permeability and vascular regulation lead to inflammation, hypertension and coagulation, thus gas, solute and hormone exchange between blood and tissues is affected, subsequently affecting angiogenesis and remodeling [22,23]. Therefore, targeting the microvascular environment of injured tissues may mitigate fibrosis. Under the guidance of the Vessel-Collateral Theory, many prescriptions and Chinese medicines as well as their individual components are being studied, and these approaches have comprehensively elucidated the clinical application of Vessel- Collateral Theory from the perspective of molecular biology, such as “Dahuang Zhechong pill (DHZC)”, “Buyang Huanwu decoction (BYHW)”, “Qili Qiangxin capsule (QLQX)”, “Xuefu Zhuyu soup (XFZY)”, “Naoxintong capsule (NXT)” and so on. These prescriptions show good efficacy in the clinical application of organ fibrosis. Therefore, it is a good supplement and alternative to use the theory and methods of Vessel-Collateral Theory in treating fibrosis. Based on the above reasons, we summarized the Chinese medicine and prescriptions for the treatment of organ fibrosis based on the Vessel-Collateral Theory.
Pulmonary Fibrosis
“Buyang Huanwu decoction (BYHW)” studied by collateral disease can reduce the expression of connective tissue growth factor (CTGF) and phosphor-AKT (p-AKT) to alleviate pulmonary fibrosis in rats and can also regulate the PI3K-Akt-ENOS pathway to improve pulmonary vascular remodeling [24,25]. LHQW has an antagonistic effect on the pro-inflammatory mediator’s TNF-α and IL-6 of the mechanism and reduce the degree of endothelialmesenchymal transition (EndMT) and fibrosis [26,28]. In addition, Tetramethylpyrazine(TMP), one of TCM monomers, regulated the SDF-1/CXCR4 pathway to inhibit angiogenesis or fibrosis, and inhibited the apoptosis of pulmonary microvascular endothelial cells (PMVEC) by the PERK/eIF2α/ATF4/CHOP apoptotic signal for improving microcirculation disorders and alleviating lung injury [29,30]. Astragaloside IV can inhibit TGF-β1/Smad2/3 signaling pathway, reduce the expression of collagen I, fibronectin (FN) and α-SMA, improve pulmonary vascular remodeling and alleviate pulmonary fibrosis [31,32]. Studies show that quercetin, gambogic acid, dihydroartemisinin(DHA) can effectively inhibit TGF-β- mediated endothelial cell proliferation and EndMT in lung and skin fibrosis models [33]. Salvianolic acid B (Sal B) protected endothelial cells from oxidative stress by inhibiting endothelial cell permeability and reducing the expression of pro-inflammatory cytokines through MAPK and NF-κB signaling pathways and improves LPS-induced rat pulmonary microcirculation disorders [34,35]. Maxing Shigan Tang MXSGT ameliorated LPS-induced leukocytosis in pulmonary small veins of rats, and effectively inhibited the production of proinflammatory factors and pulmonary perivascular edema, which shows that MXSGT has potential therapeutic effects on pulmonary microvascular hyperpermeability and inflammatory responses [36]. Pretreatment with andrographolide pills (AP) ameliorate LPSinduced increase in cytokines, neutrophil adhesion and infiltration, oxidative stress and microvascular hyperpermeability [30]. Schisandrin (Sch), the active component of Schisandra chinensis, can attenuate LPS-induced lung endothelial and epithelial cell injury, reduce expression of vascular heme factor (vWF) and keratin, and activate cell regeneration possibly through inhibition of TLR-4/ NF-κB/MAPK activation and FoxO1 signaling pathway [37].
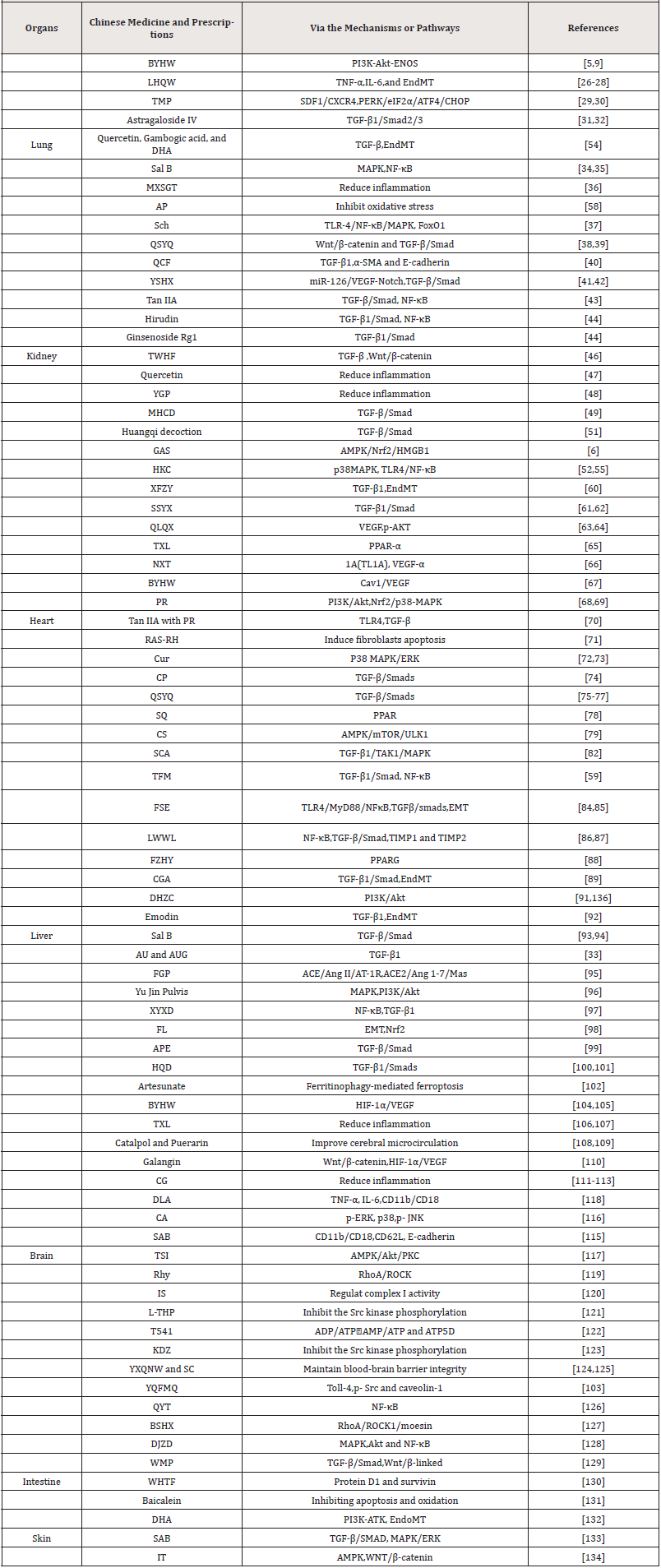
Table 1: Chinese Medicine and Prescriptions inhibit fibrosis and inflammation through various pathways in different organs.
Renal Fibrosis
The TGF/Smad pathway is the classical pathway of fibrosis mechanism and is capable of causing mesenchymal changes in a variety of cells. In view of this, collateral disease prescriptions including Qishen Yiqi pill (QSYQ), Quyu Chencuo prescription (QCF) and Yishen Huoxue prescription (YSHX) have antagonistic effect on this mechanism. QSYQ is a renal protective prescription, that can inhibit EndMT by Wnt/β -catenin and TGF-β/Smad signaling pathways, thus improve renal microcirculation disorders, prevent diabetic nephropathy and alleviate renal fibrosis [38,39]. QCF, as one of the Traditional Chinese medicine TCM prescriptione that can improve blood circulation, has been proved to improve renal interstitial microvascular environment and prevent the progression of renal fibrosis by regulating the expression of TGF-β1, α-SMA and E-cadherin in UUO rats [40]. YSHX can mediate renal microvasculogenesis and improve renal microvascular injury by upregulating miR-126/VEGF-Notch signaling pathway, and also inhibit TGF-β/Smad signal transduction, both of which can alleviate renal fibrosis [41,42]. In addition, tanshinone IIA (tan IIA) can reduce the levels of inflammation and fibrosis and ameliorate the disturbance of microvascular environment by inhibiting the activation of TGF-β/Smad and NF-κB signaling pathways in CKD rats [43]. Hirudin can inhibit renal fibrosis by blocking TGF-β1/ Smad and NF-κB pathways [44]. The treatment of ginsenoside Rg1 in combination with astragaloside IV can protect against microangiopathy in diabetic nephropathy by reducing oxidative stress and inhibiting TGF-β1/Smads signaling [45]. The anti-fibrosis effect of Tripterygium wilfordii Hook F (TWHF) is to ameliorate the microvascular injury of diabetic nephropathy by inhibiting TGF-β and Wnt/β-catenin signals [46]. Quercetin can not only inhibit the infiltration of M1 macrophages in renal interstitium and reduce inflammation, but also inhibit the activation of M2 macrophages and reduce the excessive accumulation of extracellular matrix, thus achieving the effect of treating renal interstitial fibrosis [47]. Yougui Pill (YGP) is a traditional prescription that has been widely used to “warm the kidney”. Experiments show that YGP significantly reduce UUO-induced inflammatory cell infiltration, tubular atrophy and interstitial fibrosis [48]. Modified Huangqi Chifeng Decoction (MHCD) can inhibit secretion of extracellular matrix from glomerular thylakoid cells induced by inflammatory factor, suppress excessive activation of TGF-β/Smad signaling pathway thereby inhibiting fibrosis [49,50]. Huangqi decoction can dosedependently downgrade the expression of collagen and inhibit the activation of TGF-β/Smad signaling pathway to improve ipsilateral renal fibrosis in UUO mice [51]. Gastrodin (GAS), the main phenolic glycoside extracted from Gastrodia elata Blume, was found that can attenuate CCl(4)-induced kidney inflammation and fibrosis via the AMPK/Nrf2/HMGB1 pathway [6]. Huangkui capsule (HKC) is an anti-inflammatory Chinese modern patent medicine. Studies showed that HKC can alleviate renal fibrosis by suppressing the activation of p38MAPK signaling pathway and inhibiting NLRP3 inflammasome activation and TLR4/NF-κB signaling pathways in the DN model rats [52-55].
Cardiac Fibrosis
Endothelial cells have the ability to convert to a smooth muscle-like phenotype, and the phenotypic transition is termed Endothelial-to-mesenchymal-transition (EndMT), which is a common mechanism in the process of organ fibrosis [56,57]. The prescription XFZY applied in collateral diseases can inhibit EndMT and fibroblast activation through TGF-β1 signaling pathway and improve myocardial fibrosis [58-60]. Shensong Yangxin capsule (SSYX) can inhibit TGF-β1/Smad signaling pathway, reduce fibrosis and improve cardiac function [61,62]. In addition, Qiliqiangxin Capsules (QLQX) can correct cardiac dysfunction and ventricular remodeling by upregulating VEGF expression and Akt phosphorylation, and its protective effect may be related to reduced apoptosis and myocardial fibrosis [63,64]. Tongxinluo (TXL) activates Angiopoietin-like 4 (Angptl4) under the regulation of PPAR-α pathway to maintain the functional and structural integrity of the endothelial barrier and protect the heart from I/R injury in diabetic rats [65]. Naoxintong capsule (NXT) has a variety of anti-thrombotic functions and can reduce the apoptosis of HUVECs by inhibiting the expression of tumor necrosis factor-like cytokine 1A(TL1A) and activating the expression of VEGF-α [66]. BYHW can reduce myocardial fibrosis and inflammation through Cav1/VEGF signaling pathway, so that can promote angiogenesis in infarct boundary area [67]. Puerarin (PR) can weaken EndMT and inhibit the activation of PI3K/Akt pathway by reactive oxygen species, so as to decelerate cardiac fibrosis [68]. PR can also rescue injured endothelial cells, improve repair function of vascular niche and prevent myocardial fibrosis by activating Nrf2 expression and inhibiting phosphorylation of p38-MAPK [69]. In addition, tan IIA combined with PR can reduce the expression of TLR4 and TGF-β, protect vascular endothelial cells, improve hemodynamics and vascular permeability, and inhibit myocardial fibrosis and ventricular remodeling [70]. Radix Angelica Sinensis and Radix Hedysari ultrafiltration extract (RAS-RH) can induce apoptosis, inhibit the levels of TGF-β1 and troponin-1(TnI), and reduce the expression of osteopontin (OPN), C-Jun, mirNA-21 and COL1α in fibroblasts, thus playing an anti-fibrosis role [71]. Curcumin (Cur) can inhibit the P38 MAPK/ERK signaling pathway to regulate the proliferation and cell cycle of cardiac fibroblasts, so as to inhibit abnormal growth of microvessels, and reduce cardiac fibrosis [72,73]. Cardiotonic pills (CP) improved myocardial fibrosis and prevented myocardial remodeling by inhibiting the expression of TGF-β1, P-Smad3, Smad4, MMP-9, α-SMA and CD68-positive cell number in rats I/ R-induced to myocardial infarction and fibrosis [74]. QiShen YiQi Pills (QSYQ) can reduce myocardial fibrosis by inhibiting the TGFβ1/Smads signaling pathways and prevent ischemic myocardial injury by inhibiting the release of myocardial cTnI and restoring energy-regulated metabolism after myocardial ischemia [75-77]. Sang-qi Granula (SQ) is a proprietary Chinese medicine. It was found that SQ could significantly inhibit the expression of proinflammatory mediators and collagen depositation-related proteins in SHR rat cardiomyocytes and prevent cardiac fibrosis through PPAR signaling pathway [78]. Chikusetsusaponin IVa (CS) was demonstrated that can attenuate isoprenaline-induced myocardial fibrosis by activating autophagy through AMPK/mTOR/ULK1 pathway, reduce the heart index, inhibit inflammatory infiltration, and decrease collagen deposition and myocardial cell size [79].
Hepatic Fibrosis
Hepatic microcirculatory dysfunction is a key factor in causing chronic liver disease and liver fibrosis. The disruption of vascular homeostasis leads to portal hypertension, which is an important cause of compromising the liver [80,81]. Schisandra chinensis (SCA) is a traditional Chinese medicine for liver protection, and it was showed that SCA can ameliorate the liver fibrosis by inhibiting the HSCs activation and inflammatory response and inhibiting TGF-β1 mediated TAK1/MAPK signal pathways [82]. Additionaly, the main active components of SCA, schisandrin C (Sin C) and Schisandrol B (SolB) was also found to have the effect of reversing liver fibrosis in mice [8,24,83]. Total flavonoids of Mallotus apelta leaf (TFM) can alleviate CCl(4)-induced hepatic fibrosis in rats by reducing ECM accumulation, improving antioxidant and regulating TGF-β1/ Smad signaling pathways and NF-κB-dependent inflammatory response [59]. The water-soluble component extracted from Forsythiae Fructuse, Forsythiae Fructuse water extract (FSE), can inhibit the development of liver fibrosis through TLR4/MyD88/ NF-κB and TGF-β/smads signaling pathways. In vivo, studys showed FSE attenuated CCl(4)-induced liver fibrosis in mice by inhibiting hepatic stellate cells (HSCs) activation, reducing hepatic extracellular matrix (ECM) disposition and reversing epithelialmesenchymal transition (EMT) [84,85]. There are results indicated that Liuweiwuling (LWWL) tablets, a Chinese traditional herbal prescription, can attenuate hepatic fibrosis in rats by modulating the NF-κB-dependent inflammatory response and TGF-β/Smad signaling pathway, as well as the expression levels of TIMP1 and TIMP2, which regulate extracellular matrix (ECM) degradation [86,87].
Fuzheng Huayu prescription (FZHY) have been found that its main active ingredients can directly bind to peroxisome proliferatorsactivator receptor PPARG to reduce the activities of HSCs, thus playing an anti-fibrosis role [88]. The prescription CGA is modified from FZHY. CGA can inhibit EndMT by antagonizing TGF-β1/Smad signaling pathway, so as to reverse the transformation of HSCs into myofibroblasts and alleviate liver fibrosis [89,90]. DHZC can play a role of anti-fibrosis in liver, which can not only inhibit macrophage recruitment to hepatocyte and reduce the accumulation of collagen in liver tissue, but also inactivate PI3K/Akt pathway for inhibiting the proliferation of HSCs [91,136]. Additionally, emodin may reduce EndMT by inhibiting TGF-β1 signaling pathway and play an antiliver fibrosis role [92]. Sal B is a potential anti-liver fibrosis drug by inhibiting TGF-β/Smad signaling [93,94]. Aucubin (AU) and Aucubigenin (AUG), as active ingredients of eucommia ulmoides, can inhibit the activation of HSCs and ECM deposition induced by TGF-β1, so that they restore the disturbed microvascular microenvironment [33]. Fugan pill (FGP) can repair endothelial dysfunction and alleviate liver fibrosis by inhibiting ACE/Ang II/AT- 1R signaling pathway and enhancing ACE2/Ang 1-7/Mas signaling pathway [95]. Yu Jin Pulvis has anti-fibrosis effect on CCL4-induced mice by blocking MAPK and PI3K/Akt signaling pathways [96]. Xiayu- xue decoction (XYXD), a classical Collateral recipe used in China, was revealed to inhibit hepatic fibrosis by inhibiting HSC activation via inhibition of NF-κB and TGF-β1 signaling pathway [97]. The water extract of Lonicerae Japonicae Flos (FL) from carbon tetrachloride can attenuate CCl(4)-induced liver fibrosis in mice by inhibiting HSCs activation, reversing EMT and reducing liver oxidative stress injury via inducing Nrf2 activation [98]. Astragalus and Paeoniae radix rubra extract (APE) may inhibit the progression of CCl4‑induced hepatic fibrosis via scavenging free radicals, decreasing TGF‑β1 levels and blocking of the TGF‑β/Smad signaling pathway [99]. Huangqi decoction (HQD) can alleviate DMN-induced liver fibrosis via the regulation of bile acid metabolism enzyme and inhibit CDCA-induced HSCs proliferation and activation. Moreover, the main components of HDQ, the total astragalus saponins (AST) and glycyrrhizic acid (GA), synergistically alleviated hepatic fibrosis via TGF-β1/Smads signaling pathway inhibition in hepatic stellate cells [100,101]. Artesunate, a water-soluble hemisuccinate derivative of artemisinin, could alleviate liver fibrosis by regulating ferritinophagy-mediated ferroptosis in hepatic stellate cells (HSCs) [102, 103].
Other Organ Fibrosis
Studies also found some Vessel-Collateral Theory treatment methods that can inhibit organ fibrosis in brain, intestine, skin and other organs by repairing vascular endothelial cell injury and improving the microcirculation. For example, BYHW can prevent reperfusion injury after ischemic stroke in rats by inhibiting HIF-1α and VEGF, promoting angiogenesis and repairing brain tissue [104,105]. Tongxinluo capsule (TXL) can improve ischemic cerebrovascular disease by inhibiting inflammatory response, regulating vascular endothelial function and promoting angiogenesis [106,107]. Lyophilized Powder of Catalpol and Puerarin can improve cerebral microcirculation disorders and neurological recovery after cerebral ischemia by promoting vascular renewal [108,109]. Galangin promotes vascular neogenesis and vascular remodeling through upregulation of Wnt/β-catenin and HIF-1α/VEGF signaling pathways in MCAO model rats [110]. Cerebral care Granule (CG) is a compound Chinese medicine used to treat headache and dizziness associated with cerebrovascular diseases. It was found that CG treatment could significantly reduce microvascular ultrastructural changes in the cerebral cortex of gerbils caused by I/R injury, reduce cerebral microvascular hydrogen peroxide production, leukocyte adhesion and albumin leakage, significantly reduce blood-brain barrier permeability and brain edema, and reduce brain neuronal damage [111-114]. The active monomer components of Salvia miltiorrhiza, such as 3,4-dihydroxyphenyl lactic acid (DLA), CA, Salvianolic acid B(SAB) and Total salvianolic acid injection (TSI), can also improve cerebral microvascular hyperpermeability and inhibit thrombogenesis through anti-inflammatory and antioxidant effects [115-118]. In addition, there are many prescription and herbs as well as single components that can improve perfusion and salvage cerebrovascular and neurological damage by inhibiting vascular endothelial cell injury and cerebral microcirculatory dysfunction, such as some components of herbs: Rhynchophylline(Rhy) [119], Icariside II (IS) [120], Levo-tetrahydropalmatine(L-THP) [121], herbal monomer complex T541(AS:SAA:PNS=5:4:1) [122] and some prescriptions: Kudiezi Injection(KDZ) [123], YangXue QingNao Wan(YXQNW) and Silibinin Capsules(SC) [124,125], Yiqifumai injection(YQFMQ)[102], Qing-Ying-Tang(QYT)[126], Bushen Huoxue(BSHX) [127]. All these methods play a positive role in treating fibrosis from the perspective of Vessel-Collateral Theory.
Dajianzhong decoction (DJZD) improves intestinal fibrosis and induces intestinal blood flow by regulating mitogen-activated protein kinase (MAPK), protein kinase B (Akt) and NF-κB activity [128]. Wumei pill (WMP) inhibit intestinal fibrosis and alleviate chronic colitis by regulating TGF-β/Smad and Wnt/β-linked protein pathways [129]. Dermal fibrosis is a major pathological change in systemic sclerosis (SSc), and Wenyang Huazhuo Tongluo prescription (WHTF) may exert anti-proliferative and pro-apoptotic effects on fibroblasts by downregulating mRNA and protein levels of protein D1 and survivin in SSc cells [130]. Baicalein from Scutellaria baicalensis is able to promote flap viability by stimulating angiogenesis and inhibiting apoptosis and oxidation [131]. Dihydroartemisinin (DHA) inhibits fibroblast activation and collagen deposition via the PI3K-ATK pathway to ameliorate tissue fibrosis and protects dermal vasculature from bleomycininduced EndoMT [132]. SAB can alleviate skin fibrosis and reduce collagen deposition in blomycin-induced SSc mouse model, reduce SSc skin fibroblast proliferation through TGF-β/SMAD and MAPK/ ERK pathways, and down-regulate extracellular matrix gene transcription and collagen expression [133]. Icaritin (IT), a natural compound of epimedium herb, was found to have an anti-skin fibrotic effect through activation of AMPK signaling and inhibition of WNT/β-catenin signaling [134].
Discussion
The above studies suggested that various TCM and monomer ingredients could inhibit abnormal activation of vascular microenvironment signaling pathways in different organs to repair microcirculation, thus achieving anti-inflammatory and antifibrosis effects (Table1). It is especially worth pointing out that TCM prescriptions of collateral medicine can play a multi-level and multi-target role in the intervention the progression of fibrosis and protection of blood circulation system. New data from the COVID-19 pandemic suggest that there may be substantial fibrotic consequences following SARS-CoV-2 infection [135]. Thus, current therapies targeting fibrosis have value in the prevention and treatment of chronic lesions of the post-infected organ. Therefore, by studying the treatment of fibrosis with herbal compound and monomeric components under the collateral disease theory can bring richer experience for the treatment of fibrosis.
References
- Wu Y (2011) Construction of the vessel-collateral theory and its guidance for prevention and treatment of vasculopathy. Front Med 5(2): 118-122.
- Di Carlo SE, Peduto L (2018) The perivascular origin of pathological fibroblasts. J Clin Invest 128(1): 54-63.
- Meng XM, Nikolic Paterson DJ, Lan HY (2016) TGF-β: the master regulator of fibrosis. Nat Rev Nephrol 12(6): 325-338.
- Burgy O, Königshoff M (2018) The WNT signaling pathways in wound healing and fibrosis. Matrix Biol 68-69: 67-80.
- Li H, Wang Z, Zhang J, Wang Y, Yu C, et al. (2018) Feifukang ameliorates pulmonary fibrosis by inhibiting JAK-STAT signaling pathway. BMC Complement Altern Med 18(1): 234.
- Ma JQ, Sun YZ, Ming QL, Tian ZK, Zhang YJ, et al. (2020) Effects of gastrodin against carbon tetrachloride induced kidney inflammation and fibrosis in mice associated with the AMPK/Nrf2/HMGB1 pathway. Food Funct 11(5): 4615-4624.
- Yao Q, Wu Q, Xu X, Xing Y, Liang J, et al. (2020) Resveratrol Ameliorates Systemic Sclerosis via Suppression of Fibrosis and Inflammation Through Activation of SIRT1/mTOR Signaling. Drug Des Devel Ther 14: 5337-5348.
- Dai W, Qin Q, Li Z, Lin L, Li R, et al. (2021) Curdione and Schisandrin C Synergistically Reverse Hepatic Fibrosis via Modulating the TGF-β Pathway and Inhibiting Oxidative Stress. Front Cell Dev Biol 9: 763864.
- Chen Y, Cui L, Wang C, Liu J, Guo J (2021) Ameliorative Effects and Mechanism of Buyang Huanwu Decoction on Pulmonary Vascular Remodeling: Network and Experimental Analyses. Oxid Med Cell Longev 2021: 4576071.
- Yu W, Liu Z, An S, Zhao J, Xiao L, et al. (2014) The endothelial-mesenchymal transition (EndMT) and tissue regeneration. Curr Stem Cell Res Ther 9(3): 196-204.
- Stone RC, Pastar I, Ojeh N, Chen V, Liu S, et al. (2016) Epithelial-mesenchymal transition in tissue repair and fibrosis. Cell Tissue Res 365(3): 495-506.
- Wynn TA (2008) Cellular and molecular mechanisms of fibrosis. J Pathol 214(2): 199-210.
- Lokmic Z, Musyoka J, Hewitson TD, Darby IA (2012) Hypoxia and hypoxia signaling in tissue repair and fibrosis. Int Rev Cell Mol Biol 296: 139-185.
- Vetuschi A, Pompili S, Gaudio E, Latella G, Sferra R (2018) PPAR-γ with its anti-inflammatory and anti-fibrotic action could be an effective therapeutic target in IBD. Eur Rev Med Pharmacol Sci 22(24): 8839-8848.
- Steen EH, Wang X, Balaji S, Butte MJ, Bollyky PL, et al. (2020) The Role of the Anti-Inflammatory Cytokine Interleukin-10 in Tissue Fibrosis. Adv Wound Care (New Rochelle) 9(4): 184-198.
- Medici D, Kalluri R (2012) Endothelial-mesenchymal transition and its contribution to the emergence of stem cell phenotype. Semin Cancer Biol 22(5-6): 379-384.
- Kong P, Christia P, Frangogiannis NG (2014) The pathogenesis of cardiac fibrosis. Cell Mol Life Sci 71(4): 549-574.
- Prakash J, Pinzani M (2017) Fibroblasts and extracellular matrix: Targeting and therapeutic tools in fibrosis and Adv Drug Deliv Rev 121: 1-2.
- Loganathan K, Salem Said E, Winterrowd E, Orebrand M, He L, et al. (2018) Angiopoietin-1 deficiency increases renal capillary rarefaction and tubulointerstitial fibrosis in mice. PLoS One 13(1):
- DiPietro LA (2016) Angiogenesis and wound repair: when enough is enough. J Leukoc Biol 100(5): 979-984.
- Ding BS, Cao Z, Lis R, Nolan DJ, Guo P, et al. (2014) Divergent angiocrine signals from vascular niche balance liver regeneration and fibrosis. Nature 505(7481): 97-102.
- Cao Z, Lis R, Ginsberg M, Chavez, D, Shido K, et al. (2016) Targeting of the pulmonary capillary vascular niche promotes lung alveolar repair and ameliorates fibrosis. Nat Med 22(2): 154-162.
- Kreuger J, Phillipson M (2016) Targeting vascular and leukocyte communication in angiogenesis, inflammation and fibrosis. Nat Rev Drug Discov 15(2): 125-142.
- Ai Y, Shi W, Zuo X, Sun X, Chen Y, et al. (2021) The Combination of Schisandrol B and Wedelolactone Synergistically Reverses Hepatic Fibrosis Via Modulating Multiple Signaling Pathways in Mice. Front Pharmacol 12: 655531.
- Wang X, Li X, Wang LN, Pan JJ, Yang X, et al. (2018) Buyang Huanwu Decoction Ameliorates Bleomycin-Induced Pulmonary Fibrosis in Rats via Downregulation of Related Protein and Gene Expression. Evid Based Complement Alternat Med 9185485.
- Niu WH, Wu F, Cao WY, Wu ZG, Chao YC, et al. (2021) Network pharmacology for the identification of phytochemicals in traditional Chinese medicine for COVID-19 that may regulate interleukin-6. Biosci Rep 41(1).
- Runfeng L, Yunlong H, Jicheng H, Weiqi P, Qinhai M, et al. (2020) Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2). Pharmacol Res 156:
- Takagaki Y, Lee SM, Dongqing Z, Kitada M, Kanasaki K, et al. (2020) Endothelial autophagy deficiency induces IL6 - dependent endothelial mesenchymal transition and organ fibrosis. Autophagy 16(10): 1905-1914.
- Liu W, Liu K, Zhang S, Shan L, Tang J (2018) Tetramethylpyrazine Showed Therapeutic Effects on Sepsis-Induced Acute Lung Injury in Rats by Inhibiting Endoplasmic Reticulum Stress Protein Kinase RNA-Like Endoplasmic Reticulum Kinase (PERK) Signaling-Induced Apoptosis of Pulmonary Microvascular Endothelial Cells. Med Sci Monit 24: 1225-1231.
- Cai X, Chen Z, Pan X, Xia L, Chen P, et al. (2014) Inhibition of angiogenesis, fibrosis and thrombosis by tetramethylpyrazine: mechanisms contributing to the SDF-1/CXCR4 axis. PLoS One 9(2): e88176.
- Li N, Wu K, Feng F, Wang L, Zhou X, et al. (2021) Astragaloside IV alleviates silica induced pulmonary fibrosis via inactivation of the TGF β1/Smad2/3 signaling pathway. Int J Mol Med 47(3): 16.
- Li P, Song J, Du H, Lu Y, Dong S, et al. (2021) MicroRNA-663 prevents monocrotaline-induced pulmonary arterial hypertension by targeting TGF-β1/smad2/3 signaling. J Mol Cell Cardiol 161: 9-22.
- Lv PY, Feng H, Huang WH, Tian YY, Wang, et al. (2017) Aucubin and its hydrolytic derivative attenuate activation of hepatic stellate cells via modulation of TGF-β Environ Toxicol Pharmacol 50: 234-239.
- Lin F, Liu YY, Xu B, Sun K, Wang HY, et al. (2013) Salvianolic acid B protects from pulmonary microcirculation disturbance induced by lipopolysaccharide in rat. Shock 39(3): 317-325.
- Liu Q, Shi X, Tang L, Xu W, Jiang S, et al. (2018) Salvianolic acid B attenuates experimental pulmonary inflammation by protecting endothelial cells against oxidative stress injury. Eur J Pharmacol 840: 9-19.
- Ma LQ, Pan CS, Yang N, Liu YY, Yan L, et al. (2014) Posttreatment with Ma-Xing-Shi-Gan-Tang, a Chinese medicine formula, ameliorates lipopolysaccharide-induced lung microvessel hyperpermeability and inflammatory reaction in rat. Microcirculation 21(7): 649-663.
- Sun K, Huang R, Yan L, Li DT, Liu YY, et al. (2018) Schisandrin Attenuates Lipopolysaccharide-Induced Lung Injury by Regulating TLR-4 and Akt/FoxO1 Signaling Pathways. Front Physiol 9:
- Zhang Q, Xiao X, Zheng J, Li M, Yu M, et al. (2020) Qishen Yiqi Dripping Pill Protects Against Diabetic Nephropathy by Inhibiting the Wnt/β-Catenin and Transforming Growth Factor-β/Smad Signaling Pathways in Rats. Front Physiol 11:
- Zhou L, Wei XH, Pan CS, Yan L, Gu YY, et al. (2017) Qi Shen YiQi Pills, a Compound Chinese Medicine, Prevented Cisplatin Induced Acute Kidney Injury via Regulating Mitochondrial Function. Front Physiol 8:
- Zhu R, Du XG, Yang SL, Wu YR, Liu JG (2019) Effect of Quyu Chencuo Formula on Renal Fibrosis in Obstructive Nephropathy Rats. Chin J Integr Med 25(3): 190-196.
- Du N, Liu S, Cui C, Hao F, Gao M, et al. (2020) Yishenhuoxue formula regulates TGF-β/Smad signal transduction to protect rats against Diabetic kidney disease injury. Pak J Pharm Sci 33(1): 21-26.
- Zhong J, Zhao N, Liu C, Hu J, Zhang W, et al. (2018) Research on the intervention of Yishen Huoxue prescription to renal fibrosis through the signal regulation by microRNA-126 to VEGF-Notch 12: 991-995.
- Wang DT, Huang RH, Cheng X, Zhang ZH, Yang YJ, et al. (2015) Tanshinone IIA attenuates renal fibrosis and inflammation via altering expression of TGF-β/Smad and NF-κB signaling pathway in 5/6 nephrectomized rats. Int Immunopharmacol 26(1): 4-12.
- Yang K, Fan B, Zhao Q, Ji Y, Liu P, et al. (2020) Hirudin Ameliorates Renal Interstitial Fibrosis via Regulating TGF-β1/Smad and NF-κB Signaling in UUO Rat Model. Evid Based Complement Alternat Med 2020:
- Du N, Xu Z, Gao M, Liu P, Sun B, et al. (2018) Combination of Ginsenoside Rg1 and Astragaloside IV reduces oxidative stress and inhibits TGF-β1/Smads signaling cascade on renal fibrosis in rats with diabetic nephropathy. Drug Des Devel Ther 12: 3517-3524.
- Huang WJ, Liu WJ, Xiao YH, Zheng HJ, Xiao Y, et al. (2020) Tripterygium and its extracts for diabetic nephropathy: Efficacy and pharmacological mechanisms. Biomed Pharmacother 121: 109599.
- Lu H, Wu L, Liu L, Ruan Q, Zhang X, et al. (2018) Quercetin ameliorates kidney injury and fibrosis by modulating M1/M2 macrophage polarization. Biochem Pharmacol 154: 203-212.
- Wang L, Cao AL, Chi YF, Ju ZC, Yin PH, et al. (2015) You-gui Pill ameliorates renal tubulointerstitial fibrosis via inhibition of TGF-β/Smad signaling pathway. J Ethnopharmacol 169: 229-238.
- Gao YH, Zhang Y, Li P, Liu HX, Li S, et al. (2016) [Anti-renal Fibrosis Mechanism of Modified Huangqi Chifeng Decoction Based on TGF-p1/Smad Signal Pathway]. Zhongguo Zhong Xi Yi Jie He Za Zhi 36(12): 1486-1490.
- Gautret P, Million M, Jarrot PA, Camoin Jau L, Colson P, et al. (2020) Natural history of COVID-19 and therapeutic options. Expert Rev Clin Immunol 16(12): 1159-1184.
- Zhao J, Wang L, Cao AL, Jiang MQ, Chen X, et al. (2016) HuangQi Decoction Ameliorates Renal Fibrosis via TGF-β/Smad Signaling Pathway In Vivo and In Vitro. Cell Physiol Biochem 38(5): 1761-1774.
- Han W, Ma Q, Liu Y, Wu W, Tu Y, et al. (2019) Huangkui capsule alleviates renal tubular epithelial-mesenchymal transition in diabetic nephropathy via inhibiting NLRP3 inflammasome activation and TLR4/NF-κB signaling. Phytomedicine 57: 203-214.
- Han X, Fan Y, Alwalid O, Li N, Jia X, et al. (2021) Six-month Follow-up Chest CT Findings after Severe COVID-19 Pneumonia. Radiology 299(1): E177-E186.
- Huang S, Zhu X, Huang W, He Y, Pang L, et al. (2017) Quercetin Inhibits Pulmonary Arterial Endothelial Cell Transdifferentiation Possibly by Akt and Erk1/2 Pathways. Biomed Res Int 2017: 6147294.
- Mao ZM, Wan YG, Sun W, Chen HL, Huang YR, et al. (2014) Effects and mechanisms of huangkui capsule ameliorating renal fibrosis in diabetic nephropathy rats via inhibiting oxidative stress and p38MAPK signaling pathway activity in kidney. Zhongguo Zhong Yao Za Zhi 39(21): 4110-4117.
- Piera Velazquez S, Mendoza FA, Jimenez SA (2016) Endothelial to Mesenchymal Transition (EndoMT) in the Pathogenesis of Human Fibrotic Diseases. J Clin Med 5(4): 45.
- Qin W, Cao L, Massey IY (2021) Role of PI3K/Akt signaling pathway in cardiac fibrosis. Mol Cell Biochem 476(11): 4045-4059.
- Yang N, Liu YY, Pan CS, Sun K, Wei XH, et al. (2014) Pretreatment with andrographolide pills® attenuates lipopolysaccharide-induced pulmonary microcirculatory disturbance and acute lung injury in rats. Microcirculation 21(8): 703-716.
- Zhang B, Lai L, Tan Y, Liang Q, Bai F, et al. (2020) Hepatoprotective effect of total flavonoids of Mallotus apelta (Lour.) Muell.Arg. leaf against carbon tetrachloride-induced liver fibrosis in rats via modulation of TGF-β1/Smad and NF-κB signaling pathways. J Ethnopharmacol 254:
- Zhang G, Yang G, Deng Y, Zhao X, Yang Y, et al. (2016) Ameliorative effects of Xue-Fu-Zhu-Yu decoction, Tian-Ma-Gou-Teng-Yin and Wen-Dan decoction on myocardial fibrosis in a hypertensive rat mode. BMC Complement Altern Med 16:
- Shen N, Li X, Zhou T, Bilal MU, Du N, et al. (2014) Shensong Yangxin Capsule prevents diabetic myocardial fibrosis by inhibiting TGF-β1/Smad signaling. J Ethnopharmacol 157: 161-170.
- Yang HJ, Kong B, Shuai W, Zhang JJ, Huang H (2020) Shensong Yangxin Protects Against Metabolic Syndrome-Induced Ventricular Arrhythmias by Inhibiting Electrical Remodeling. Front Pharmacol 11:
- Cheng W, Wang L, Yang T, Wu A, Wang B, et al. (2020) Qiliqiangxin Capsules Optimize Cardiac Metabolism Flexibility in Rats with Heart Failure After Myocardial Infarction. Front Physiol 11: 805.
- Liang T, Zhang Y, Yin S, Gan T, An T, et al. (2016) Cardio-protecteffect of qiliqiangxin capsule on left ventricular remodeling, dysfunction and apoptosis in heart failure rats after chronic myocardial infarction. Am J Transl Res 8(5): 2047-2058.
- Qi K, Li X, Geng Y, Cui H, Jin C, et al. (2018) Tongxinluo attenuates reperfusion injury in diabetic hearts by angiopoietin-like 4-mediated protection of endothelial barrier integrity via PPAR-α PLoS One 13(6): 0198403.
- Li Q, Chen Y, Zhao D, Wei Z, Zhang S, et al. (2018) NaoXinTong Capsule Inhibits Carrageenan-Induced Thrombosis in Mice. J Cardiovasc Pharmacol 72(1): 49-59.
- Zhu JZ, Bao XY, Zheng Q, Tong Q, Zhu PC, et al. (2019) Buyang Huanwu Decoction Exerts Cardioprotective Effects through Targeting Angiogenesis via Caveolin-1/VEGF Signaling Pathway in Mice with Acute Myocardial Infarction. Oxid Med Cell Longev 2019:
- Li X, Sun S, Chen D, Yuan T, Chen Y, et al. (2020) Puerarin attenuates the endothelial-mesenchymal transition induced by oxidative stress in human coronary artery endothelial cells through PI3K/AKT pathway. Eur J Pharmacol 886: 173472.
- Cai SA, Hou N, Zhao GJ, Liu XW, He YY, et al. (2018) Nrf2 Is a Key Regulator on Puerarin Preventing Cardiac Fibrosis and Upregulating Metabolic Enzymes UGT1A1 in Rats. Front Pharmacol 9: 540.
- Gao S, Li L, Li L, Ni J, Guo R, et al. (2019) Effects of the combination of tanshinone IIA and puerarin on cardiac function and inflammatory response in myocardial ischemia mice. J Mol Cell Cardiol 137: 59-70.
- Ma C, Fu Z, Guo H, Wei H, Zhao X, et al. (2019) The effects of Radix Angelica Sinensis and Radix Hedysari ultrafiltration extract on X-irradiation-induced myocardial fibrosis in rats. Biomed Pharmacother 112:
- Fang G, Chen S, Huang Q, Chen L, Liao D (2018) Curcumin suppresses cardiac fibroblasts activities by regulating the proliferation and cell cycle via the inhibition of the p38 MAPK/ERK signaling pathway. Mol Med Rep 18(2):1433-1438.
- Zhang J, Mao K, Gu Q, Wu X (2021) The Antiangiogenic Effect of Sanguinarine Chloride on Experimental Choroidal Neovacularization in Mice via Inhibiting Vascular Endothelial Growth Factor. Front Pharmacol 12:
- Wei XH, Liu YY, Li Q, Yan L, Hu BH, et al. (2013) Treatment with cardiotonic pills® after ischemia-reperfusion ameliorates myocardial fibrosis in rats. Microcirculation 20(1): 17-29.
- Cui YC, Yan L, Pan CS, Hu BH, Chang X, et al. (2018) The Contribution of Different Components in QiShenYiQi Pills® to Its Potential to Modulate Energy Metabolism in Protection of Ischemic Myocardial Injury. Front Physiol 9: 389.
- Li YC, Liu YY, Hu BH, Chang X, Fan JY, et al. (2012) Attenuating effect of post-treatment with QiShen YiQi Pills on myocardial fibrosis in rat cardiac hypertrophy. Clin Hemorheol Microcirc 51(3): 177-191.
- Zheng QN, Wei XH, Pan CS, Li Q, Liu YY, et al. (2019) QiShenYiQi Pills® ameliorates ischemia/reperfusion-induced myocardial fibrosis involving RP S19-mediated TGFβ1/Smads signaling pathway. Pharmacol Res 146:
- Chen LY, Pan CS, Wei XH, Li L, Han JY, et al. (2013) Sang-qi Granula Reduces Blood Pressure and Myocardial Fibrosis by Suppressing Inflammatory Responses Associated with the Peroxisome Proliferator-Activated Receptors and Nuclear Factor κ B Protein in Spontaneously Hypertensive Rats. Evid Based Complement Alternat Med 2013: 721729.
- Wang L, Yuan D, Zheng J, Wu X, Wang J, et al. (2019) Chikusetsu saponin IVa attenuates isoprenaline-induced myocardial fibrosis in mice through activation autophagy mediated by AMPK/mTOR/ULK1 signaling. Phytomedicine 58:
- Gracia Sancho J, Marrone G, Fernández Iglesias A (2019) Hepatic microcirculation and mechanisms of portal hypertension. Nat Rev Gastroenterol Hepatol 16(4): 221-234.
- Guixé Muntet S, Zhu CP, Xie WF, Gracia Sancho J (2020) Novel therapeutics for portal hypertension and fibrosis in chronic liver disease. Pharmacol Ther 215: 107626.
- Wang H, Che J, Cui K, Zhuang W, Li H, Sun J, et al. (2021) Schisantherin A ameliorates liver fibrosis through TGF-β1mediated activation of TAK1/MAPK and NF-κB pathways in vitro and in vivo. Phytomedicine 88:
- Cui LN, Zheng XH, Yu JH, Han Y (2021) [Role of CXCL12-CXCR4/CXCR7 signal axis in liver regeneration and liver fibrosis]. Zhonghua Gan Zang Bing Za Zhi 29(9): 900-903.
- Hu N, Guo C, Dai X, Wang C, Gong L, et al. (2020) Forsythiae Fructuse water extract attenuates liver fibrosis via TLR4/MyD88/NF-κB and TGF-β/smads signaling pathways. J Ethnopharmacol 262: 113275.
- Zhang Y, Miao H, Yan H, Sheng Y, Ji L (2018) Hepatoprotective effect of Forsythiae Fructus water extract against carbon tetrachloride-induced liver fibrosis in mice. J Ethnopharmacol 218: 27-34.
- Liu H, Dong F, Li G, Niu M, Zhang C, et al. (2018) Liuweiwuling tablets attenuate BDL-induced hepatic fibrosis via modulation of TGF-β/Smad and NF-κB signaling pathways. J Ethnopharmacol 210: 232-241.
- Liu H, Zhang Z, Hu H, Zhang C, Niu M, et al. (2018) Protective effects of Liuweiwuling tablets on carbon tetrachloride-induced hepatic fibrosis in rats. BMC Complement Altern Med 18(1):
- Xing X, Chen S, Li L, Cao Y, Chen L, et al. (2018) The Active Components of Fuzheng Huayu Formula and Their Potential Mechanism of Action in Inhibiting the Hepatic Stellate Cells Viability - A Network Pharmacology and Transcriptomics Approach. Front Pharmacol 9:
- Li XM, Peng JH, Sun ZL, Tian H, Duan XH, et al. (2016) Chinese medicine CGA formula ameliorates DMN-induced liver fibrosis in rats via inhibiting MMP2/9, TIMP1/2 and the TGF-β/Smad signaling pathways. Acta Pharmacol Sin 37(6): 783-793.
- Wang Z, Fei S, Suo C, Han Z, Tao J, et al. (2018) Antifibrotic Effects of Hepatocyte Growth Factor on Endothelial-to-Mesenchymal Transition via Transforming Growth Factor-Beta1 (TGF-β1)/Smad and Akt/mTOR/P70S6K Signaling Pathways. Ann Transplant 23: 1-10.
- Chen C, Yao X, Xu Y, Zhang Q, Wang H, et al. (2019) Dahuang Zhechong Pill suppresses colorectal cancer liver metastasis via ameliorating exosomal CCL2 primed pre-metastatic niche. J Ethnopharmacol 238: 111878.
- Liu F, Zhang J, Qian J, Wu G, Ma Z (2018) Emodin alleviates CCl4‑induced liver fibrosis by suppressing epithelial‑mesenchymal transition and transforming growth factor‑β1 in rats. Mol Med Rep 18(3): 3262-3270.
- Wu C, Chen W, Ding H, Li D, Wen G, et al. (2019) Salvianolic acid B exerts anti-liver fibrosis effects via inhibition of MAPK-mediated phospho-Smad2/3 at linker regions in vivo and in vitro. Life Sci 239:
- Zhang W, Ping J, Zhou Y, Chen G, Xu L (2019) Salvianolic Acid B Inhibits Activation of Human Primary Hepatic Stellate Cells Through Downregulation of the Myocyte Enhancer Factor 2 Signaling Pathway. Front Pharmacol 10:
- Li S, Zhao W, Tao Y, Liu C (2020) Fugan Wan alleviates hepatic fibrosis by inhibiting ACE/Ang II/AT-1R signaling pathway and enhancing ACE2/Ang 1-7/Mas signaling pathway in hepatic fibrosis rat models. Am J Transl Res 12(2): 592-601.
- Wu W, Piao H, Wu F, Han Y, An D, et al. (2019) Yu Jin Pulvis inhibits carbon tetrachloride-induced liver fibrosis by blocking the MAPK and PI3K/Akt signaling pathways. Am J Transl Res 11(9): 5998-6006.
- Liu C, Yuan X, Tao L, Cheng Z, Dai X, et al. (2015) Xia-Yu-Xue Decoction (XYXD) reduces Carbon Tetrachloride (CCl4)-induced liver fibrosis through inhibition hepatic stellate cell activation by targeting NF-κB and TGF-β1 signaling pathways. BMC Complement Altern Med 15:
- Miao H, Zhang Y, Huang Z, Lu B, Ji L (2019) Lonicera japonica Attenuates Carbon Tetrachloride-Induced Liver Fibrosis in Mice: Molecular Mechanisms of Action. Am J Chin Med 47(2): 351-367.
- Huang W, Li L, Tian X, Yan J, Yang X, et al. (2015) Astragalus and Paeoniae radix rubra extract inhibits liver fibrosis by modulating the transforming growth factor β/Smad pathway in rats. Mol Med Rep 11(2): 805-814.
- Song YN, Zhang GB, Lu YY, Chen QL, Yang L, et al. (2016) Huangqi decoction alleviates dimethylnitrosamine-induced liver fibrosis: An analysis of bile acids metabolic mechanism. J Ethnopharmacol 189: 148-156.
- Zhou Y, Tong X, Ren,S, Wang X, Chen J, et al. (2016) Synergistic anti-liver fibrosis actions of total astragalus saponins and glycyrrhizic acid via TGF-β1/Smads signaling pathway modulation. J Ethnopharmacol 190: 83-90.
- Kong Z, Liu R, Cheng Y (2019) Artesunate alleviates liver fibrosis by regulating ferroptosis signaling pathway. Biomed Pharmacother 109: 2043-2053.
- Li DT, Sun K, Huang P, Pan CS, Yan L, et al. (2019) Yiqifumai injection and its main ingredients attenuate lipopolysaccharide-induced cerebrovascular hyperpermeability through a multi-pathway mode. Microcirculation 26(7): e12553.
- Chen ZZ, Gong X, Guo Q, Zhao H, Wang L (2019) Bu Yang Huan Wu decoction prevents reperfusion injury following ischemic stroke in rats via inhibition of HIF-1 α, VEGF and promotion β-ENaC expression. J Ethnopharmacol 228: 70-81.
- Zhang ZQ, Song JY, Jia YQ, Zhang YK (2016) Buyanghuanwu decoction promotes angiogenesis after cerebral ischemia/reperfusion injury: mechanisms of brain tissue repair. Neural Regen Res 11(3): 435-440.
- Chen L, Wang X, Zhang J, Dang C, Liu G, et al. (2016) Tongxinluo Enhances Neurogenesis and Angiogenesis in Peri-Infarct Area and Subventricular Zone and Promotes Functional Recovery after Focal Cerebral Ischemic Infarction in Hypertensive Rats. Evid Based Complement Alternat Med 2016: 8549590.
- Liu S, Wei C, Kang N, He Q, Liang J, et al. (2018) Chinese medicine Tongxinluo capsule alleviates cerebral microcirculatory disturbances in ischemic stroke by modulating vascular endothelial function and inhibiting leukocyte-endothelial cell interactions in mice: A two-photon laser scanning microscopy study. Microcirculation 25(2): 12437.
- Liu Y, Tang Q, Shao S, Chen Y, Chen W, et al. (2017) Lyophilized Powder of Catalpol and Puerarin Protected Cerebral Vessels from Ischemia by Its Anti-apoptosis on Endothelial Cells. Int J Biol Sci 13(3): 327-338.
- Xue Q, Liu Y, He R, Yang S, Tong J, et al. (2016) Lyophilized Powder of Catalpol and Puerarin Protects Neurovascular Unit from Stroke. Int J Biol Sci 12(4): 367-380.
- Wu C, Chen J, Chen C, Wang W, Wen L, et al. (2015) Wnt/β-catenin coupled with HIF-1α/VEGF signaling pathways involved in galangin neurovascular unit protection from focal cerebral ischemia. Sci Rep 25(5):
- Huang P, Zhou CM, Qin H, Liu YY, Hu BH, et al. (2012) Cerebralcare Granule® attenuates blood-brain barrier disruption after middle cerebral artery occlusion in rats. Exp Neurol 237(2): 453-463.
- Sun K, Hu Q, Zhou CM, Xu XS, Wang, F, et al. (2010) Cerebralcare Granule, a Chinese herb compound preparation, improves cerebral microcirculatory disorder and hippocampal CA1 neuron injury in gerbils after ischemia-reperfusion. J Ethnopharmacol 130(2): 398-406.
- Wang F, Hu Q, Chen CH, Xu XS, Zhou CM, et al. (2012) The protective effect of Cerebralcare Granule® on brain edema, cerebral microcirculatory disturbance, and neuron injury in a focal cerebral ischemia rat model. Microcirculation 19(3): 260-272.
- Xu XS, Ma ZZ, Wang F, Hu BH, Wang CS, et al. (2009) The antioxidant Cerebralcare Granule attenuates cerebral microcirculatory disturbance during ischemia-reperfusion injury. Shock 32(2): 201-209.
- Chen B, Sun K, Liu YY, Xu XS, Wang CS, et al. (2016) Effect of salvianolic acid B on TNF-α induced cerebral microcirculatory changes in a micro-invasive mouse model. Chin J Traumatol 19(2): 85-93.
- Lu Y, Li Q, Liu YY, Sun K, Fan JY, et al. (2015) Inhibitory effect of caffeic acid on ADP-induced thrombus formation and platelet activation involves mitogen-activated protein kinases. Sci Rep 5:
- Tang H, Pan CS, Mao XW, Liu YY, Yan L, et al. (2014) Role of NADPH oxidase in total salvianolic acid injection attenuating ischemia-reperfusion impaired cerebral microcirculation and neurons: implication of AMPK/Akt/PKC. Microcirculation 21(7): 615-627.
- Li YJ, Han D, Xu XS, Liu YY, Sun K, et al. (2012) Protective effects of 3,4-dihydroxyphenyl lactic acid on lipopolysaccharide-induced cerebral microcirculatory disturbance in mice. Clin Hemorheol Microcirc 50(4): 267-278.
- Hao HF, Liu LM, Liu YY, Liu J, Yan L, et al. (2014) Inhibitory effect of rhynchophylline on contraction of cerebral arterioles to endothelin 1: role of rho kinase. J Ethnopharmacol 155(1): 147-153.
- Yan BY, Pan CS, Mao XW, Yang L, Liu, et al. (2014) Icariside II improves cerebral microcirculatory disturbance and alleviates hippocampal injury in gerbils after ischemia-reperfusion. Brain Res 1573: 63-73.
- Mao XW, Pan CS, Huang P, Liu YY, Wang CS, et al. (2015) Levo-tetrahydropalmatine attenuates mouse blood-brain barrier injury induced by focal cerebral ischemia and reperfusion: Involvement of Src kinase. Sci Rep 5:
- Chen QF, Liu YY, Pan CS, Fan JY, Yan L, et al. (2018) Angioedema and Hemorrhage After 4.5-Hour tPA (Tissue-Type Plasminogen Activator) Thrombolysis Ameliorated by T541 via Restoring Brain Microvascular Integrity. Stroke 49(9): 2211-2219.
- Chen FQ, Li Q, Pan CS, Liu YY, Yan L, et al. (2016) Kudiezi Injection (®) Alleviates Blood-Brain Barrier Disruption After Ischemia-Reperfusion in Rats. Microcirculation 23(6): 426-437.
- Gu YY, Huang P, Li Q, Liu YY, Liu G, et al. (2018) YangXue QingNao Wan and Silibinin Capsules, the Two Chinese Medicines, Attenuate Cognitive Impairment in Aged LDLR (+/-) Golden Syrian Hamsters Involving Protection of Blood Brain Barrier. Front Physiol 9: 658.
- Jiao YQ, Huang P, Yan L, Sun K, Pan CS, et al. (2019) YangXue QingNao Wan, a Compound Chinese Medicine, Attenuates Cerebrovascular Hyperpermeability and Neuron Injury in Spontaneously Hypertensive Rat: Effect and Mechanism. Front Physiol 10: 1246.
- Wang HM, Huang P, Li Q, Yan LL, Sun K, et al. (2019) Post-treatment With Qing-Ying-Tang, a Compound Chinese Medicine Relives Lipopolysaccharide-Induced Cerebral Microcirculation Disturbance in Mice. Front Physiol 10:
- Li Y, Li Q, Pan CS, Yan L, Hu BH, et al. (2018) Bushen Huoxue Attenuates Diabetes-Induced Cognitive Impairment by Improvement of Cerebral Microcirculation: Involvement of RhoA/ROCK/moesin and Src Signaling Pathways. Front Physiol 9: 527.
- Hiraishi K, Kurahara LH, Sumiyoshi M, Hu YP, Koga K, et al. (2018) Daikenchuto (Da-Jian-Zhong-Tang) ameliorates intestinal fibrosis by activating myofibroblast transient receptor potential ankyrin 1 channel. World J Gastroenterol 24(35): 4036-4053.
- Wu F, Shao Q, Hu M, Zhao Y, Dong R, et al. (2020) Wu-Mei-Wan ameliorates chronic colitis-associated intestinal fibrosis through inhibiting fibroblast activation. J Ethnopharmacol 252:
- Han L, Bian H, Ouyang J, Bi Y, Yang L, et al. (2016) Wenyang Huazhuo Tongluo formula, a Chinese herbal decoction, improves skin fibrosis by promoting apoptosis and inhibiting proliferation through down-regulation of survivin and cyclin D1 in systemic sclerosis. BMC Complement Altern Med 16: 69.
- Lin R, Lin J, Li S, Ding J, Wu H, et al. (2018) Effects of the traditional Chinese medicine baicalein on the viability of random pattern skin flaps in rats. Drug Des Devel Ther 12: 2267-2276.
- Li R, Yin H, Wang J, He D, Yan Q, et al. (2021) Dihydroartemisinin alleviates skin fibrosis and endothelial dysfunction in bleomycin-induced skin fibrosis models. Clin Rheumatol 40(10): 4269-4277.
- Liu Q, Lu J, Lin J, Tang Y, Pu W, et al. (2019) Salvianolic acid B attenuates experimental skin fibrosis of systemic sclerosis. Biomed Pharmacother 110: 546-553.
- Li M, Liu Q, He S, Kong X, Lin J, et al. (2021) Icaritin Inhibits Skin Fibrosis through Regulating AMPK and Wnt/β-catenin Signaling. Cell Biochem Biophys 79(2): 231-238.
- George PM, Wells AU, Jenkins RG (2020) Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir Med 8(8): 807-815.\
- Gong Z, Lin J, Zheng J, Wei L, Liu L, et al. (2020) Dahuang Zhechong pill attenuates CCl4-induced rat liver fibrosis via the PI3K-Akt signaling pathway. J Cell Biochem 121(2): 1431-1440.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.